Mycobacterium 2
advertisement
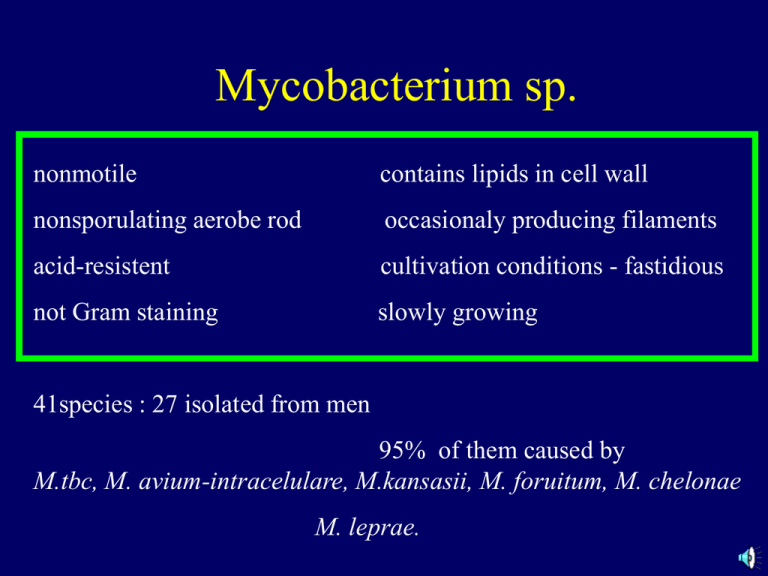
Mycobacterium sp. nonmotile contains lipids in cell wall nonsporulating aerobe rod occasionaly producing filaments acid-resistent cultivation conditions - fastidious not Gram staining slowly growing 41species : 27 isolated from men 95% of them caused by M.tbc, M. avium-intracelulare, M.kansasii, M. foruitum, M. chelonae M. leprae. Classification of mycobacteria Slowly growing -Mycobacterium tuberculosis complex Mycobacterium tuberculosis , Mycobacterium leprae, M.bovis, M.ulcerans Atypical mycobacteriae – classification according Runyon M.kansasi, M.marinum photochromatic M.scrofulaceum scotochromatic M.avium, M.intracelulare slowly growing non pigmented M.fortuitum, M.chelonae quickly growing non pigmented Mycobacterium – genus Cell wall rich for lipids = hydrophobic surface = resistent for desinfection = not accepting colour, but if stained (special procedure – warming sc.Ziehl Neelsen) they resist to decolorisation by strong acid = acid resistent, acid fast Mycobacterium tbc – Ziehl Neelsen sstaining Growing conditions and colony morphology complex structure of cell wall and cultivation requirements Speed of growth and pigmentation – classification sc. Runyon: Slowly growing, non pigmented – M. tbc...... I. group – fotochromatic – production of intense yellow pigment karotenoid on light II. group – scotochromatic – production of pigment in dark and light III. group – slowly growing not pigmented IV. group – rapidly growing not pigmented Group of slowly growing and IIIrd group acc. Runyon - generation time 12 –24 hrs – visible colonies appeat after 3-8 weeks Group I, II and IV - rapidly growing – first coloniesafter 3 days and more M. leprae – not cultivatable Cell wall – complex Peptidoglyc (rigidity of the structure) with phosphodiesterically bound molecules D - arabinose a D - galactose to mycolic acid (most important lipids in cell wall). with free lipids (waxes, mycosides – cord factor) – responsible for paralel arrangement of bacili in virulent strains polypeptidmi (PPD) na povrchu. Cell wall – most outer layer polypeptides (PPD) on the surface (purified protein derivate) – antigenic properties, -- stimulation of cell immunity, -- extracted and partially purified (PPD) used for skin test Tuberculin reaction -- test for specific (anti TBC) cell immunity detection – hypersensitivity of the IVth type – delayed cell hypersensitivity reaction Patogenesis of infection Destruction of tissue and fibrosis – produced by host immunity on infection by M.tbc Intracelular bacterium – escape innate immune mechanism Tuberculosis – classical mycobacterial disease starts after inhalation of M.tbc * engulfment by alveolar macrophages * multiplication intracelularly - escape immunity mechanism and destoy phagocytes that engulfed them. * repetition of this process (phagocytosis of bacilli, replication of M.tbc, lysis of cells = multilobular giant cells of macrophages„Langhans cells“) * inficated macrophages spread to local lymphatic nodes, blood net, bone marrow, spleen, kidney, bones, CNS...) 2-4 weeks after infection – specific immunity reaction Cytokns production by CD4 T lymphocytes aktivise macrophages and they are then able to kill bacterie localise inside: low antigenic burden – small tissue devastation high antigenic burden (masive infection – big tissue devastation-necrosis Effectivity of bacteria elimination depends on size and localisarion of infection: localised activated macrophages (granuloms < 3 mms): macrophages penetrate inside it and kill bakcteria, eliminate spreading larger necrosis, caseous granulomas – encircled by fibrin, bacteriae survive inside, can reactivate after years Immunity mechanism: * cytokins produced by T lymfocytes, * activcation of complement cascade, * ischemia of tissue , * hydrolytic enzymes produced by macrophages Cell immunity Reactivation in cell immunity decrease – lack of T lymphocytes: -immunodeficiencies -HIV-AIDS -agea -immunosupresive therapy – rheumatoid artritis, SM, Crohn disease – biological therapy to depress cell immunity requires dignosis of latent infection Clinical sy and diseases M.tbc can infect any organ * lung * extrapulmonal tbc * Tbc in HIV infected M.avium-intracellulare * lung (in immunocompromised) * asymptomatic colonisation * disseminated infection in HIV positive M. leprae * Lepra lepromatosa, * Lepra tuberculoid Other mycobacteriosis * Lung disease (M.kansasií) * Skin disease (M. marinum,M.ulcerans) Clinical sy Lung tbc after inhalation of contaminated aerosol Inicial lung infection – middle lobe or lower lobe, multiplication 3-6 weeks, untill cell immunity is stimulised 5% infected – acute disease before 2 years 5-10% later in life Non specific signs, few sputum, rtg signs of lung infections, positive skin test, laboratory verification microscopically and by cultivation. Active disease with pneumonia, production of abscesses and cavities with sever involvement of upper lobes. Extrapulmonal tbc – hematogenous spread during inicial phases (nodes, pleura, UGT) – not necessary the lung symptoms Tbc in HIV positive – decrease of CD4 lymphocytes, present before other opportunistic infections Patogenesis and immunity in Mycobacterium leprae Lepra, Hansen´s disease: Lepra - lepromatous – strong antibody reaction, defect of cell immunity to M.leprae as antigen.Many bacteria in skin macrophages (Schwann cells), very infectious Lepra - tuberculoid – strong hypersensitivity of delayed type, feeble humoral immunity, many lymphocytes and granulomas, few bacteria in tissue (activated macrophages fagocyte and eliminate bacteriae Symptoms are caused by immunity reactions Other mycobacteria: M.kansasí,M avium-intracellulare granulomatous inflamation – localised lung infection, clinicall the same as tbc, or disseminated infection M.marinum, M.ulcerans: skin infection – prefer lower themperature M.fortuitum, M.chelonae: very rarely disseminated infection HIV-AIDS Laboratory diagnosis Microscopy rapid dg, Ziehl Neelsen, fluorescence, preparation of sample Cultivation morning sputum 3 days consequently or a lot of other liquidv– urine * slow growing * overgrowing contaminating flora * decontamination, NaOH, * egg media(Šula,Lowenstein) and solid agar media * rapid dg - detection of metabolism of palmit acid and CO2 - Genetic probes detection of aminoacids specific for M.tbc, shortens dg to 6 hrs, directly from biol.material Serology not sensitive nor specific Resistencie on common ATB longlasting therapy (18 –24 mnths lepra., 6-9 mnths other) = rapid evolution of resistence = use of combination of antimycobacterial protected ATB INH, rifampicin, pyrazinamid, ethanbutol, streptomycin + cycloserin (atypical), chinolons (contaminating infection) 1990 common rezistence in USA in HIV positive Rapidly growing mycobacteriae – very resistent on common ATT - sensitive on aminoglykosides, cephalosporins, TTC, chinolons M.leprae rapid development of resistence – combination dapson+rifampicin, clofazimin+etionamid Antituberculotics and therapy • Streptomycin (kills actively multiplying M.tbc) • Izoniazid, Rifampicin (acting on strains in caseouse necrosis) • Ethanbutol Etionamid Kanamycin Cycloserin Pyrazinamid (active intra cellularly) Pacients woth lung tbc - 3 populations of M.tbc - localised extracellularly in cavities, intracellularly in macrophages, in caseouse necrosis • Combination of 2-3 ATTs. Detection of ATB susceptibility • ATTs are dissolved in cultivation medium, and on the surface, the tested strain is innoculated • Method of proportionnal sensitivity – dilution method. Innoculum is diluted so that cultivation there will be 100300 CFU – colony forming unit – on the medium • If the number of resistent colonies (growing on the medium with ATT) is higher then 1% (1-3 colonies) M. tbc – therapy will be not efficient • Spontaneous appearance of resistent mycobacteria without exposition to ANTITUBERCULOTICS • Frequency of resistent cells is 1:105 in INH and 1:106 in STM – if the combination is used, incidence of resistent strains will be 1011. • Overall population of bacteriae in patients with open cavity is 10 7 - 109, so there can be as much as 102 - 104 of resistent strains. • 1 ATT means owergrowing of resistent population of strains, that will replace sensitive killed bacterial population. Combination of 2 and more ATT: INH+RIF - 9 mnths, + STR+ Ethanbutol 2-8 weeks from 2nd mnth 2x weekly, INH + Ethanbutol 18-24 months, Therapy principals • ATT are active only on multiplying mycobacteria, • activity of the growth depends on the availability of oxygen and pH (optimal is neutral or alcaline) • Max. growth is in open cavities, min. is in caseouse necrosis. • i.c. – in fagosomes - pH is 5,5, acid – slow growth and less bacteria, less resistent strains – ATT supporting acid environment are used - Pyrazinamide. (STM is not able to work in fagosomes and loss activity in acid pH) • in closed caseouse necrosis there is just a few oxygen, slow metabolism, few living cells, neutral pH and feeble grow ATT Bactericidal: STM – extracelular mycobacteria in tissue • INH – kills slowly growing cells • Rifampicin – effective on mycobacteriae in caseouse necrosis and macrophages • Pyrazinamide – only in acide pH and macrophages Bakteristatic: Ethanbutol – only in combination, able to penetrate in mycobactera situoated ic and ec • Capreomycin, Kanamycin – baktericidal for e.c mycobacteria in cavities • Ethionamid, cycloserin – bakteriostatic for i.c and e.c Epidemiology – process of the spread of infection M.tbc Man is the only natural host and source Transmission by longlasting narrow contact with ill or infected Particles of aerosol with 1-3 tbc bacili can get as far as to alveoli 5-200 bacteriae may cause infections. Rising of the number of cases, AIDS pacients, alcoholics, narkoman Resistence on antituberculotics ATTs Other mycobacteriae M. bovis – infection of annimals, source of infection of men from milk M.avium-intraellulare complex – present in water and soil and annimal Transmission by infected food to immunocompromised patients with AIDS M.leprae 12 milions, 62% in Asia, 34% in Africa, 10% in USA, transmission by longlasting, premanent contact with infected, by inhalation, skin contact with nose secresion, exudation from wound Prevention Chemoprophylaxis INH 1 year after the contact with M.tbc and positive skin test hepatotoxicita Vaccination atenuated living strain of M. bovis - bacillus Calmette Guerin–BCG strain 5th day after birth, side effect – BCG-itida - positive tuberculine skin test ! interpretation! BCG • Vaccination against tbc • BCG - Bacillus Calmette - Guérin – vaccination by life attenuated strains Mycobacterium bovis – cross reacting Mycobacterium tbc. • Testovating of cell immunity - in vivo skin tuberclin test – Mantoux - in vitro Tuberculin reaction i.d 0,1 mcg = 5TU - tuberculin unit aplication of PPD purified protein derivate of cell wall after 48 – 72 hrs <15mms negat – without reaction, anergia ( HIV infected too), 15mms - OK., immunity more than 15 mms – strong reactions – susp.expositions IGRA – interferon gama release assay Quantiferon – in vitro test of specific cell mediated immunity • method to detect latent infection • in vitro detection of specific CMI in blood Principes • Person exposed in past to antigen has specific T lymfocytes and memory cells • after exposition of antigen to whole blood, the rapid and repeated stimulation of antigen specific memory cells followed by release of cytokins follows (interferon gama) • Detection of released IFN-gama (by ELISA) is a specific proove of cell mediated reaction to specific antigen (stimulationg) Postup pri inkubácii a zbere plazmy Test is based on exposition of blood in 3 tubes: - antigen of M.tbc, - v 1 skúmavke - non specific mitogen – positive control - negatíve control – without antigen Whole blood is sampled to 3 tubes – the blood should adhere to tube wall., after thorought agitation for 5 sec. Incubation for 16 – 24 hrs at 37 dg.C (untill the memory cells are sensitised by M.tbc – exposition to specific M.tbc antigen on the surface of the tube stimulateds secression of INTERFERON GAMA Blood si centrifugated Plasma is sampled for detection of interferon gama To detect IF-gama secreted after in vitro activation (antigen on the surface of the vial + memory cells in whole blood of the patient) of memory cells of M.tbc and detected by ELISA test Interprettion: comparison of IFG in the tube with -TB ag : negat.contr. Negat control – exclude nonspecific secrection( ex. after therapy) Posit. control – shows capability to react (negat. in imunocompromised or after therapy Comparison • • • • • Mantoux: in vivo reaction of memory cells after BCG and M.tbc. stimulation aplication of PPD i.d. memory cells after BCG or M.tbc will go to the place of innoculation inflamation and induration in the place • • • Quantiferon: in vitro memory cells after M.tbc infection in the tube contact of memory cell with + M.tbc = release of gama IF if memory cells present. Memory cells after infection ELISA