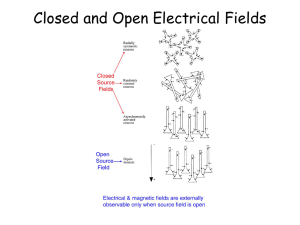
EEG
advertisement

Introduction to EEG for non-epileptologists working in seizure prediction and dynamics Richard Wennberg, MD, FRCPC University of Toronto IWSP4, Kansas City, 2009 1. EEG source • • • • cortical pyramidal cells voltage fluctuations in space/time summated EPSPs/IPSPs dependent on neural “synchrony” 2. EEG oscillations • Normal – (alpha, beta, mu, gamma, sleep spindles/delta) – generated in cortex – varying degrees of thalamocortical interdependence • Abnormal – (seizures, burst-suppression) 3. EEG sharp transients • Normal – Vertex sharp waves, positive occipital sharp transients of sleep (POSTS), benign epileptiform transients of sleep (BETS) or small sharp spikes; eye blinks, EKG, EMG • Abnormal – Epileptiform spikes, polyspikes, spike and waves, sharp waves, sharp and slow waves – Periodic complexes (lateralized and generalized), triphasic waves International (10-20) Electrode Placement Gloor, J Clin Neurophysiol, 1985 Gloor, J Clin Neurophysiol, 1985 Gloor, J Clin Neurophysiol, 1985 Pedley and Traub. In: Daly and Pedley, eds. Current Practice of Clinical EEG, 1990 Pedley and Traub. In: Daly and Pedley, eds. Current Practice of Clinical EEG, 1990 Steriade. In: Niedermeyer and Lopes da Silva, eds. Electroencephalography, 1993 EEG examples Subject awake, resting. Normal posterior alpha rhythm disappears with eye opening (*). High frequency activity at end of figure after eye opening is muscle artifact. Anterior-posterior bipolar montage. LFF 0.5 Hz, HFF 70 Hz, this and all other figures. Stage II sleep. K-complex (*); Sleep spindles (**). Anterior-posterior bipolar montage. Burst of generalized 3 Hz spike and wave activity (*). Primary generalized epilepsy. Anterior-posterior bipolar montage. Generalized, bilaterally synchronous, 3 Hz spike and wave activity in a different patient with primary generalized epilepsy. Referential montage; reference = linked ears. Primary generalized epilepsy: spike and wave bursts Juvenile myoclonic epilepsy Generalized, bilaterally synchronous bursts of spike and wave activity in another patient with primary generalized epilepsy, subtype juvenile myoclonic epilepsy. Referential montage; reference = linked ears. Primary generalized epilepsy: transition to tonic-clonic seizure Juvenile myoclonic epilepsy In this condition, bursts of spike and wave activity increase in frequency in the morning hours after awakening in a true “pre-ictal period” that may – or may not – result in a transition to a generalized tonic-clonic seizure. Primary generalized epilepsy: transition to tonic-clonic seizure High amplitude “hypersynchrony” Same seizure transition as previous figure, shown here at slower sweep speed. Bilateral temporal lobe (“focal”, “partial”) interictal epileptiform activity. Independent sharp and slow wave complexes over right (*) and left (**) anterior-mid temporal regions. Temporal lobe epilepsy. Anterior-posterior bipolar montage. Ictal EEG showing focal rhythmic seizure pattern localized to right temporal region (“equipotentiality” at F8-T4). Temporal lobe epilepsy. Anterior-posterior bipolar montage. Patient with bilateral hippocampal sclerosis, global developmental delay, medically-refractory complex partial seizures Interictal EEG during drowsiness in a different patient showing unilateral right anterior temporal lobe spikes (“phase reversing” at Zg2, F8, F10) Patient with bilateral hippocampal sclerosis, global developmental delay, medically-refractory complex partial seizures Ictal EEG showing unilateral right temporal lobe seizure (with “equipotentiality” at Zg2-T4, F8-T4, F10-T10) (note different sensitivity and time scale compared with preceding, interictal EEG figure from same patient) Artifacts Reference electrodes Why should the non-epileptologist care about artifacts and reference electrodes? Two examples – EEG studies of beta and gamma oscillations in cognition would appear to have been analyzing mainly muscle artifact • Whitham et al. Clin Neurophysiol 2008;119:1166-75 and Clin Neurophysiol 2007;118;1877-88 – The need for a reference electrode in EEG affects phase synchronization studies; resulting amplitude variations influence the phase locking analyses • Guevara et al. Neuroinformatics 2005;3:301-13 Eye blink, horizontal eye movements, frontalis and temporalis EMG, lateral rectus EMG, pulse artifacts. CZ-C3 C3-T3 T3-SP1 SP1-SP2 SP2-T4 T4-C4 C4-CZ EOG1-EOG2 FP1-F7 F7-T3 T3-T5 T5-O1 FP2-F8 F8-T4 T4-T6 T6-O2 FP1-F3 F3-C3 C3-P3 P3-O1 FP2-F4 F4-C4 C4-P4 P4-O2 EKG Comment Eye Blink C3 pulse artifact C3 pulse artifact C3 pulse artifact Eyes left Eyes right 100 uV 1 sec Combined circular and anterior-posterior bipolar montage. Eye blink, horizontal eye movements, frontalis and temporalis EMG, lateral rectus EMG, pulse artifacts. F7-Pz T3-Pz T5-Pz Fp1-Pz F3-Pz C3-Pz P3-Pz O1-Pz Fz-Pz Cz-Pz Pz-Pz Fp2-Pz F4-Pz C4-Pz P4-Pz O2-Pz F8-Pz T4-Pz T6-Pz Comment Eye Blink C3 pulse artifact C3 pulse artifact C3 pulse artifact Eyes left Eyes right 100 uV 1 sec Referential montage; reference = Pz. Eye blink, horizontal eye movements, frontalis and temporalis EMG, lateral rectus EMG, pulse artifacts. F7-Fz T3-Fz T5-Fz Fp1-Fz F3-Fz C3-Fz P3-Fz O1-Fz Fz-Fz Cz-Fz Pz-Fz Fp2-Fz F4-Fz C4-Fz P4-Fz O2-Fz F8-Fz T4-Fz T6-Fz Comment Eye Blink C3 pulse artifact C3 pulse artifact C3 pulse artifact Eyes left Eyes right 100 uV 1 sec Referential montage; reference = Fz. Eye blink, horizontal eye movements, frontalis and temporalis EMG, lateral rectus EMG, pulse artifacts. F7-C3 T3-C3 T5-C3 Fp1-C3 F3-C3 C3-C3 P3-C3 O1-C3 Fz-C3 Cz-C3 Pz-C3 Fp2-C3 F4-C3 C4-C3 P4-C3 O2-C3 F8-C3 T4-C3 T6-C3 Comment Eye Blink C3 pulse artifact C3 pulse artifact C3 pulse artifact Eyes left Eyes right 100 uV 1 sec Referential montage; reference = C3. Eye blink, horizontal eye movements, frontalis and temporalis EMG, lateral rectus EMG, pulse artifacts. F7-Av12 T3-Av12 T5-Av12 Fp1-Av12 F3-Av12 C3-Av12 P3-Av12 O1-Av12 Fz-Av12 Cz-Av12 Pz-Av12 Fp2-Av12 F4-Av12 C4-Av12 P4-Av12 O2-Av12 F8-Av12 T4-Av12 T6-Av12 Comment Eye Blink C3 pulse artifact C3 pulse artifact C3 pulse artifact Eyes left Eyes right 100 uV 1 sec Referential montage; reference = common average (of electrodes F3, F4, T3, C3, C4, T4, T5, P3, P4, T6, O1, O2). Eye blink, horizontal eye movements, frontalis and temporalis EMG, lateral rectus EMG, pulse artifacts. F7-aF7 T3-aT3 T5-aT5 Fp1-aFp1 F3-aF3 C3-aC3 P3-aP3 O1-aO1 FZ-aFz CZ-aCz PZ-aPz Fp2-aFp2 F4-aF4 C4-aC4 P4-aP4 O2-aO2 F8-aF8 T4-aT4 T6-aT6 Comment Eye Blink C3 pulse artifact C3 pulse artifact C3 pulse artifact Eyes left Eyes right 100 uV 1 sec Referential montage; reference = Laplacian. EEG cannot “see” deep into the brain Spontaneous activity in, e.g., mesial temporal regions, interhemispheric frontal lobe structures, thalamus is NOT apparent on scalp EEG Comparison of intracranial interictal epileptiform activity recorded during sleep with simultaneous scalp EEG. Focal spikes in left and right hippocampus (LH and RH), electrode contacts LHD1 and RHD1, show no scalp EEG correlates; more diffuse right temporal spike and wave complexes (RT) apparent at multiple contacts of right temporal depth electrode (RHD1-4) are associated with visible epileptiform potentials on scalp EEG (channels F8, T4). Referential montage; reference = common average 10-20 electrodes. Top 16 channels = scalp EEG. Channels 17-20 and 21-24 = left and right, respectively, temporal depth electrode recordings. Sensitivity = 15μV/mm for scalp EEG, 50 μV/mm for intracranial recordings. • Alarcón et al. JNNP 1994;57:435-49. – Scalp/FOE or depth/subdural or scalp/subdural/depth – Mesial temporal focal spike voltage gradient ~ 750μV/2.5mm – Estimated depth current dipole 2 nA·m would produce scalp voltage of 0.45μV – A typical 100μV scalp spike would require a mesial temporal focal dipole strength ~ 100-600 nA·m (an 80 mV hippocampal spike!) • Nayak et al. Clin Neurophysiol 2004;115:1423-35. – Scalp/FOE – Only 9% of temporal spikes seen intracranially visible on scalp w/o averaging * LHD1-Ref LHD2-Ref LHD3-Ref LHD4-Ref LAT1-Ref LAT2-Ref LAT3-Ref LAT4-Ref L.MT1-Ref LMT2-Ref LMT3-Ref LMT4-Ref LPT1-Ref LPT2-Ref LPT3-Ref LPT4-Ref RHD1-Ref RHD2-Ref RHD3-Ref RHD4-Ref RAT1-Ref RAT2-Ref RAT3-Ref RAT4-Ref RMT1-Ref RMT2-Ref RMT3-Ref RMT4-Ref RPT1-Ref RPT2-Ref RPT3-Ref 750 uV 1 sec RPT4-Ref * Comparison of intracranial ictal epileptiform activity recorded during sleep with simultaneous scalp EEG. Focal electrographic seizure in right hippocampus (rhythmic activity at intracranial depth electrode contact RHD1) has no scalp EEG correlate. Referential montage; reference = common average 10-20 electrodes. Top 16 channels = scalp EEG. Channels 17-20 and 21-24 = left and right, respectively, temporal depth electrode recordings. Sensitivity = 15μV/mm for scalp EEG, 50 μV/mm for intracranial recordings. Intracranial EEG (ECoG) Intracranial EEG of one mesial temporal lobe seizure (continuous recording from top left to bottom right). EEG recorded from a depth electrode contact situated within the right anterior hippocampus in a patient with medically-refractory temporal lobe epilepsy. Referential montage, scalp FCz reference. Temporal lobe epilepsy Left regional hippocampal/parahippocampal seizure onset (Intracranial depth electrode recording) Temporal lobe epilepsy Seizure “spread” to right mesial temporal region (Do seizures “spread” or “jump”?) An individual patient may have more than one morphology and/or localization of seizure onset Next seizures all from same patient, now seizure free >1 year after right anterior temporal lobe resection RHD1-Ref 750 uV 500 msec RHD1-Ref 750 uV 500 msec RHD1-Ref 750 uV 500 msec LHD1-Ref 750 uV 500 msec LHD1-Ref 750 uV 500 msec Five different seizure onsets recorded from intracranial depth electrodes in one patient over 24 hours RHD1-Ref 750 uV 500 msec RHD1-Ref 750 uV 500 msec RHD1-Ref 750 uV 500 msec LHD1-Ref 750 uV 500 msec LHD1-Ref 750 uV 500 msec …Continuation of the five seizures from previous figure LHD1-Ref LHD2-Ref LHD3-Ref LHD4-Ref LAT1-Ref LAT2-Ref LAT3-Ref LAT4-Ref L.MT1-Ref LMT2-Ref LMT3-Ref LMT4-Ref LPT1-Ref LPT2-Ref LPT3-Ref LPT4-Ref RHD1-Ref RHD2-Ref RHD3-Ref RHD4-Ref RAT1-Ref Focal onset Left Hippocampus RAT2-Ref RAT3-Ref RAT4-Ref RMT1-Ref RMT2-Ref RMT3-Ref RMT4-Ref RPT1-Ref RPT2-Ref RPT3-Ref RPT4-Ref Time LHD1-Ref LHD2-Ref LHD3-Ref LHD4-Ref LAT1-Ref LAT2-Ref LAT3-Ref LAT4-Ref L.MT1-Ref LMT2-Ref LMT3-Ref LMT4-Ref LPT1-Ref LPT2-Ref LPT3-Ref LPT4-Ref RHD1-Ref RHD2-Ref RHD3-Ref RHD4-Ref RAT1-Ref RAT2-Ref RAT3-Ref RAT4-Ref RMT1-Ref RMT2-Ref RMT3-Ref RMT4-Ref RPT1-Ref RPT2-Ref RPT3-Ref RPT4-Ref Time LHD1-Ref LHD2-Ref LHD3-Ref LHD4-Ref LAT1-Ref LAT2-Ref LAT3-Ref LAT4-Ref L.MT1-Ref LMT2-Ref LMT3-Ref LMT4-Ref LPT1-Ref LPT2-Ref LPT3-Ref LPT4-Ref RHD1-Ref RHD2-Ref RHD3-Ref RHD4-Ref RAT1-Ref Regional onset Left Hippocampus Parahippocampus RAT2-Ref RAT3-Ref RAT4-Ref RMT1-Ref RMT2-Ref RMT3-Ref RMT4-Ref RPT1-Ref RPT2-Ref RPT3-Ref RPT4-Ref Time LHD1-Ref LHD2-Ref LHD3-Ref LHD4-Ref LAT1-Ref LAT2-Ref LAT3-Ref LAT4-Ref L.MT1-Ref LMT2-Ref LMT3-Ref LMT4-Ref LPT1-Ref LPT2-Ref LPT3-Ref LPT4-Ref RHD1-Ref RHD2-Ref RHD3-Ref RHD4-Ref RAT1-Ref RAT2-Ref RAT3-Ref RAT4-Ref RMT1-Ref RMT2-Ref RMT3-Ref RMT4-Ref RPT1-Ref RPT2-Ref RPT3-Ref RPT4-Ref Time LHD1-Ref LHD2-Ref LHD3-Ref LHD4-Ref LAT1-Ref LAT2-Ref LAT3-Ref LAT4-Ref L.MT1-Ref LMT2-Ref LMT3-Ref LMT4-Ref LPT1-Ref LPT2-Ref LPT3-Ref LPT4-Ref RHD1-Ref RHD2-Ref RHD3-Ref RHD4-Ref RAT1-Ref Regional onset Right Uncus Hippocampus RAT2-Ref RAT3-Ref RAT4-Ref RMT1-Ref RMT2-Ref RMT3-Ref RMT4-Ref RPT1-Ref RPT2-Ref RPT3-Ref RPT4-Ref Time LHD1-Ref LHD2-Ref LHD3-Ref LHD4-Ref LAT1-Ref LAT2-Ref LAT3-Ref LAT4-Ref L.MT1-Ref LMT2-Ref LMT3-Ref LMT4-Ref LPT1-Ref LPT2-Ref LPT3-Ref LPT4-Ref RHD1-Ref RHD2-Ref RHD3-Ref RHD4-Ref RAT1-Ref RAT2-Ref RAT3-Ref RAT4-Ref RMT1-Ref RMT2-Ref RMT3-Ref RMT4-Ref RPT1-Ref RPT2-Ref RPT3-Ref RPT4-Ref Time LHD1-Ref LHD2-Ref LHD3-Ref LHD4-Ref LAT1-Ref LAT2-Ref LAT3-Ref LAT4-Ref L.MT1-Ref LMT2-Ref LMT3-Ref LMT4-Ref LPT1-Ref LPT2-Ref LPT3-Ref LPT4-Ref RHD1-Ref RHD2-Ref RHD3-Ref RHD4-Ref Regional onset Right Uncus Hippocampus “spread” to Generalized RAT1-Ref RAT2-Ref RAT3-Ref RAT4-Ref RMT1-Ref RMT2-Ref RMT3-Ref RMT4-Ref RPT1-Ref RPT2-Ref RPT3-Ref RPT4-Ref Time LHD1-Ref LHD2-Ref LHD3-Ref LHD4-Ref LAT1-Ref LAT2-Ref LAT3-Ref LAT4-Ref L.MT1-Ref LMT2-Ref LMT3-Ref LMT4-Ref LPT1-Ref LPT2-Ref LPT3-Ref LPT4-Ref RHD1-Ref RHD2-Ref RHD3-Ref RHD4-Ref RAT1-Ref RAT2-Ref RAT3-Ref RAT4-Ref RMT1-Ref RMT2-Ref RMT3-Ref RMT4-Ref RPT1-Ref RPT2-Ref RPT3-Ref RPT4-Ref Time Intraoperative ECoG Pre-resection ECoG in a patient with right temporal lobe epilepsy, hippocampal sclerosis and a posterior middle temporal gyrus gliotic lesion. C1-4 inferior temporal gyrus, C4 anterior. C5-8 middle temporal gyrus, C8 anterior. C11-14 superior temporal gyrus; C1, C5 over lesion, C11 superior to lesion. C14-17 above Sylvian fissure. Propofol bolus given 3 minutes earlier with maximal activation of inferior temporal spikes. ECoG 2 min after bolus of alfentanil: activation of amygdala/hippocampal spikes and suppression of temporal neocortical spikes ECoG 10 min later: return to pre-activation baseline of amygdala/hippocampal spikes and reappearance of independent temporal neocortical spikes