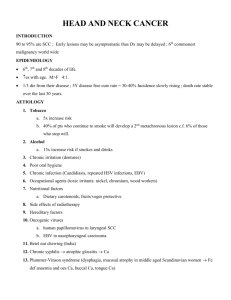
4412 Head and Neck Cancer
advertisement

Head and Neck Cancer Radiation Therapy 4412 Management of Head and Neck Cancer Through multidisciplinary treatment we try to: 1. decrease deformity 2. maintain the reduction of the tumor 3. restore function 4. preserve the structure and esthetics 5. cure the cancer 1. Compare and contrast the epidemiologic factors prevalent in head and neck cancers 1/3 of patients that are treated have early stage 2/3 of patients will have locally advanced stages Lungs are the most common site for mets The nerve routes are important in treatment planning, tumors can spread this way Almost half of all squamous cell ca occur in the oral cavity Head and neck cancer involves the upper aerodigestive tract. Oral cavity Pharynx Paranasal sinuses Larynx Thyroid gland Salivary glands Men- usually 50-60 years old Can occur in people younger than 40 years of age More women are smoking Smokeless tobacco Recurrences- usually within first 2 years Rarely after 4 years Most 5 year survivors will be alive at 10 years 2. List and describe the etiologic factors associated with head and neck cancers Smokeless tobacco- squamous cell of cheek and gum Previous radiation exposure- thyroid /salivary glands Poor oral hygiene Ill fitting dentures/irritation to tissues Wood mill workers- nasal cavity/paranasal sinuses Lip cancer- UV exposure, unfiltered cigarettes Viruses Epstein Barr virus Herpes simplex (cold sores) HPV- oral/larynx Chronic abuse of marijuana- degree of risk unknown Diet Vitamin A and E deficiency Plummer-Vinson syndrome- iron deficiency anemia Alcohol Pharyngeal and laryngeal cancer Liver damage Secondary nutritional deficiencies Alcohol damages mucosa and makes it more permeable Impurities in the alcoholic beverages Smoking Head and neck cancers occur 6x more frequently than non-smokers Unfiltered cigarettes Cigar smoking is a risk Laryngeal cancer mortality increases as the number of cigarettes smoked increases Smoking, tobacco, alcohol: a deadly combination! Alcohol is synergistic to tobacco- cooperate together to produce a total effect greater than the sum of the individual elements Tars Aromatic hydrocarbons Ethanol suppresses the efficiency of DNA repair Nitrosamines most noncombustible product in snuff and chewing tobacco Pre-cancerous signs: Leukoplakia is a precancerous, slowly developing change in the mucous membrane. They are characterized by thickened, white, firmly attached patches that are slightly raised. Erythroplasia- A premalignant lesion that is shiny, velvety and reddish in color These are severe dysplastic changes and should be taken seriously Leukoplakia 3. Identify the prognostic indicators in head and neck cancers Prognosis decreases as: The affected area progresses backward from the lips to the hypopharynx (excludes larynx) Lesions that cross the midline Exhibits endophytic growth- invades within the lamina propria and submucosa Have cranial nerve involvement Fixed nodes Fixed lesion in the anatomic compartments Are poorly differentiated Nonsquamous cell 5. Compare and contrast endophytic and exophytic tumor features of head and neck cancers *Endophytic growth- growth pattern that invades the lamina propria and submucosa -more aggressive and harder to control locally *Exophytic- a noninvasive neoplasm that projects out from an epithelial surface -characterized by raised, elevated borders *Most head and neck cancers are infiltrative lesions found in the epithelial lining Staging Lymphatics of the head and neck are in direct correlation to the prognosis 1/3 of the body’s lymphatics are in the head and neck area Staging depends on: Site of primary disease Extent of primary disease Size of primary tumor Staging cont’d Cell type and differentiation Lymphatic vascular space invasion of the tumor The nodal status 6. List and describe the different types of head and neck cancers Most head and neck cancers will infiltrate into the epithelial lining of the upper digestive tract 80% of all head and neck cancers will be squamous cell 7. Compare and describe the different types of head and neck cancers. 8. Describe the different treatment considerations for the different types of head and neck cancers. Oral Cavity Oral cavity extends from the skin vermilion junction of the lip to the posterior border of the hard palate superiorly And the circumvallate papillae inferiorly Anterior 2/3 of the tongue lips, buccal mucosa, lower alveolar ridge, upper alveolar ridge, retromolar trigone, floor of the mouth, and hard palate Page 694 Washington/Leaver Oral cavity cancers The most common aerodigestive tract cancers Occur mostly in men- 55 to 65 years old Alcohol and tobacco are synergistic Patients usually have poor oral and dental hygiene Plummer-Vinson syndrome is important etiologic factor General practitioner or dentist will find the cancer Early diagnosis is important Leukoplakia and erythroplasia are serious Most oral cavity cancers will be nonhealing ulcers with little pain Localized pain is an advanced disease The cancer is usually raised, centrally ulcerated, indurated edges and the base is infiltrating Mandatory biopsy Squamous cell carcinoma makes up 90%95% Well or moderately well differentiated Has the lowest incidence (except glottic) of nodal mets Cervical node involvement=advanced disease Lips and Gum Lip cancer is treated with radiation the same way as skin cancer Usually involves the lower lip and spreads by direct invasion Carcinoma in-situ and early lesions of the lip may be surgically removed Radiation Therapy: Portal should include primary lesion with a 2 cm A shield (stent) of lead and bolus material (to absorb backscatter) is placed under the lip This blocks the alveolar process and gums Treated with external beam, interstitial implant or both 100 SSD, 100% isodose line Lip Cancer Floor of Mouth Floor of the mouth lesions usually arise on the anterior surface on either side of the midline. They can spread to bone and tongue Approx 30% of these cancers will involve the submaxillary and subdigastric nodes Opposed lateral fields are used The tip of the tongue can be elevated out of the portal with a cork or a bite block and tongue depressor Bite blocks can also spare the roof of the mouth from incidental irradiation If the lesion has grown into the tongue, the tongue is flattened to reduce the superior border of the portal Radiation therapy: supraclavicular and bilateral neck fields, followed with a boost of intraoral cone, needle implants, or small external photon beams Tongue The anterior 2/3 of the tongue is included in the oral cavity The base of the tongue is considered oropharynx Small tumors in the anterior 2/3 of the oral tongue are usually resected Radiation therapy is used for inoperable patients Post-op radiation therapy Treats the primary site Treats the cervical lymph nodes And margins positive for tumor, extensive primary tumor with bone or skin invasion, and multiple positive nodes The anterior tongue drains into the Submandibular lymph nodes The posterior portion of the tongue drains into the Jugulodigastric Posterior pharyngeal Upper cervical lymph nodes Lesions of the tongue usually appear on the lateral borders near the middle and posterior third section A limited number of tongue cancers can be excised Most are controlled with external beam and interstitial boost fields Lesions at the base and posterior 1/3 of the tongue invade The floor of the mouth Tonsils or the muscles Are advanced Have a higher incidence of nodal mets Hemiglossectomy- surgical removal of half the tongue. It is used for treatment of an early stage lesion of the tongue Radiation therapy- three field technique Utilizes external beam, electron beam Possibly an iridium implant and neck dissection Isocentric lateral opposed fields Lower anterior neck field Fields include subdigastric and submaxillary nodes Upper cervical nodes T1 Squamous cell of tongue Buccal Mucosa Buccal mucosa is the mucous membrane lining the inner surface of the cheeks and lips Most lesions arise on the lateral walls Have a history of leukoplakia Are raised, exophytic growths Lesion invades the skin and bone First sign is a bump on the tip of the tongue No pain associated at first until the nerves to the tongue or ear become involved Advanced lesions will bleed Stensen’s duct (parotid duct) can become obstructed The parotid gland becomes enlarged Small lesions are surgically removed Large lesions are treated with surgery and radiation therapy or Radiation therapy alone Complications- fibrosis of the cheek and trismus Hard Palate Located between the upper alveolar ridge and mucous membrane covering the palatine process of the maxillary palatine bones Mostly adenocarcinomas and rare Spread to the bone, invade the maxillary antrum Treatment- surgical resection, post-op radiation therapy History of ill fitting dentures or trauma Retromolar Trigone Triangular space behind the last molar tooth Rare carcinomas Symptoms- tongue, ear canal pain, trismus Usually moderately differentiated squamous cell carcinoma Lymphatic spread to the submaxillary & subdigastric nodes Treated with radiation therapy PHARYNX Subdivided into three anatomic divisions: Oropharynx Nasopharynx hypopharynx Common symptoms Persistant sore throat Painful swallowing Referred otalgia Cervical node enlargement Fetor oris, dyspnea, dysphasia, hoarseness, dysarthria, hypersalivation indicates advanced disease Diagnosis- indirect mirror exam, palpation, biopsy, CT, MRI Histopathology- squamous cell carcinomas Staging- AJCC Classification Mets- cervical lymph nodes (bilateral), retropharyngeal nodes, lung Oropharynx Consists of the base of the tongue, the tonsils (fossa and pillars), soft palate, oropharyngeal walls The oropharynx is located between the axis and C3 vertebral bodies Soft tissue regions- anterior tonsillary pillars, soft palate, uvula, base of the tongue and the lateral-posterior pharyngeal walls Tonsils are the most common site for disease Symptoms- sore throat and pain during swallowing Upper spinal accessory nodes are involved bilaterally in 50% to 70% of the patients Radiation therapy is treatment of choice Cancer of tongue Hypopharynx Pyriform sinuses, postcricoid, and lower posterior pharyngeal walls below the base of the tongue It is situated between C3 to C6 The cricoid cartilage is the inferior border Epiglottis is the superior border Hypopharyngeal cancer is advanced High rate of nodal mets Tumor is highly infiltrative The highest area for incidence is the pyriform sinus Radical surgery and radiation therapy is the treatment of choice Rouviere’s (lateral retropharyngeal) lymph nodes at the base of the skull are included with other nodal groups in treatment (page 706, Washington) Tonsillar, pharyngeal wall and posterior cricoid are treated using radiation therapy (page 709, figure 30-28, Washington) Unresectible T4 pyriform sinus tumor, surrounding carotid artery Nasopharynx Posterosuperior pharyngeal wall and lateral pharyngeal wall, the eustachian tube orifice and adenoids The nasopharynx is a cuboidal structure lying on a line from the zygomatic arch to the external auditory meatus (EAM), extending inferiorly to the mastoid tip The nasopharynx lies behind the nasal cavities and above the level of the soft palate The nasal cavity drains into the nsopharynx via the two posterior nares Two eustachian tubes are on the lateral walls which connect to the middle ear Nasopharyngeal disease can mimic an inflammatory process Can cause considerable respiratory or auditory dysfunction The cranial nerve is frequently involved The ninth to the twelfth cranial nerves can be affected Enlargement of the retropharyngeal nodes Can affect the external carotid artery A lesion can invade directly into the third cranial nerve Commonly involves the sixth cranial nerve When cranial nerves are involved, this means the disease is advanced and widespread Histology- squamous cell Nasopharyngeal cancer is usually poorly differentiated and shows an unusual growth pattern This disease is not associated with tobacco consumption NPC is associated with the Epstein Barr virus Can occur in adolescence and young adults Occurs again between 50 and 70 years of age Uncommon in white populations Found mostly in southern China and the Middle East Positive cervical nodes in 75% to 85% of NPC patients About half of all cases will have bilateral or contralateral disease Radiation ports are large The lateral retropharyngeal (node of Rouviere) which cannot be surgically removed, and jugulodigastric nodes are almost always treated Primary lesion is small but the nodal disease is extensive Bone and lung common mets sites NPC spreads to adjacent sites and has a high recurrence rate Aggressive, large volume curative radiation therapy is given Larynx The larynx is contiguous with the lower portion of the pharynx above and is connected with the trachea below. It extends from the tip of the epiglottis at the level of the lower border of the C3 vertebra to the lower border of the cricoid cartilage at the level of C6 There are 3 main parts to the larynx. These parts are: The supraglottis - the area above the vocal cords that contains the epiglottis cartilage The glottis - the area around the vocal cords The subglottis - the part below the vocal cords, containing the cricoid cartilage. It continues down into the windpipe Glottic cancer- 65% Supraglottic cancer- 25% to 33% Subglottic- make up the rest of the cases Most common cancer in the aerodigestive tract is the larynx Male dominated disease 50-60 years of age Smoking high risk factor Extensive use of voice in occupation is risk factor (singers, auctioneer) for laryngeal cancer Alcohol high risk factor for supraglottic cancer Cancer of the glottis (true vocal cord) is not life threatening Choice of treatment is based on the preservation of speech and airway Laryngeal cancer shows a mutation of the p53 gene Classic Symptoms- persistent sore throat and hoarseness Cervical lymph nodes involvement is associated with supraglottic lesions Carcinoma in situ is common on the vocal cords Glottic lesions are well to moderately differentiated Supraglottic lesions are less differentiated and more aggressive Glottic lesions will appear of the anterior 2/3 of one cord (approx 65%-75%) Cord mobility is a factor in the classification of lesions Treatment- radiation therapy is the treatment of choice for nonfixed surface glottic lesions that have not invaded muscle, bone or cartilage Glottic cancer is treated with lateral opposing fields 5X5cm or 6X6 cm Large, fixed lesions will require aggressive treatment Radiation therapy offers the best voice preservation Supraglottic lesions are usually large and bulky They do not usually invade the inferior false cord or the ventricles These lesions usually spread superiorly to the epiglottis Lymph nodes are usually involved in 40%50% of the patients Subglottic lesions are treated with total laryngectomy with Post-op radiation therapy Larynx- squamous cell, Rt anterior vocal fold Salivary Glands Salivary glands are made up of: Parotid-largest gland, located superficial to and partly behind the ramus of the mandible, and covers the masseter muscle It fills the space between the ramus of the mandible and the anterior border of the sternocleidomastoid muscle Contains extensive lymphatic capillary plexus many aggregates of lymphocytic cells Numerous intraglandular lymph nodes in the superficial lobe Submandibular glands Sublingual glands Tumors of the salivary gland are rare The parotid is the most common site for tumors Nearly 2/3 of these tumors will be benign Low-dose ionizing radiation in childhood may have been a risk factor Dental x-rays have been implicated for both benign and malignant tumors Most major and minor salivary gland cancers are of unknown origin Adenoid cystic, mucoepidermoid, and adenocarcinoma are the most common cell types Symptoms- asymptomatic parotid mass lasting 4-8 months before the tumor arises Presenting symptoms- localized swelling and pain, facial palsy, & rapid growth Facial nerve involvement suggests malignancy Diagnosis is done through lobectomy Treatment- Although most tumors are benign, local recurrence is high Total resection with margins sparing facial nerves Radiation therapy- post-op for residual, recurrent or inoperable tumors Accelerated fractionation- provides similar dose levels of radiation therapy in a shorter amount of overall time. This counteracts quick cellular proliferation of aggressive tumors by giving more dose in a shorter period of time. Maxillary Sinus Maxillary sinus is a pyramid shaped cavity lined by ciliated epithelium and bound by thin bone or membranous partitions. Carcinomas arising from the ciliated epithelium or mucous glands perforate the bony walls almost from the beginning Tumors will also involve the superior portion of the sinus and extend into the floor of the orbit Maxillary sinus cancers- 80% of all sinus cancers Long history of sinusitis, nasal obstructions and bloody discharge Squamous cell carcinomas Invade the floor of the orbit, ethmoid sinuses, hard palate & zygomatic arch Displacement of the eye is common Nasal cavity and paranasal sinus tumors are often associated with cranial nerve palsies- trigeminal branches CT and MRI are the most useful studies Submandibular node will be the first involved, although cervical node spread is uncommon Treatment- Surgery is the treatment of choice Primary radiation therapy has a chance of optic nerve damage from the high dose required for tumor control Surgery and radiation therapy used in most cases Lateral and anterior ports are used When the orbit is involved, eye blocking will not be used Care should be taken to miss the cord and contralateral lens Angling the anterior beam a few degrees off the vertical spares brain tissue Nasal cavity risk- Bolus material will be inserted to improve dose homogeneity Angling the lateral port a few degrees off the horizontal plane spares the contralateral optic nerve and lens Management of the Head and Neck Patient Washington, Page 718, Table 30-3, dosetissue response schedule Page 719, Box 30-11, recommended skin care program Care of the head and neck patient Peridontal disease and caries Nutrition Mucositis/stomatitis Xerostomia Cataract formation Lacrimal glands Taste changes Skin reactions