Bariatric Surgery for the Treatment of Obesity
advertisement
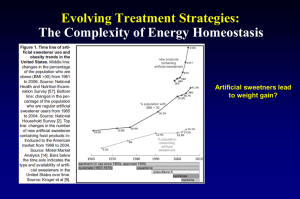
Bariatric Surgery Roberto C. Mirasol, MD, FPCP, FPSEM Obesity and Weight Management Center St. Luke’s Medical Center Bariatric Surgery • Indications 1. BMI >40 kg/m2 or BMI 35–39.9 kg/m2 and life-threatening cardiopulmonary disease, severe diabetes, or lifestyle impairment 2. Failure to achieve adequate weight loss with nonsurgical treatment • Contraindications 1. History of noncompliance with medical care 2. Certain psychiatric illnesses: personality disorder, uncontrolled depression, suicidal ideation, substance abuse 3. Unlikely to survive surgery NIH Consensus Development Panel. Ann Intern Med 1991;115:956. CLINICAL PRACTICE RECOMMENDATIONS, 2009 ADA • Bariatric surgery should be considered for adults with BMI 35 kg/m2 and type 2 diabetes, especially if the diabetes is difficult to control with lifestyle and pharmacologic therapy. (B) • Patients with type 2 diabetes who have undergone bariatric surgery need life-long lifestyle support and medical monitoring. (E) Bariatric Surgery Stats 1995 the number of bariatric surgeries performed was well over 20000 2003 - 103,000 2004 - 144,000 Average age of patient – 30 years old Length of Hospital Stay – 3.9 days Bariatric surgeons – increased by 500% Complication rate – 10% Deaths <1% CDC, 2006 Current Bariatric Surgical Procedures Classification Procedure Gastric restriction • Adjustable Gastric Banding Primarily restrictive and partially malabsorptive • Roux-en-Y Gastric Bypass Primarily malabsorptive and partially restrictive Biliopancreatic diversion with duodenal switch Biliopancreatic diversion Distal gastric bypass Gastric Bypass Procedure A small (10–30 mL) gastric pouch is anastomosed to a Roux limb of jejunum. Increasing the length of the Roux limb increases malabsorption and weight loss. Long-term Effect of Gastric Bypass Surgery on Body Weight Weight Loss (% of Excess Weight) 0 20 40 60 80 100 0 2 BMI (kg/m2): 50 Poiries et al. Ann Surg 1995;222:339. 4 6 8 10 Years After Surgery 34 35 12 14 35 Randomized, Controlled Trial Comparing Open With Laparoscopic Gastric Bypass • Both procedures had – Similar weight loss – Similar incidence of anastomotic leaks – Equivalent costs • Laparoscopic procedure had – Less wound complications (infection and hernia) – Increased late anastomotic strictures – Less blood loss – Shorter hospital stay – Faster recovery – Faster improvement in quality-of-life Nguyen et al. Ann Surg 2001;234:279. Weight Loss With Gastric Bypass Procedure vs. Vertical Banded Gastroplasty Decrease in Excess Weight (%) 90 70 Gastric bypass 50 Vertical banded gastroplasty 30 10 0 6 12 18 24 Time (months) Sugerman et al. Ann Surg 1987;205:613. 30 36 Laparoscopic Adjustable Gastric Banding LapBandTM Access port (reservoir) Gastric Band Connection tubing Silicone band placed around upper stomach to create a small pouch. Outlet diameter can be changed by infusing or withdrawing saline from port. American Society for Metabolic and Bariatric Surgery, www.asbs.org LAP BAND Laparoscopic Adjustable Gastric Banding Produces Greater Weight Loss than Comprehensive Medical Therapy* in Patients with Class I Obesity (BMI 30-35 kg/m2) 0 Weight Loss, % -5 -10 -15 -20 Surgical -25 -30 Nonsurgical Baseline 6 mo 12 mo *(VLCD, behavioral modification, and pharmacotherapy) Obrien et al. Ann Intern Med. 2006;144:625-33 18 mo 24 mo Biliopancreatic Diversion With Duodenal Switch Sleeve gastrectomy with rerouting of small intestine through “nutrient limb” and “biliopancreatic limb.” Digestion and absorption are limited to 100 cm “common channel” of terminal ileum. Causes marked weight loss, but can lead to significant nutritional deficiencies. Marceau P. et al. World J Surg 1998;22:947-54. Effect of Different Bariatric Surgical Procedures on Weight Loss Procedure Approximate Loss of Excess Weight (%) Laparoscopic gastric banding 45–65 Gastric bypass procedure 55–65 Biliopancreatic diversion with duodenal switch 60–75 Klein et al. Gastroenterology. 2002;123:882-932 Incidence of Gallstone Formation (% subjects/wk) Relationship Between Rate of Weight Loss and Gallstone Formation 3 2 Data reported from individual studies 1 0 0 1 0.5 1.5 Rate of Weight Loss (kg/wk) Weinsier et al. Am J Med 1995;98:115. 2 2.5 Complications of Bariatric Surgery All procedures: • • • • • • • • • Atelectasis and pneumonia Deep vein thrombosis Pulmonary embolism Wound infection Gastrointestinal bleeding Gallstones Failure to lose weight Intractable vomiting/kwashiorkor (B1) Mortality (0.1%–2%) Gastric bypass: • • • • • • • Anastomotic leak with peritonitis Stomal stenosis Marginal ulcers Staple line disruption Nutrient deficiencies (iron, calcium, folic acid, vitamin B12) Dumping syndrome Small bowel obstruction – Internal hernia – Adhesions Gastric banding procedure: • • • • • • Band slippage Band erosion Esophageal dilatation Band or port infections Port disconnection Port displacement Biliopancreatic diversion: • • • • • • Anastomotic leak with peritonitis Protein-calorie malnutrition Calcium, iron, folic acid, fat soluble vitamin (A,D,E,K) deficiencies Dehydration Steatorrhea Small bowel obstruction – Internal hernia – Adhesions Relationship Between Surgical Experience and Perioperative Mortality in Gastric Bypass Surgery 7% Thirty Day Mortality 6% 5% 125 case lifetime bariatric surgery experience 4% 3% 2% 1% 0% 0 50 100 150 200 250 300 350 400 450 500 550 600 650 Chronological case order per surgeon D Flum et al. J Am Coll Surg 199:543, 2004 Patients with Normal Fasting Blood Glucose and HbA1c After Surgery (%) Gastric Bypass Surgery Improves Glycemic Control in Impaired Glucose Tolerance or Type 2 Diabetes 100 75 50 25 0 Patents with Type 2 Diabetes Pories et al. Ann Surg 1995;222:339. Patients with IGT Incidence of Type 2 Diabetes (% Patients) Prevention of Type 2 Diabetes at 8 Years After Bariatric Surgery (94% Restrictive) 20.0 16.0 Control Bariatric surgery 18.5 12.0 8.0 4.7 3.6 4.0 0.0 0.0 2 8 Follow-up After Surgery (y) Control Initial BMI (kg/m2) 41 5 Weight change at year 8: 1 11% Sjostrom et al. Hypertension 2000;36:20. Surgery 41 4 -16 12% Ratio of Recovery (% of subjects) Effect of Bariatric Surgery on Obesity-related Metabolic Complications 100 Control Surgery 72 80 62 60 46 36 34 40 21 13 21 19 22 24 11 20 0 2 yr 10 yr Diabetes Sjöström: N Engl J Med 2004;351:2683. 2 yr 10 yr Hypertension 2 yr 10 yr Hypertriglyceridemia (Brunt et al. system) Histology score Effect of Gastric Bypass Surgery-induced Weight Loss on Liver Histology 3 Before GBS 1 Yr after GBS 2 1 0 Steatosis Inflammation Klein S. et al. Gastroenterology 130:1564, 2006 Fibrosis Long-term Survival: Canada 7 Rel. Risk = 0.11 (.04-.27) % Mortality 6 89% reduction in risk of death over 5 years 5 4 3 2 1 0 Control Christou et al. Ann Surg 2004;240:416-424 Bariatric Surgery Major Obesity-related Comorbidities That Have Been Improved by Bariatric Surgery • • • • • • • • Type 2 diabetes Hypertension Obstructive sleep apnea Obesity hypoventilation GERD NALD, NASH Pseudotumor cerebri Depression • • • • • • • • • Dyslipidemias Coronary artery disease Cardiac dysfunction Venous stasis disease Polycystic ovary syndrome Infertility Cancers Degenerative joint disease Quality of life GLP-1 and GIP Are the Two Major Incretins GLP-1 GIP • Produced by L cells mainly located in the distal gut (ileum and colon) • Stimulates glucose-dependent insulin release Other effects • Suppresses hepatic glucose output by inhibiting glucagon secretion in a glucose-dependent manner • Inhibition of gastric emptying; reduction of food intake and body weight • Enhances beta-cell proliferation and survival in animal models and isolated human islets • Produced by K cells in the proximal gut (duodenum) • Stimulates glucose-dependent insulin release • Minimal effects on gastric emptying; no significant effects on satiety or body weight • Potentially enhances beta-cell proliferation and survival in islet cell lines GLP-1=glucagon-like peptide-1; GIP=glucose-dependent insulinotropic polypeptide. Drucker DJ. Diabetes Care. 2003;26:2929–2940; Ahrén B. Curr Diab Rep. 2003;3:365–372; Drucker DJ. Gastroenterology. 2002;122: 531–544; Farilla L et al. Endocrinology. 2003;144:5149–5158; Trümper A et al. Mol Endocrinol. 2001;15:1559–1570; Trümper A et al. J Endocrinol. 2002;174:233–246; Wideman RD et al. Horm Metab Res. 2004;36:782–786. Nonincretin Gut Peptides • Peptide YY (PYY) – Secreted by the L cells of the distal intestine – Present in 2 molecular forms: PYY(1-36) and PYY (3-36), a cleavage product – PYY increases satiety and delays gastric emptying through neuropeptide Y-receptor subtypes in the central and peripheral nervous system – IV PYY(3-36) increases satiety and decreases food intake in humans Nonincretin Gut Peptides • GHRELIN – Secreted by gastric fundus and proximal small intestine and acts on the hypothalamus to regulate appetite – Inhibits insulin secretion by a paracrine mechanism – Systemic ghrelin levels increase before a meal and decrease afterward – Ghrelin stimulates appetite and food intake and suppresses energy expenditure and fat catabolism – Inversely proportional to body weight – Weight loss increases ghrelin levels suggests that ghrelin affects long term regulation of body weight PROPOSED MECHANISMS FOR IMPROVED GLYCEMIC CONTROL AFTER BARIATRIC SURGERY Effects of Decreased Caloric Intake on Fasting Glycemia • Decreased caloric intake affects glucose metabolism • Rate of diabetes remission are not the same – Complete remission within days of intestinal bypass procedures (Porries, 1995) – Takes months to occur in LAGB (Dixon, 2008) RUBINO EXPERIMENTS • Goto- Kakizaki Rats- non obese animal model for diabetes DJB (duodenal-jejunal bypass) – less fasting and postprandial hyperglycemia than control Weight loss by caloric restriction – glycemic control did not improve HINDGUT HYPOTHESIS (LOWER INTESTINAL HYPOTHESIS) • Intestinal rearrangement speeds the delivery of nutrients to the distal intestines • Causes exaggerated GLP-1 and PYY levels and improves glucose tolerance and insulin secretion Cummings, et al, 2007 FOREGUT EXCLUSION THEORY (UPPER INTESTINAL HYPOTHESIS) Bypassing gut prevents the secretion of a “putative signal” that promotes insulin resistance and Type 2 DM. • Stomach sparing DJB vs Gastrojejunostomy (leaves nutrient flow in the proximal intestine intact) • Bypass of proximal gut prevents secretion “Anti-incretin factor” or “decretin” • May be implicated in the pathogenesis of diabetes Gut Peptide Response to Different Bariatric Surgical Procedures* HORMONE Cell Type (Location) Effect on Insulin Secretion BPD RYGB LAGB Ghrelin X/A cells Stomach Decrease Increase Increase/ Decrease Increase/ No Change GIP K cells duodenum Increase Decrease Decrease No change GLP-1 L cells Distal ileum Increase Increase Increase No change Peptide YY L cells Distal ileum Decrease Increase Increase No change *Folli, 2007 BARIATRIC SURGERY IN ST LUKE’S PATIENT PROFILE* MALE FEMALE TOTAL 18 (36%) 32 (64%) 50 14-18 1 (6%) 1(3%) 2 (4%) 19-59 15 (83%) 30 (94%) 45 (90%) >60 2 (11%) 1 (3%) 3 (6%) 14-18 57 46.8 51.9 19-59 47.07 46.15 46.5 >60 39.45 39 39.3 7 (39%) 10 (31%) 17 (34%) 4 (22%) 12 (38%) 16 (32%) 7(39) 10(21%) 17 (34%) Number (%) Age group BMI (mean) Obesity Types Obese (30-40) Morbidly obese (40-50) Super obese *Dineros, Obesity Surgery, 2007 Weight Reduction in ALL Patients* Postoperative Period Initial Weight (kg+ SD) Weight Loss (kg + SD) % Excess Weight Loss BMI (kg / m2) Start 126.7+ 25.4 0 0.00 48.0+ 11.7 1 month 115.9 + 19.4 10.7 + 6.4 8.50% 43.2 + 9.2 3 months 113.2 + 21.4 13.4 + 6.4* 10.60% 42.3 + 9.9 6 months 93.5 + 24.7 33.1+ 10.9* 26.10% 33.7 + 7.1 9 months 91.4 + 20.8 35.3 +10.4* 27.90% 32.4 + 8.7 12 months 68.6+ 10.8 38.3 +11.9* 31.00% 27.5 + 3.1 Dineros, Obesity Surgery, 2007 COMPLICATIONS • Early Complications • • • • • Wound infection 2/50 Pneumonia 1/50 Dehydration 1/50 Gastritis 1/50 Leakage 1/50 COMPLICATIONS • Late Complications • Band Slippage 2/20 (10%) • Stomal Stenosis 1/20 (5%) • Ventral Hernia 1/5 (20%) STARTING WEIGHT: 307 lbs; BMI 49.44 END WEIGHT: 156 lbs; BMI 25.16 STARTING WEIGHT: 516 lbs; BMI 83.10 END WEIGHT: 258 lbs; BMI 37.01 100 kg (220 lb) 76 kg (168 lb) BYPASS on Non- obese • 2 mildly overweight • Duodenal bypass lowered fasting insulin, fasting glucose, and HgbA1c within 1 month after surgery Diabetes Surgery Summit, Rome, 2007