Introduction
• Opacity in lens
• Can be: Visually significant or not
Stable or Progressive
Congenital or Acquired
Unilateral or Bilateral
Partial or Complete
• Congenital: incidence 6/10 000
10% of childhood blindness
Classification : Acquired cataracts
• Systemic diseases : Diabetes mellitus
: Myotonic dystrophy
: Atopic dermatitis
: Neurofibromatosis 2
• Ocular diseases
: Chronic anterior uveitis
: High myopia
: Fundus dystrophies eg Retinitis
pigmentosa
• Drugs
: Corticosteroids
: Chlorpromazine
• Trauma
: Blunt
: Sharp
Congenital cataracts: Bilateral
•
•
Genetic Mutation : Autosomal Dominant
Metabolic
: Galactosaemia
: Lowe
: Hypoparathyroidism
: Fabry
•
Infective
•
Chromosomal
•
Skeletal
•
•
: TORCH organisms
: Trisomy 21 (Down)
: Trisomy 18 (Edward)
: Trisomy 13 (Patau)
: Hallerman-Streiff
: Nance-Horan
Ocular anomalies : Aniridia
: Anterior segment dysgenesis syndrome
Idiopathic
: in 50%
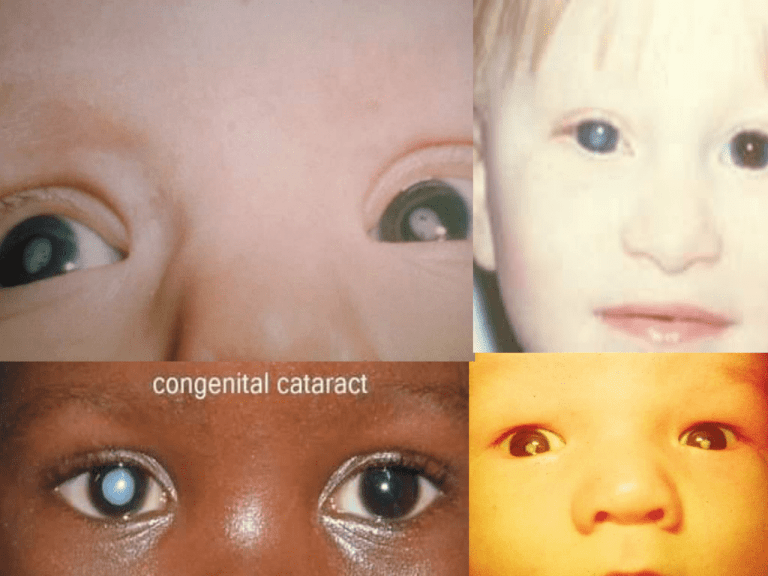
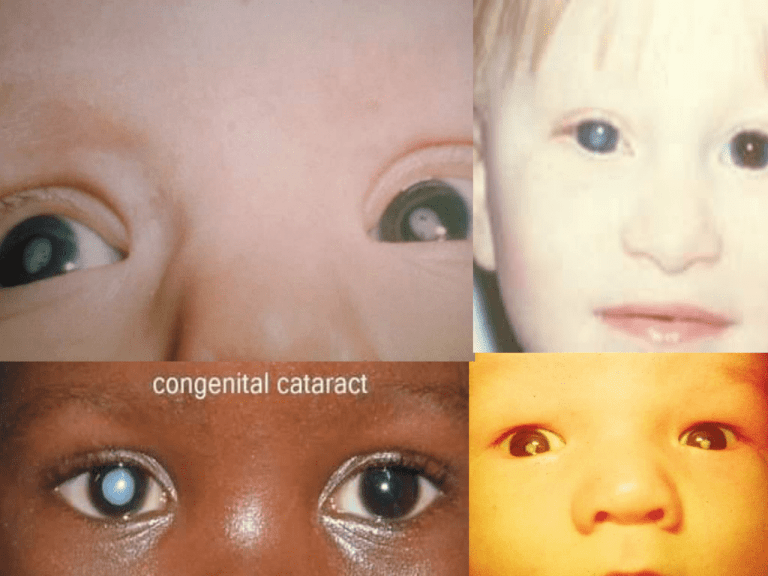
Congenital Cataracts
• Responsible for nearly 10% of all visual loss in
children worldwide
• Approximately 0.03% of newborns have some form
of congenital cataract
• Most are not associated with additional
developmental problems
• Around one fifth of these patients have a family
history of congenital cataract but in up to half of all
cases there is no family history
Congenital cataract surgery
Cataract surgery in children, although
complex and time consuming , can have
excellent results.
1) Unilateral or bilateral
2) Cause : usually no cause is found
Cataract Types
1)Polar Cataract
2)Lamellar Cataract
3)Sutural Cataract
4)Coronary Cataract
5)Cerulean Cataract
6)Nuclear Cataract
7)Capsular Cataract
8)Membranous Cataract
1)Polar Cataract
2)Lamellar Cataract
3)Sutural Cataract
3)Sutural Cataract
4)Coronary Cataract
5)Cerulean Cataract
(Blue Color)
5)Cerulean Cataract
(Blue Color)
• Cerulean cataracts are opaque areas that develop in the
lens of the eye that often have a bluish or whitish color.
They may be present at birth or develop in very early
childhood, but may not be diagnosed until adulthood.[1]
They are usually bilateral and progressive.[2] Infants can be
asymptomatic, but may also be visually impaired from birth
and develop nystagmus and amblyopia.[2] In adulthood,
the cataracts may progress, making lens removal
necessary.[1] Cerulean cataracts may be caused by
mutations in several genes, including the CRYBB2, CRYGD,
and MAF genes, and are inherited in an autosomal
dominant manner. No treatment is known to prevent
cerulean cataracts, but frequent evaluations and cataract
surgery are typically required to prevent amblyopia as the
opacities progress.
6)Nuclear Cataract
6)Nuclear Cataract
7)Capsular Cataract
8)Membranous
cataract
Unilateral cataract
• Unilateral cataracts are more
likely to cause visual loss
because of the competition
between the two eyes
Congenital cataracts: Unilateral
• Sporadic, no family history
• Ocular anomalies : Persistent fetal vasculature(PHPV)
• Cause identified in only 10%
Etiology
There is no benefit in doing a large number of tests and
investigations on all children with cataract.
It is better to take a careful history.
a) Family history
b) Any illnesses or drugs used during the pregnancy
c) Pediatric consultation
d) Intra – uterine infection ( rubella , cytomeygalovirus ,
syphilis)
e) Hereditary systemic disorders
Downs syndrome
Turners syndrome , Stickler syndrome
Etiology of Pediatric Cataracts
• Hereditary
– Autosomal dominant form most common
• Genetic and Metabolic Diseases
– Down syndrome
– Marfan’s syndrome
– Myotonic Dystrophy
• Maternal Infections
– Rubella, Syphilis, Toxoplasmosis, Varicella
Rubella Virus
Rubella Virus
Rubella virus is the pathogenic agent of the disease Rubella, and is the cause of
congenital rubella syndrome when infection occurs during the first weeks of
pregnancy. Humans are the only known host of this virus.
Rubella virus is the only member of the genus of Rubivirus and belongs to the family
of Togaviridae, whose members commonly have a genome of single-stranded RNA of
positive polarity which is enclosed by an icosahedral capsid.
The molecular basis for the causation of congenital rubella syndrome are not yet
completely clear, but in vitro studies with cell lines showed that Rubella virus has an
apoptotic effect on certain cell types. There is evidence for a p53-dependent
mechanism.
Rubella Virus
Rubella
cytomegalovirus
cytomegalovirus
Syphilis Bacteria
Treponema pallidum is a Gram-negative spirochaete bacterium with
subspecies that cause treponemal diseases such as syphilis, bejel, pinta
and yaws. The treponemes have a cytoplasmic and outer membrane. This
bacterium can be detected with special stains, such as the Dieterle stain.
Syphilis
Downs syndrome
Stickler syndrome
Stickler syndrome (hereditary progressive arthro-ophthalmopathy) is a group of
genetic disorders affecting connective tissue, specifically collagen. [1] Stickler
syndrome is a subtype of collagenopathy, types II and XI. Stickler syndrome is
characterized by distinctive facial abnormalities, ocular problems, hearing loss, and
joint problems. It was first studied and characterized by Gunnar B. Stickler in 1965.
Turner syndrome or Ullrich–Turner syndrome (also known as "Gonadal
dysgenesis"[1]:550), 45,X, encompasses several conditions in human females, of which
monosomy X (absence of an entire sex chromosome, the Barr body) is most common.
It is a chromosomal abnormality in which all or part of one of the sex chromosomes is
absent (unaffected humans have 46 chromosomes, of which two are sex
chromosomes). Normal females have two X chromosomes, but in Turner syndrome,
one of those sex chromosomes is missing or has other abnormalities.
•
•
•
•
•
•
•
•
•
•
•
•
•
Common symptoms of Turner syndrome include:
Short stature
Lymphedema (swelling) of the hands and feet
Broad chest (shield chest) and widely spaced nipples
Low hairline
Low-set ears
Reproductive sterility
Rudimentary ovaries gonadal streak (underdeveloped
gonadal structures that later become fibrosed)
Amenorrhoea, or the absence of a menstrual period
Increased weight, obesity
Shield shaped thorax of heart
Shortened metacarpal IV
Small fingernails
•
•
•
•
•
•
•
•
•
•
Characteristic facial features
Webbed neck from cystic hygroma in infancy
Coarctation of the aorta
Bicuspid aortic valve
Poor breast development
Horseshoe kidney
Visual impairments sclera, cornea, glaucoma, etc.
Ear infections and hearing loss
High waist-to-hip ratio (the hips are not much bigger than the waist)
Attention Deficit/Hyperactivity Disorder or ADHD (problems with
concentration, memory, attention with hyperactivity seen mostly in
childhood and adolescence)
• Nonverbal Learning Disability (problems with math, social skills and spatial
relations)
• Other features may include a small lower jaw (micrognathia), cubitus
valgus,[8] soft upturned nails, palmar crease, and drooping eyelids. Less
common are pigmented moles, hearing loss, and a high-arch palate
(narrow maxilla). Turner syndrome manifests itself differently in each
female affected by the condition, therefore, no two individuals will share
the same features.
When to operate
1) If a child is behaving and developing
normally, do not operate , but keep under
review.
2) Do not be misled by the red reflex as children
may see remarkably well despite a copsular
cataract through which no red reflex is visible
Loss of accommodation by surgery
3) Removing a cataract in a child removes their
ability to accommodate.
The visually significant cataract
•
•
•
•
In central visual axis, bigger than 3mm
Posterior cataract
No clear zones in between
Retinal details not visible with direct
ophthalmoscope
• Nystagmus or strabismus present
• Poor central fixation after 8 weeks
Treatment
• Surgery: Cataract extraction and intraocular lens
implantation for visually significant cataract
• By 6 weeks of age
• Bilateral cases: 1 week apart
• Non visually significant cases : careful observation, possible pupillary
dilation
Surgery
1) Cataract surgery in children is very different
to a cataract surgery in adults.
2) Children do not have a hard lens nucleus so it
can be removed by aspiration alone.
3) Anterior vitrectomy is necessary after
complete lens aspiration.
4) An intact rim capsule is necessary.
Anterior vitrectomy is mandatory
Capsular rim
IoL insertion
It is possible to insert an ioL at the time of
surgery or later as secondary procedure.
Anterior capsule of a child is much more elastic
than an adult lens. So capsulorhexis is more
difficult.
Post capsule
If the capsule is left intact , it will opacify.
Lensectomy
It is belter to do lensectomy under 5 years of
age and ECCE on older children for less risk of
amblyopia.
So vision lost from capsule opacity can be
regained.
How to prevent amblyopia
In infants it is essential to correct aphakia as
soon as possible after surgery.
1) One option is to implant an IoL when the
cataract is removed.
2) Second option is contact lens .
3) Third option is wearing glasses .
Problems with IoL
At birth the human lens is more spherical than
in adults. It has a power of about 30 D, which
compensate for the shorter axial length of a
baby's eye.
This decreases to about 20 – 22 D by the age of
five. So an Iol which gives normal vision to an
infant will lead to significant myopia when he
or she is older.
IoL correct power ?
Since corneal power of the cornea and axial
length of the globe, changes are most rapid
during the first few years of life and this makes
it almost impossible to predict the correct
power of lens for IoL in any infant.
IoL Implantation
IoL implantation has become quite routine for
older children, but it is still very controversial
in younger children, particularly those under
two years old.
Post operative care
In children the surgery is only the beginning of a
prolonged course of treatment for prevention
of amblyopia.
Refraction
2) Contact lens
the first priority is to correct the aphakia and
this should be done as early as possible.
In rich countries contact lenses are widely
used. They require meticulous hygiene.
3) Spectacles or an IoL.
Even if an IoL is used there will be some
residual refractive error and spectacles is
necessary.
Complications of cat surgery
1)
2)
3)
4)
Amblyopia
Posterior capsule opacification
Glaucoma
Retinal detachment
Amblyopia
1) Most children with congenital cataract will be
amblyopic
2) removing the cataract and correcting the
aphakia can improve it's Nystagmus and
amblyopia .
3) Occlusion treatment of the preferred eye is very
essential.
4) The risk of amblyopia is greatest during the first
year of life and declines rapidly after the age of
five.
ضمن عرض پوزش
بدلیل حجم باالی LECTUERادامه اسالیدها امکان پذیر
نمیباشد در صورت نیاز به ادامه لطفا به واحد سمعی و
بصری مرکز آموزشی درمانی فیض مراجعه و یا با شماره
تلفن 03114476010داخلی 392تماس حاصل نمائید
با تشکر