Aetiology of Cataract
advertisement

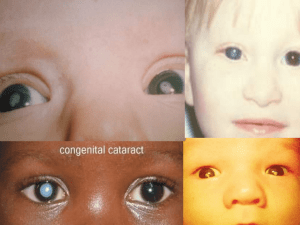
Cataract By Col Rana Intisarul Haq MCPS, FCPS (AFIO) Lens The lens is a biconvex structure located directly behind the posterior chamber and pupil It is the lesser of the two refractive elements in the dioptric system The equatorial diameter in adult is about 9-10 mm The anteroposterior width of the lens is about 6 mm The lens has certain unusual features. It lacks innervation and is avascular. Detail view of the anatomy of the eye cataract Definition Any congenital or acquired opacity in the lens capsule or substance of the lens , irrespective of the effects on vision is called cataract. Classification of Cataract According to Age According to Morphology According to Etiology According to maturity Congenital and acquired Age Related Senile Cataract Age related cataract is universal in persons over 70 years of age. Both sexes are involved equally. There is considerable genetic influence. Average age of onset of cataract is approximately 10 years earlier in tropical countries. 6 Age Related Cataracts senile Presenile Cataracts Diabetes Mellitus Myotonic Dystrophy Atopic Dermatitis Neurofibromatosis-2 Traumatic Cataract Direct Penetrating Injury Concussion Electric Shock & Lightening Ionizing Radiation Toxic Cataracts Steroids Chlorpromazine Miotics Busulphan Amiodarone Gold Secondary Cataracts Ch Ant Uveitis Ac Congestive Glaucoma High Myopia Hereditary Fundus Dystrophy According to Morphology Posterior Subcapsular Cataract Ant Subcapsualr Cataract Nuclear Cataract Cortical Cataract Mature Cataract THE LENS CATARACT F This diagram illustrates the different morphological characteristics of cataract together with their depth and location within the lens. The following illustrations demonstrate clinical examples of these anatomical entities. CLASSIFICATION ON BASIS OF MATURITY IMMATURE CATARACT MATURE HYPERMATURE MORGAGNIAN Causes Hereditary Age DM Steroids UV Rays Poor Nutrition Smoking Epidemiology Cataract surgery is the most commonly performed surgery in elderly patient Any Age Two peaks <10 Years >65 Years Pathology Depends on type of Cataract Early Changes – tiny areas of liquefaction called morgagnian degeneration seen as cortical spokes Progress to involve entire cortex Later on homogeneous appearance Etiopathogenesis of Cataract Caused by degeneration and opacification of existing lens fibres, formation of aberrant fibres or deposition of other material in their place. Loss of transparency occurs because of abnormalities of lens protein and consequent disorganization of the lens fibres 15 Etiopathogenesis of Cataract Any factor that disturbs the critical intra and extra cellular equilibrium of water and electrolytes or deranges the colloid system within the fibres causing opacification. Fibrous metaplasia of lens fibres occurs in complicated cataract. Epithelial cell necrosis occurring in angle closure glaucoma leads to focal opacification of the lens epithelium (Glaucomflecken) 16 Etiopathogenesis of Cataract Abnormal products of metabolism, drugs or metals can be deposited in storage diseases (Febry), metabolic diseases (Wilson) and toxic reactions (Siderosis) 17 Nuclear Cataract Mature Cataract Hypermature Cataract Traumatic Cataract(Penetrating Trauma) Vossius Ring PSC in Atopic Dermatitis Congenital Cataract Stellate PSC in Myotonic Dystrophy Shield Anterior Subcapsular Cataract (Atopic Dermatitis) PSC in Atopic Dermatitis Progression of Steroidinduced Cataract Anterior Subcapsular Opacities (Ch Ant Uveitis) Adv Cataract & Posterior Synechiae (Ch Ant Uveitis) Symptoms of Cataract 1. Blurring of vision 2. Frequent change of glasses due to rapid change in refractive index of the lens 3. Painless, progressive, gradual diminution of vision due to reduction in transparency of the lens 4. Second sight or myopic shift in case of nuclear cataract causing index myopia, improving near vision. 31 Symptoms of Cataract 5. Loss or marked diminution of vision in bright sunlight or bright light beam in central posterior sub-capsular cataract. 6. Monocular diplopia or polyopia in presence of cortical spoke opacities 7. Glare in posterior sub-capsular cortical cataract due to increased scattering of light 32 Symptoms of Cataract 8. Colored haloes around the light as seen in cortical cataract due to irregular refractive index in different parts of the lens. 9. Color shift , reds are accentuated 10. Visual field loss, generalized reduction in sensitivity due to loss of transparency 33 Signs of senile cataract Positive findings 1. Diminution of vision 2. Anterior chamber is shallow in cases of intumescent cataract and deep in cases of hypermature (shrunken) cataract 3. Tremulousness of iris in cases of hypermature shrunken cataract 34 Signs of senile cataract 4. Lenticular opacity , grey or white opacity in lens. Iris shadow in immature cataract. No iris shadow in mature cataract 5. Morgagnian Cataract- is characterized by liquefied cortex, which is milky and nucleus is seen as brown mass, seen as semicircular line, altering its position with change in position of head 35 Signs of senile cataract 6. Distant direct ophthalmoscopy will reveal black shadow against red background in cases of immature cataract. 36 Thank you Management of Cataract HISTORY Age of Onset Decreased Vision Painless, effecting daily routine? If the patient is bothered about his decreased vision. Trauma Any Ophthalmological Problems Drugs Intake Exposure to Radiations Systemic Diseases Skin disease, joint pains, etc. Family History Examination GPE SYSTEMIC EXAMINATION OCULAR EXAMINATION VISUAL ACUITY ADNEXA CORNEA ANTERIOR CHAMBER PUPIL VITROUS RETINA Investigations Blood Glucose ECG Chest x-rays (PA view) Blood Complete Picture Any specific relevant investigation (if indicated) Indication for Surgery Visual Improvement When the patient is bothered. Medical Indications When cataract is adversely affecting the health of the eye e.g.: Phacolytic Glaucoma Intumescent Cataract Diabetic Retinopathy Cosmetic Indications To restore black pupil Optimal Post Op Refraction If monocular correction is reqd. e.g. in contralateral dense or amblyopia best post op refraction is -1DS. If binocular correction is reqd difference between the two eyes should not be more than 3DS. SURGICAL TECHNIQUES ICCE ECCE ECCE with posterior chamber IOL implant Phacoemulcification ECCE IOL Implantation Phacoemulcification Operative Complications Complications of Local Anaesthesia Retrobulbar Hemorrhage Perforation of the globe, optic nerve or sheath Operative Complications: Bridle Suture Perforation of the globe Stripping of Descemet’s Membrane Damage to ciliary body Operative Complications(Contd) Rupture of the Posterior Capsule Capsular Rupture without Vitreous Loss Small Tear Large Tear or Zonular Tear Capsular Rupture with Vitreous Loss vitrectomy Posterior Loss of Lens Fragments Small Fragments Large Fragments Nuclear Material in Vitreous Operative Complications(Contd) Suprachoroidal Hemorrhage Source long or short ciliary artery Contributing Factors sudden in IOP coughing Valsalva Manoeuvre Vitreous Loss Sudden rise in B.P. Retrobulbar anaesthetic without adrenaline Operative Complications(Contd) Suprachoroidal Hemorrhage(Contd) Presentation after lens delivery, progressive shallowing of anterior chamber, increased IOP & iris prolapse, vitreous extrusion, loss of red reflex. In severe cases all intraocular contents may be extruded Immediate Treatment Closure of the Incision Administration of Hyperosmotic Agent Operative Complications(Contd) Suprachoroidal Hemorrhage(Contd) Subsequent Treatment Topical & Systemic Steroids Between 7 & 14 Day drainage of the blood, pars plana vitrectomy & air-fluid exchange Early Post-Operative Complications Iris Prolapse Cause - inadequate suturing Complications defective wound healing, ch ant uveitis, epithelial ingrowth, cystoid macular edema, excessive astigmatism. Treatment Early Post-Operative Complications Striate Keratopathy Cause damage to corneal endothelium Hyphema Early Post-Operative Complications Acute Bacterial Endophthalmitis Pathogenesis Causative Organisms Staph Epidermidis, Staph Aureus, Pseudomonas sp etc Source of Infection Prevention Treatment of local infections of the Patients Preoperative instillation of Povidine-iodine Meticulous draping Technique Postoperative injection Draping of Eyes Early Post-Operative Complications Acute Bacterial Endophthalmitis(contd) Clinical Features severity Time Interval Staph Aureus - 1st to 3rd day Staph Epidermidis - 4rth to 10th day Differential Diagnosis Retained Lens Matter Toxic Reaction Difficult or Prolonged surgery Fibrinous Exudation in Severe Acute Endophthalmitis Small Hypopyon Acute Bacterial Endophthalmitis(contd) Clinical Features Differential Diagnosis Retained Lens Matter Toxic Reaction Difficult or Prolonged surgery Early Post-Operative Complications Acute Bacterial Endophthalmitis(contd) Management Identification of causative organism aqueous samples vitreous samples Antibiotics Vitrectomy Steroids Subsequent therapy Late Post-Operative Complications Opacification of the Posterior Capsule Types Elschnig’s Pearls Capsular Fibrosis Indications for Treatment Visual Acuity Impaired Visualization of Fundus Monocular Diplopia or severe glare Nd:YAG Laser Capsulotomy Complications Elschnig Pearls Fibrosis of Posterior Capsule Technique of Nd:YAG Laser capsulotomy Late Post-Operative Complications Malposition of IOL Tilting Decentration Treatment Corneal Decompensation Causes Treatment Late Post-Operative Complications Retinal Detachment Risk Factors Disruption of Posterior Capsule Vitreous Loss Lattice Degeneration Sunset Syndrome Cause Traetment Late Post-Operative Complications Chronic Endophthalmitis Causative Organism Propionibacterium Acnes Staph Epidermidis Clinical Features Treatment Strategy steroids & antibiotics Removal of IOL, remaining cortex & entire capsular bag