Isolation Precautions 2013
advertisement
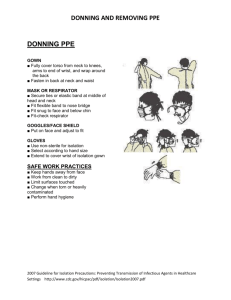
Hand Washing and Isolation Precautions Healthcare Associated Infections (HAIs) in the USA Today • HAIs affect 5-10% of patients in US acute care hospitals. • HAIs affect nearly 2 million patients per year. • HAIs cost an estimated $5-10 Billion per year. • More than 70% of bacteria that cause HAIs are resistant to at least one of the drugs most commonly used to treat the infections. HAIs – The Human Cost • 99,000 people will DIE this year from a HAI. • It’s equivalent to a 747 plane crash killing all passengers and crew every other day. • It’s one death every 6 minutes. • IT IS PREVENTABLE! Desired Goals • Reduce hospital acquired infections • Thereby reducing avoidable morbidity, mortality and cost. Key Factors: • Hand hygiene • Environmental decontamination • Identification and isolation of colonized patients • Education Contaminated Surfaces tested positive for VRE (+) in patient environment. Hayden M. ICAAC,2001, Chicago, IL Hand Hygiene • Hand hygiene is the single most important means of preventing the spread of infection. • It is to be performed before and after every patient encounter, and after the removal of gloves. Wash Hands Access the CDC Hand Washing Course go to: http://www.cdc.gov/handhygiene/training/int eractiveEducation/ Personal Stethoscopes • Personal stethoscopes should be cleaned before and after each use. An EPA registered hospital disinfectant (disinfecting surface wipes) or alcohol wipes may be used Personal Protective Equipment • Gowns, gloves, masks, goggles, face shields, PAPRs • Available on the nursing units • Gloves should be in every patient room • Types of PPE required for each isolation category are identified on a sign posted on the door to the patient room. Key Points About PPE • Don before contact with the patient, generally before entering the room • Use carefully – don’t spread contamination • Remove and discard carefully, either at the doorway or immediately outside patient room; remove respirator outside room • Immediately perform hand hygiene Sequence* for Donning PPE 1. Gown first 2. Mask or respirator 3. Goggles or face shield 4. Gloves * Combination of PPE will affect sequence – be practical How to Don a Gown • Select appropriate type and size • Opening is in the back • Secure at neck and waist • If gown is too small, use two gowns – Gown #1 ties in front – Gown #2 ties in back How to Don a Mask • Place over nose, mouth and chin • Fit flexible nose piece over nose bridge • Secure on head with ties or elastic • Adjust to fit How to Don a Particulate Respirator • Select a fit tested respirator • Place over nose, mouth and chin • Fit flexible nose piece over nose bridge • Secure on head with elastic • Adjust to fit • Perform a fit check – – Inhale – respirator should collapse – Exhale – check for leakage around face How to Don Eye and Face Protection • Position goggles over eyes and secure to the head using the ear pieces or headband • Position face shield over face and secure on brow with headband • Adjust to fit comfortably How to Don Gloves • Don gloves last • Select correct type and size • Insert hands into gloves • Extend gloves over isolation gown cuffs “Contaminated” and “Clean” Areas of PPE • Contaminated – outside front • Areas of PPE that have or are likely to have been in contact with body sites, materials, or environmental surfaces where the infectious organism may reside • Clean – inside, outside back, ties on head and back • Areas of PPE that are not likely to have been in contact with the infectious organism Sequence for Removing PPE 1. Gloves 2. Face shield or goggles 3. Gown 4. Mask or respirator Where to Remove PPE • At doorway, before leaving patient room or in anteroom • Remove respirator outside room, after door has been closed How to Remove Gloves • Grasp outside edge near wrist • Peel away from hand, turning glove insideout • Hold in opposite gloved hand How to Remove Gloves • Slide ungloved finger under the wrist of the remaining glove • Peel off from inside, creating a bag for both gloves • Discard Remove Goggles or Face Shield • Grasp ear or head pieces with ungloved hands • Lift away from face • Place in designated receptacle for reprocessing or disposal Removing Isolation Gown • Unfasten ties • Peel gown away from neck and shoulder • Turn contaminated outside toward the inside • Fold or roll into a bundle • Discard Removing a Mask • Untie the bottom, then the top • Remove from face • Discard Removing a Particulate Respirator • Lift the bottom elastic over your head first • Then lift off the top elastic • Discard Hand Hygiene • Perform hand hygiene immediately after removing PPE. – If hands become visibly contaminated during PPE removal, wash hands before continuing to remove PPE • Wash hands with soap and water or use an alcohol-based hand rub Protect Yourself and Your Patient • PPE is available to protect you from exposure to infectious agents in the healthcare workplace • Know what type of PPE is necessary for the duties you perform and use it correctly Donning and Removal of PPE Video Review Click on the link below. http://www.siumed.edu/common/videoplay er.php?f=mp4:oec/Student/PPE.f4v CDC Guideline for Isolation Precautions • There are 4 isolation categories - The name of each reflects how the infectious organism/disease is transmitted. • The next few slides will detail the requirements of each category and show examples of the signs posted on patient doors to communicate these requirements to all who enter. 4 CDC Categories • Standard • Contact • Airborne • Droplet STANDARD PRECAUTIONS • Assume that every person is potentially infected or colonized with an organism that could be transmitted in the healthcare setting. • Wear PPE according to the level of anticipated contamination, when handling patient-care equipment and instruments/devices that are visibly soiled or may have been in contact with blood or body fluids. CONTACT ISOLATION Protects from diseases spread by contact. Including: Clostridium difficile (C-Diff) Scabies, lice, impetigo Patients with multiple drug resistant organisms (MDRO) like MRSA, VRE, and MDRO gram negative organisms (i.e.Pseudomonas, Acinetobacter). •Private room required •Gown required •Gloves required Contact Isolation: Patient transport: Patient: Patient wears clean gown. Cover any open wounds. Cover patient with clean sheet prior to transport. HCW: (Healthcare Worker) Wear Personal protective equipment (PPE) when touching patient. Remove and dispose of PPE and perform hand hygiene prior to transporting patient. Don clean PPE to handle patient at transport destination. Visitors: Visitors who are not providing direct care to patients in contact precautions will not need to wear gown and gloves. This does not apply to students, residents or other healthcare providers. Equipment: Clean glucometers, thermometers or any other equipment used for or on a patient. Dedicate stethoscope, B/P cuff to each patient. For patients with spore-forming organisms, such as Clostridium difficile (C. diff), you must wash hands with soap and water. Alcohol-based hand cleaners are less effective. Memorial Medical Center ONLY AIRBORNE PRECAUTIONS Protects from disease spread by air/respiratory tract. • Primarily used for suspected or diagnosed TB. • A special ventilation room (negative airflow) is required. Door is kept closed. • A Powered Air-purifying Respirator (PAPR) is required to enter the room. • Some areas (surgery, MRI) wear a N-95 mask. An annual fit-test is required for N-95 users. Airborne Isolation: Patient transport: Patient: Patient wears surgical mask when out of room. Follow respiratory hygiene/cough etiquette. If skin lesions are present—cover lesions with clean sheet HCW: (Healthcare worker) Wear PAPR when entering room and handling patient May remove PAPR once out of the room and patient is wearing mask Hand hygiene prior to transport HCW does not need to wear PAPR during transport Equipment: Clean stretchers/wheelchairs after use Clean glucometers, thermometers, or any other equipment used for patient AIRBORNE/CONTACT PRECAUTIONS • Used for other occasions when a special ventilation room (negative airflow) is needed, i.e. varicella (chickenpox), measles, shingles (varicella) in an immunocompromised patient, or disseminated shingles. • These conditions are also spread by contact so Contact precautions are required also. • A PAPR, gown and gloves are required to enter the room. DROPLET PRECAUTIONS Protects against diseases spread by respiratory droplets. Including suspected or known: Neisseria meningitidis (meningococcemia), Meningitis of unknown origin (bacterial vs. viral) Influenza Pertussis (whooping cough). A surgical type mask is required to enter the room. Droplet Isolation: Patient Transport: Patient: Patient wears surgical mask when out of room. Follow respiratory hygiene/cough etiquette HCW: Wear mask when entering room (Healthcare May remove mask once patient is wearing a mask Worker) HCW does not need to wear mask during transport Equipment: Clean stretchers/wheelchairs after use Clean glucometers, thermometers or any other equipment used for patient SUMMARY • Standard: Wear PPE according to the level of anticipated contamination, when handling pt-care equipment and instruments/devices that are visibly soiled or may have been in contact with blood or body fluids. • Contact: A gown and gloves are required to enter the room. • Airborne: A PAPR is required when entering the room. • Droplet: A surgical type mask is required to enter the room. • Airborne/Contact: A PAPR, gown and gloves are required to enter the room. Equipment Decontamination If extra equipment is taken into an isolation room and used such as a reflex hammer, tuning fork, ophthalmoscope etc., be sure to decontaminate the equipment afterward with the PDI Surface Wipes located in a canister on the infection control cart or plastic wall hanger outside the patient room. Wash your hands after decontaminating the items. Note Taking in an Isolation Room For droplet or airborne isolation do not take notes in the room. For contact isolation, if you must, follow these steps. • don all appropriate PPE • take paper and a pen into the room • take and record the history information without touching any equipment or the patient. • place the paper and pen in the anteroom or outside the door. Take care to cover the information with a blank paper or turn the forms upside down so the information is not visible to those in the hall. • perform the physical exam, remove the PPE, wash hands and record this information after leaving the room..