Physiopathology and Rehabilitation of Nonarticular Rheumatism
advertisement

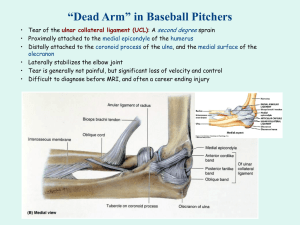
PHYSİOPATHOLOGY AND REHABİLİTATİON OF NONARTİCULAR RHEUMATİSM Dr. Pembe Hare Yiğitoğlu Near East University Faculty of Medicine Department of Physical Medicine and Rehabilitation 2012 • • • • • • • • • • • • Fibromyalgia Myofascial Pain Syndrome Bursitis Impingement Syndrome Calcific Tendinitis Bicipital Tendinitis De Quervain’s Tenosynovitis Patellar Tendinitis Adhesive Capsulitis Lateral Epicondylitis Medial Epicondylitis Plantar fasciitis FIBROMYALGIA • Fibromyalgia is a disorder characterized by – chronic widespread musculoskeletal pain, – stiffness, – paresthesia, – disturbed sleep, – easy fatigability, – multiple painful tender points, which are widely and symmetrically distributed. • Fibromyalgia affects predominantly women in a ratio of 9:1 compared to men. • The prevalence of fibromyalgia in the United States was reported to be 3.4% in women and 0.5% in men. PATHOGENESİS • Disturbed sleep has been implicated as a factor in the pathogenesis. • Nonrestorative sleep or awakening unrefreshed has been observed in most patients with fibromyalgia. • Sleep electroencephalographic studies in patients with fibromyalgia have shown disruption of normal stage 4 sleep [non–rapid eye movement (NREM) sleep] by many repeated α-wave intrusions. • Serotonin is a neurotransmitter that regulates pain and NREM sleep. • Deficiency of serotonin might also be involved in the pathogenesis of fibromyalgia. • Low levels of serotonin metabolites have been reported in the cerebrospinal fluid (CSF) of patients with fibromyalgia. • Growth hormone is secreted normally during stage 4 sleep, which is disturbed in patients with fibromyalgia. This may explain the extended periods of muscle pain following exertion. • The level of the neurotransmitter substance P has been reported to be increased in the CSF of fibromyalgia patients and may play a role in spreading muscle pain. • Patients with fibromyalgia have a decreased cortisol response to stress. • Autonomic dysfunction has also been suggested to play a role in the pathogenesis of fibromyalgia. • This may account for the dry eyes and mouth and the cold sensitivity and Raynaud’s-like symptoms seen in patients with fibromyalgia. • Reduced blood flow to the areas in the brain involved in the signaling, integration, and modulation of pain is demonstrated. (the thalamus, caudate nucleus, and pontine tectum) • Approximately 30% of patients fit a psychiatric diagnosis, the most common being – depression, – anxiety, – somatization, and – hypochondriasis. CLINICAL MANIFESTATIONS • Symptoms are generalized musculoskeletal aching, stiffness and fatigue. • Patients complain of muscle pain after even mild exertion, and some degree of pain is always present. • The pain has been described as a burning or gnawing pain or as stiffness. • Patients may complain of joint pain and perceive palpation of the tender points. • Fibromyalgia may be triggered by emotional stress, infections and other medical illness, surgery, hypothyroidism, and trauma. • It has appeared in some patients with hepatitis C infection, HIV infection, parvovirus B19 infection, or Lyme disease. FMS DİAGNOSİS • The Symptom Severity (SS) scale and the Widespread Pain Index (WPI) are combined to recommend a new case definition of fibromyalgia: • (WPI >7 AND SS >5) OR (WPI 3–6 AND SS >9). • This allows people with fewer painful areas but more severe symptoms to be diagnosed. Treatment • Antidepressants – Tricyclic antidepressants – Selective serotonin reuptake inhibitors (SSRI’s) – Duloxetine (Cymbalta), • Pregabalin (Lyrica), • Aerobic exercise programs • NSAIDs have not been proved to be effective in the treatment of fibromyalgia. • Avoid corticosteroids and narcotics. MYOFASCIAL PAIN SYNDROME • Myofascial pain syndrome is characterized by localized musculoskeletal pain and tenderness in association with trigger points. • Myofascial pain may follow trauma, overuse, or prolonged static contraction of a muscle, which may occur when reading or writing at a desk or working at a computer. • In addition, this syndrome may be associated with underlying osteoarthritis of the neck or low back. • Trigger points are a diagnostic feature of this syndrome. • Pain is referred from trigger points to areas distant from the original tender points. • Palpation of the trigger point reproduces or accentuates the pain. The trigger points are usually located in the center of a muscle belly. • Trigger point sites palpation may cause the muscle to twitch. • Myofascial pain most often involves the posterior neck, low back, shoulders, and chest. Treatment • Stretching: Intermittent cold and stretch • Thermotherapy: Hot pack, ultrasound • Electrotherapy: Interferential current, transcutaneous nerve stimulation • Cold laser therapy • Acupuncture • Dry needling • Myofascial trigger point injection • Medication • Exercise therapy – Stretching and postural exercises – Strengthening – Conditioning - swimming BURSITIS • Bursa is a thinwalled sac lined with synovial tissue. • The function of the bursa is to facilitate movement of tendons and muscles over bony prominences. • Bursitis is inflammation of a bursa. • Excessive frictional forces from overuse, trauma, systemic disease (e.g., rheumatoid arthritis, gout), or infection may cause bursitis. • Subacromial bursitis (subdeltoid bursitis) is the most common form of bursitis. • The subacromial bursa, which is contiguous with the subdeltoid bursa, is located between the undersurface of the acromion and the humeral head and is covered by the deltoid muscle. • Bursitis is caused by repetitive overhead motion and often accompanies rotator cuff tendinitis. • Another frequently encountered form is trochanteric bursitis, which involves the bursa around the insertion of the gluteus medius onto the greater trochanter of the femur. • Patients experience pain over the lateral aspect of the hip and upper thigh and have tenderness over the posterior aspect of the greater trochanter. • External rotation and resisted abduction of the hip elicit pain. • Treatment of bursitis consists of – prevention of the aggravating situation, – rest of the involved part, – nonsteroidal anti-inflammatory drug (NSAID), – local glucocorticoid injection. ROTATOR CUFF TENDINITIS AND IMPINGEMENT SYNDROME • Tendinitis of the rotator cuff is the major cause of a painful shoulder and is currently thought to be caused by inflammation of the tendon(s). • The rotator cuff consists of the tendons of the – – – – supraspinatus, infraspinatus, subscapularis and teres minor muscles. • Of the tendons forming the rotator cuff, the supraspinatus tendon is the most often affected. • This is probably because of – its repeated impingement between the humeral head and the undersurface of the anterior third of the acromion and coracoacromial ligament above, – the reduction in its blood supply that occurs with abduction of the arm. • The process begins with edema and hemorrhage of the rotator cuff, which evolves to fibrotic thickening and eventually to rotator cuff degeneration with tendon tears and bone spurs. • Subacromial bursitis also accompanies this syndrome. • Severe pain is experienced when the arm is actively abducted into an overhead position. • The arc between 60° and 120° is especially painful. • Tenderness is present over the lateral aspect of the humeral head just below the acromion. CALCIFIC TENDINITIS • This condition is characterized by deposition of calcium salts, primarily hydroxyapatite, within tendon. • The supraspinatus tendon is most often affected because it is frequently impinged on and has a reduced blood supply when the arm is abducted. BICIPITAL TENDINITIS • Bicipital tendinitis, or tenosynovitis, is produced by friction on the tendon of the long head of the biceps as it passes through the bicipital groove. • When the inflammation is acute, patients experience anterior shoulder pain that radiates down the biceps into the forearm. • Abduction and external rotation of the arm are painful and limited. • The bicipital groove is very tender to palpation. • Pain may be elicited along the course of the tendon by resisting supination of the forearm with the elbow at 90°(Yergason’s supination sign). TREATMENT OF TENDİNİTİS • NSAIDs, • Local glucocorticoid injection, • Physical therapy relieve symptoms. • Surgical decompression of the subacromial space may be necessary in patients refractory to conservative treatment. DE QUERVAIN’S TENOSYNOVITIS • In this condition, inflammation involves the abductor pollicis longus and the extensor pollicis brevis as these tendons pass through a fibrous sheath at the radial styloid process. • The usual cause is repetitive twisting of the wrist. • It may occur in pregnancy, and it also occurs in mothers who hold their babies with the thumb outstretched. • Patients experience pain on grasping with their thumb, such as with pinching. • Swelling and tenderness are often present over the radial styloid process. • The Finkelstein sign is positive. • It is elicited by having the patient place the thumb in the palm and close the fingers over it. • The wrist is then ulnarly deviated, resulting in pain over the involved tendon sheath in the area of the radial styloid. • Treatment consists initially of splinting the wrist and an NSAID. • When severe or refractory to conservative treatment, glucocorticoid injections can be very effective. PATELLAR TENDINITIS (JUMPER’S KNEE) • Tendinitis involves the patellar tendon at its attachment to the lower pole of the patella. • Patients may experience pain when jumping during basketball or volleyball, going up stairs. • Tenderness is noted on examination over the lower pole of the patella. • Treatment consists of rest, icing, and NSAIDs, followed by strengthening and increasing flexibility. ADHESIVE CAPSULITIS (FROZEN SHOULDER) • Adhesive capsulitis is characterized by pain and restricted movement of the shoulder, usually in the absence of intrinsic shoulder disease. • Adhesive capsulitis, however, – may follow bursitis or tendinitis of the shoulder – or be associated with systemic disorders such as chronic pulmonary disease, myocardial infarction, and diabetes mellitus. • Prolonged immobility of the arm contributes to the development of adhesive capsulitis. • The capsule of the shoulder is thickened, and a mild chronic inflammatory infiltrate and fibrosis may be present. • The shoulder is tender to palpation, and both active and passive movement is restricted. • In most patients, the condition improves spontaneously 1–3 years after onset. • While pain usually improves, most patients are left with some limitation of shoulder motion. • Local injections of glucocorticoids, NSAIDs, and physical therapy provide relief of symptoms. LATERAL EPICONDYLITIS (TENNIS ELBOW) • Lateral epicondylitis, or tennis elbow, is a painful condition involving the soft tissue over the lateral aspect of the elbow. • The pain originates at or near the site of attachment of the common extensors to the lateral epicondyle and may radiate into the forearm and dorsum of the wrist. • This painful condition is caused by repeated resisted contractions of the extensor muscles. • The pain usually appears after work involving repeated motions of wrist extension and supination against resistance. • Most patients with this disorder injure themselves in activities like tennis, carrying suitcases, or using a screwdriver. MEDIAL EPICONDYLITIS • Medial epicondylitis is an overuse syndrome resulting in pain over the medial side of the elbow with radiation into the forearm. • The cause of this syndrome is considered to be repetitive resisted motions of wrist flexion and pronation, which lead to microtears and granulation tissue at the origin of the pronator teres and forearm flexors, particularly the flexor carpi radialis. • It occurs in work-related repetitive activities or while playing golf or throwing a baseball. • On physical examination, there is tenderness just distal to the medial epicondyle over the origin of the forearm flexors. • Pain can be reproduced by resisting wrist flexion and pronation with the elbow extended. LATERAL AND MEDİAL EPICONDYLITIS TREATMENT • • • • Discontinuation of aggravating activities, Use of analgesic medications, Physical modalities, Bracing (e.g., medial/lateral counter-force strap and neutral wrist splint), • Corticosteroid injections, • Operative treatment can be warranted for those who fail to improve with conservative measures. PLANTAR FASCIITIS • Plantar fasciitis is a common cause of foot pain in adults. • Plantar fasciitis is thought to be the result of repetitive microtrauma to the tissue. • Several factors that increase the risk of developing plantar fasciitis include – obesity, – pes planus (excessive pronation of the foot), – pes cavus (high-arched foot), – limited dorsiflexion of the ankle, – prolonged standing, – walking on hard surfaces, – faulty shoes. • Patients experience severe pain with the first steps on arising in the morning or following inactivity during the day. • The pain usually lessens with weight-bearing activity during the day, only to worsen with continued activity. • Pain is made worse on walking barefoot or up stairs. • On examination, maximal tenderness is elicited on palpation over the inferior heel corresponding to the site of attachment of the plantar fascia. • The patient is advised to reduce or discontinue activities that can exacerbate plantar fasciitis. • Orthotics provide medial arch support and can be effective in relieving symptoms. • A short course of NSAIDs can be given to alleviate symptoms. • Local glucocorticoid injections have also been shown to be efficacious but may carry an increased risk for plantar fascia rupture. REFERENCES • • • • Physical Medicine & Rehabilitation DeLisa’s Physical Medicine & Rehabilitation Harrison’s Rheumatology Primer on the Rheumatic Diseases