Fertility Preservation in Gynaecological Oncology - erc
advertisement

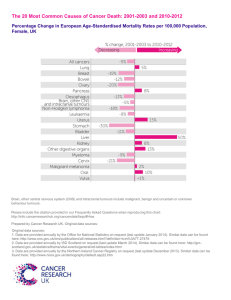
Conservative Surgery to Preserve Fertility in Gynaecological Cancers. Sean Kehoe Oxford Gynaecological Cancer Centre Churchill Hospital Oxford Malignancies Cervical Endometrial Ovarian Vulval Cancer ? Counselling Counselling is very important Often we are deviating from what could be considered the ‘Standard Recommendations’ In essence – experimentation with the patient taking the risk. Cervical Carcinoma Occurs not uncommonly in younger patients [33% < 40 years] A real increase in adenocarcinomas An impression of more cases occurring in nulliparous women – probably due to women delaying pregnancies as compared to previous times. Figure 1.1: Numbers of new cases and age specific incidence rates, cervical cancer, UK 2004 20 85+ 80-84 75-79 70-74 65-69 60-64 55-59 50-54 45-49 40-44 0 35-39 0 30-34 5 25-29 100 20-24 10 15-19 200 10-14 15 5-9 300 0-4 Number of cases Female cases Female rates Rate per 100,000 population 400 Age at diagnosis About 33% of cervical carcinomas occur in women <40 years Cervical Carcinoma Severe Dyskaryosis ? Invasion ? Invasion on Colposcopy Requires some form of biopsy Stage 1A1 – Squamous Carcinoma A loop cone excision of the cervix is sufficient treatment Once all pre-invasive and invasive disease cleared. Stage 1A1 Adenocarcinoma Problem with ‘definition’ Now staging as 1A1 is acceptable Skip lesions can occur : ? Just Pre-invasive For lesions 3 -5 mm x 7 mm, 141 women – only 1 case of lymph node disease [0.73%] Cervical Cancer: Trachelectomy Rules Nulliparous [?] – family incomplete Careful clinical staging MRI scan to evaluate tumour extent. Ib1 [2cms] or less. Adenocarcinomas ? ? Poorly Differentiated ?Lymph Vascular Space Invasion Trachelectomy Excise to Isthmus Insert Cervical Circlage Cervical Cancer Cervical Circlage Parametrial Tissue But will surgery be further modified? Why parametrial tissue which addresses only 2 of 4 planes ? In tumour <10mm invasion and <2cms diameter – incidence of parametrial involvement is estimates at 0.6% Cervical Cancer Single or 2 stage procedure ? If single – depending on Frozen Section Histology Extra-peritoneal or Intra-peritoneal Lymphadenectomy? If the procedure is about preserving fertility – it seems logical to prevent intra-peritoneal surgery when an alternative is available. Patients and tumor characteristics for the seven clinical studies of radical vaginal trachelectomy Beiner ME and Covens A (2007) Surgery Insight: radical vaginal trachelectomy as a method of fertility preservation for cervical cancer Nat Clin Pract Oncol 4: 353–361 doi:10.1038/ncponc0822 Table 2 Operative data and complications in the seven clinical studies of radical vaginal trachelectomy Beiner ME and Covens A (2007) Surgery Insight: radical vaginal trachelectomy as a method of fertility preservation for cervical cancer Nat Clin Pract Oncol 4: 353–361 doi:10.1038/ncponc0822 Table 7 Number of obstetric outcomes in patients who underwent trachelectomy Beiner ME and Covens A (2007) Surgery Insight: radical vaginal trachelectomy as a method of fertility preservation for cervical cancer Nat Clin Pract Oncol 4: 353–361 doi:10.1038/ncponc0822 Counselling Pregnancy: If achieved – 30% miscarriage rate Assume – Premature delivery Assume – Operative Delivery Recurrence Rates To date the recurrence rates at about 4% are not in excess of that expected with a radical hysterectomy. The application of this procedure to large tumours is less frequent now. How Safe: Trachelectomy? Case selection very important Probably as safe as Radical Procedures Avoid in Large tumours [>2cms ?] Avoid in rare/high risk tumours For nulliparous women only? ENDOMETRIAL CANCER Endometrial Cancer A Rare issue in women where fertility is a factor. Histopathology Imaging Both of these are paramount in decision making. Endometrial Cancer Histology: Differentiation between Atypical Hyperplasia and Frank Carcinoma Remember – when tissue confirms Atypical Hyperplasia – Frank Malignancy is found in the Hysterectomy specimen in 40-50% of cases [Cancer 2006,GOG study] Most would agree that fertility preservation should be limited to those with well differentiated tumours [stage 1A] Endometrial Cancer Imaging: This is important for the ‘staging’ process. CT/MTI/Ultrasound? Kinkel et al,Radiology 1999: Metaanalysis Contrast enhanced MRI best – BUT of note myometrial invasion detected correctly in 90% of cases – i.e. 10% false negative rate. Endometrial Cancer In the main – progestagens used as therapy. Treatment time to regression ranges from 3.5 – 9 months Recurrence occurs in about 20% of responders This approach requires careful surveillance – and repeated endometrial curettage. Endometrial Cancer How to manage?? Mirena IUCD Progestogens: GnRH analogues All the above have been used with reasonable success [responses about 70%]. Tamoxifen can increase the PR, and hence potentially enhance the efficacy of progestagenic agents Endometrial Cancer Stage 1a Treatment Curettage at 3/12 Curettage at 6/12 If Attempt pregnancy If + Offer Hysterectomy Intervene If Any concerns Endometrial Cancer Ref Cases Response Pregnancies Kaku 2001 12 75% 2 Imai 2001 15 50% 2 Randall 1997 14 75% ? Gotlieb 2003 13 100% 9 babies Signorelli, 2009 21 57% 13 pregnancies Laurelli 2011 14 90% 1 baby Miniq, 2011 14 57% 11 pregnancies Endometrial Cancer Ushijima et al. J. Clinical Oncology 2007 28 Stage 1 A, 17 Atypical hyperplasia, all < 40 years 600mgs MPA with low dose aspirin Continued for 28 weeks once responding Endometrium checked 8 and 16 weeks CR 55% Endometrial CA, and 82% AH In responders– either oestrogen/progesterone therapy or Fertility therapy. 36 months follow-up – 12 pregnancies and 7 deliveries However 47% recurrence rate – need careful monitoring Distribution of clinicopathological characteristics in the endometrial cancer patients with conception in the meta-analysis Characteristics Patients no. Group 1 Group 2 p Age at diagnosis, yr (mean SD) Age at pregnancy, yr (mean SD) Histology type Adenocarcinoma Adenosquamous Grade of differentiation Well Moderate and poor Hysterectomy after childbearing Yes No Metastasis/recurrence Yes No 50 43 45 44 1 41 38 3 50 9 41 50 4 46 32.8 , 4.1 (n = 14) 34.3, 4.0 (n = 13) 14 14 0 14 13 1 14 3 11 14 0 14 29.5, 5.3 (n = 36) 30.9 , 5.3 (n = 30) 31 30 1 27 25 2 36 6 30 36 4 32 Taiwan J Obstet Gynecol. 2011 Mar;50(1):62-6. Obstetric outcomes of pregnancy after conservative treatment of endometrial cancer: case series and literature review. Chao AS, Chao A, Wang CJ, Lai CH, Wang HS 0.05 0.05 1.0 1.0 0.70 0.57 author platform+m yes Analyses of obstetric outcomes according to undergoing: IVF, ICSI, gamete intrafallopian transfer, or zygote intrafallopian transfer (Group 1) and spontaneous conception/intrauterine insemination (Group 2) Preterm labor Cesarean rate Primigravida Multiple pregnancy Group 1 (n=15) Group 2 (n=50) p 7 (46.7) 14 (93.3) 14 (93.3) 6 (40.0) 3 (6.0) 11 (22.0) 36 (72.0) 0.160 3 (6.0) 0.003 0.001 <0.001 Taiwan J Obstet Gynecol. 2011 Mar;50(1):62-6. Obstetric outcomes of pregnancy after conservative treatment of endometrial cancer: case series and literature review. Chao AS, Chao A, Wang CJ, Lai CH, Wang HS How safe : Endometrial cancer? Numbers are too small to make any dogmatic statements. We can preserve fertility After single delivery – most recommend hysterectomy. Ovarian Cancer Agreed fertility preservation in all young patients [?<40 years]- as: 1. Germ cell tumours very chemosensitive 2. Borderline tumours – normally cured with local excision [ if early stage] 3. If advanced ovarian cancer – then can always re-operate. 4. May be another condition – eg Hodgkins !! Invasive Early stage disease Schilder et al, Gynecol Oncol, 2002 N = 52 42 stage 1A Grade 1 = 35 Grade 2= 9 10 stage 1C Grade 3 = 5 20 had adjuvant chemotherapy 5 recurrences [8-78 months after first surgery] Sites : Contralateral ovary – 3 , peritoneum 1 and lung 1. 2 deaths 24 attempted pregnancies – 71% conceived. Survival at 5 years 98% and 10 years 93% Fertility-sparing surgery in young women with mucinous adenocarcinoma of the ovary. Gynecol Oncol. 2011 Aug;122(2):334-8. Kajiyama H et al,Japan N=148,The median follow-up time of all mEOC patients was 71.6 (4.8-448.3) months 41 patients with Fertility Sparing, 27 = Stage 1a, 14 Stage 1c 5 year overall survival was 97.3% Compared with 101 women who underwent Radical surgery for the Same disease – there was no difference in outcome. Germ Cell Tumours Ref Cases Chemo Preg Survival Perrin 1999 45 29 7 babies 2 deaths Sagae 2003 26 23 4 pregnancies – no deaths Zanetta 2001 138 81 40 babies 95% 5 year For Germ cell tumours – outcome excellent. Most problems were in the more advanced stage diseases. Fertility can be retained. Borderline Ovarian Tumours Ref Cases Recurrence Pregnancies Gotlieb, 2003 39 8% 22 in 15 women Zanetta,2001 189 18% 41in 21 women Demeter, 2002 12 ? 50% Donnez,2003 16 18.7% 64% Boran 2004 62 6.5% 13 in 10 women Rao , 2005 38 16% 6 in 5 women Ovarian Cancer What if Cystectomy performed ? A. If malignant – proceed to oophorectomy and full staging B. If borderline – oophorectomy – reduces recurrence rates Ovarian Cancer Must Monitor the Contra-lateral ovary. Ultrasound/tumour markers. Borderline Ovarian Cancer Boran 2005 Fertility Sparing 62 Radical 80 Recurrence 6.5% vs 0.0% Zanetta 2001 189* 150 18.5 % vs 4.6% • 7 cases progressed to ‘invasive’ carcinoma Important to counsel the patient and is this evidence to support routine pelvic clearance after completion of the family ?? Ovarian Cancer Fertility conservation safe for Borderline tumours. In invasive tumours – probably best to restrict fertility preservation surgery to properly staged, Stage 1 disease. Following completion of family – pelvic clearance seems a logical approach to reduce recurrences, and considering the limitations of screening such women. Conclusions Yes it can be done – but always the question is :Should it be done? Need the full Multidisciplinary Team – Oncological and Fertility Working together. [?Obstetric/Neonatal?] Counsell– Counsell and Counsell A Healthy Mother and Child