Neuronal intranuclear hyaline inclusion disease
advertisement

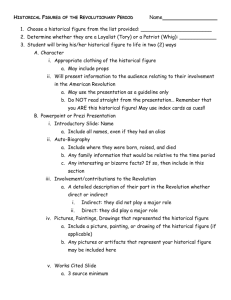
American Association of Neuropathologists: 2011 Diagnostic Slide Session 2011-8 Jeremy Deisch, M.D. Dennis Burns, M.D. Charles White III, M.D. History • 21-year-old female; developmental history normal until… – Age 10 years: tremors and headaches – Age 12 years: dysarthric speech – Age 15 years: muscle biopsy demonstrated chronic neurogenic atrophy; temporal instability, tongue fasiculations, progressive dysarthria, tremors, and cognitive decline were noted – Age 18 years: Bilateral deep brain stimulator placement with temporary alleviation of tremors – Clinical condition progressed to disabling dyskinesia, severe dysphagia, and inability to walk or stand History • Family History: – Maternal great grandmother with tremors, onset in the 7th decade – Maternal grandfather with tremors, onset in the 6th decade – Maternal aunt with mental retardation – Both parents report seizures in past • Because of repeated complications and in agreement between the patient and her family, the gastric feeding tube was removed; death followed shortly thereafter 1150 grams Substantia nigra Substantia nigra Frontal lobe Diagnostic immunostains were performed… Subthalamic nucleus Dentate nucleus Cerebellar cortex Spinal cord, anterior horn Ubiquitin; frontal lobe Ubiquitin; frontal lobe Summary… • Ubiquitin-immunoreactive neuronal intranuclear hyaline inclusions noted in all levels of the neuroaxis – – – – – – Neocortex Basal ganglia Diencephalon Brainstem Cerebellum Spinal cord (anterior horn) • Rare glial, endothelial inclusions noted Diagnosis • Neuronal Intranuclear Hyaline Inclusion Disease (NIHID) – First described in 1980 by Joo Ho Sung et al, University of Minnesota – 21-year-old female patient with neuronal intranuclear inclusions in nearly all neuroanatomic locales (central, peripheral, and autonomic nervous system) – Electron microscopy: inclusions comprised haphazardly-arranged fine filaments measuring 8 to 9 nm NIHID • Approximately 30 cases described in the literature • Slowly-progressive, multiple-system neurodegenerative condition defined pathologically by the finding of eosinophilic, hyaline intranuclear inclusions in neurons in diverse neuroanatomic locations • Heterogenous clinical and pathologic characteristics – – – – Age of onset ranges from 2 to 72 years (mean 22.8 years) M:F ratio = 1.08 Variable presence of glial intranuclear inclusions Variable presentation with personality disturbances, cognitive decline, pyramidal and extrapyramidal motor symptoms, autonomic disturbances NIHID- Categorization • J. Takahashi-Fujigasaki, 2003; Proposed dividing cases into three categories • Infantile form- onset prior to age 5 years, clinical course < 10 years; ataxia, dysarthria, and tremor predominate • Juvenile form- characterized by personality change, pyramidal and extrapyramidal motor disturbances, and cerebellar disturbances; clinical course > 10 years • Adult form- cognitive disturbances predominate; clinical course highly variable (1-14 years). Glial inclusions predominate • Familial cases reported, including examples in identical twins 1C2 (polyglutamine); frontal lobe Polyglutamine and NIHID • Similar to NIHID, CAG repeat expansion disorders (Huntington, DRPLA, SCA1-7) show pathologic neuronal intranuclear inclusions. • Rare neurons in NIHID show 1C2 (polyglutamine) immunoreactive inclusions described by multiple authors – No CAG repeat expansion documented in any known susceptible genes – Some have hypothesized that polyglutamine expansion is occurring in a yet undiscovered gene. – Wild-type ataxin 1, ataxin 2, ataxin 3, and TBP have been demonstrated in NIIs. – Vast minority of nuclear inclusions are 1C2 immunoreactive. Differential Diagnosis • Neuronal intranuclear inclusions – Poliomyelitis – rare, minute – Marinesco bodies – Small ( < nucleolus), SN, LC – Ferritinopathy – Mutation in ferritin light-chain gene gene, similar presentation, granular intranuclear, iron-reactive inclusions primarily in Fe the basal ganglia – Polyglutamine repeat expansion disorders – intranuclear inclusions are typically sparse, tend not to be visible on routine sections. Differential Diagnosis • Fragile-X Dementia-Parkinson Syndrome (FXDPS); Yachnis et al, 2010 – 58-year-old female with rapidly-progressive nonfluent dementia and Parkinsonism • Fragile-X carrier; two sons with fragile-X, one normal daughter • Diffuse, symmetric white-matter attenuation • Astrocytes/glia with prominent ubiquitinimmunoreactive intranuclear inclusions in neocortex, hippocampi, deep gray, cerebellum, and brainstem NIHID- Antemortem Diagnosis • Sone et al, 2011 • 7 patients with NIHID • 27 patients with other neurologic d/o • 8 normal volunteers • 7/7 patients showed ubiquitinimmunoreactive inclusions in adipocytes, sweat glands, and fibroblasts • No samples from patients with other neurologic disorders or normal control patients showed intranuclear inclusions Questions?