Presentation
LCDR C. Fredette, BSN, CCHP, RN
CDR R. Hunter Buskey, DHSc, CCHP, PA-C
OBJECTIVES:
Review unique characteristics of inmates with diabetes
Highlight clinical practice guidelines for correctional diabetic management
Discuss practical methods to increase active inmate participation in diabetes management that incorporate personal behavior change
Review glucose meter distribution program for inmates
DIABETES PREVELENCE:
438 million worldwide by 2030
25 million United States = 8% of US Population
7 th leading cause of death 2007
International Diabetes Federation (IDF); Centers for Disease Control and Prevention (CDC);
Bureau of Justice Statistics (BJS)
DIABETES RISK FACTORS:
Non-Modifiable
African American, Native American, Hispanic
Family history
Chronic illnesses
Modifiable
Food choices
Physical activity
Weight
FEDERAL INMATE PROFILE
White
African-American
Other
Hispanic
Non-Hispanic
57.2
39.2
3.2
32.2
67.8
Bureau of Justice Statistics , 2009
CHALLENGES FOR INMATES WITH
DIABETES
Lifestyle
Health literacy and education
Culture
Health numeracy
Non-formulary drugs
Motivation
Health beliefs
SURGEON GENERAL’S
National Prevention Strategy
Injury and violence free living
Tobacco free living
Preventing drug abuse and excessive alcohol use
Healthy Eating
Active Living
Mental and emotional well being
Reproductive and sexual health
COST FOR DIABETES CARE
US diabetes related costs 2007:
174 billion; 116 billion for direct medical care
Inmate average health care costs $7.15/day
Range from $2.74-$11.96
US Department of Health and Human Services, 2011
The Council for State Governments, 2004; 1998 survey
IDF AACE ADA ADA Inmate
Evidenced based, cost effective levels of care
6.5
Aggressive, comprehensive
Team based care
6.5
Well and sick care for diverse populations
7.0
Early assessment, staff training and coordination of resources
7.0
NCCHC FBOP
Emphasize selfmanagement,
Quality improvem ent
Primary care provider team, strive for target goals
7.0
7.0
Chronic disease management models for diabetes
Screening, diagnostic, therapeutic
Categories for increased risk
All Guidelines
Testing
Target goals
Assessment of glycemic control
Guidelines
ADA Treatment Goals
Glycemic control
HBA
1
C
Preprandial plasma glucose
< 7.0%
90-130 mg/dl
Peak postprandial plasma glucose <180 mg/dl
< 130/80 mmHg Blood pressure
Lipids
LDL
Triglycerides
HDL
Weight
<100 mg/dl
< 150 mg/dl
> 40/mg/dl
BMI Targets
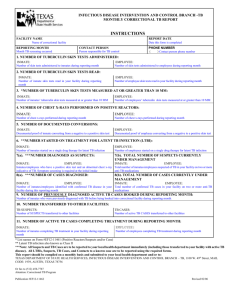
FACILITY TIMELINE
2004 – Medical record review revealed clinical improvement opportunities for diabetic inmates
(physical assessment, medication, patient education)
2005 – FCC Butner designation “Diabetes Center of Excellence” (DICE)
2006 – Committee launched diabetes awareness programs for staff and inmates, now annual
2007 – inmate education classes, re-established target clinical outcomes
2008 – initiation of inmate self monitoring blood glucose program
INMATE CHARACTERISTICS:
~20% known or at risk are in diabetes chronic care clinics
Disproportionate number of federal inmates are overweight; many take anti-psychotics which can cause obesity
Predominately Hispanic, African American
INMATE BARRIERS TO ACHIEVING
TARGET GOALS
Inmate contributions to food choices – commissary, menu
Lockdowns
Insulin timing
Lack of community support
Comorbidities
Quality Improvement
The continual assessment of health care delivery to improve outcomes and reduce medical errors
Areas to improve include:
Appropriate utilization of medical services based on evidence, reduce service variability, address disparities, improve communication, increase patient-centered care, incorporate technology
Agency for Healthcare Research and Quality (AHRQ), 2012
Performance Improvement Priorities
Monitoring Parameters for Control and Complications
Every Visit
Blood Pressure
Foot Exam
Weight, Waist Circumference
3-6 months
HBA1c
Every 3 months (for poor control ):
Initiate/change medication
Every 6 months for stable control
Annual
Dilated Eye Examination
Lipid Levels*
Microalbumin
* Every 2 years if levels fall in lower risk categories
American Diabetes Association. Clinical Practice Recommendations. Diabetes Care.
FACILITY DIABETES STATISTICS
Majority Type 2
25% at or below target goals*
~500 insulin users
Insulin use inevitably rises
* estimated by random hemoglobin A1c review
FACILITY INSULIN EXPENDITURES
10614
42K
1866
46K
Increase in insulin expenditures from 2010 to 2011
No significant change in Metformin or SFU costs
Significant decrease in TZD costs
Sulfonyurea = SFU; Thiazolidines = TZD
PHARMACY COSTS FOR DIABETES
MEDICATIONS*
Insulin is associated with the greatest staff resource**
Insulin is associated with increased risk for medical errors, medical emergencies and morbidity
*2010/2011 data; does not include lancets, needles, syringes, alcohol swabs, gauze, band aids
**insulin prep time, pill line time, triage and emergency interventions
Federal Bureau of Prison
Inmate Self monitoring program
Agency glucose meter distribution program initiated in 2008 for inmate insulin users
Considerations:
Staff apprehension
Oversight
Education
Cost
Accountability
Continuity during transfers
Hundreds of glucose meters issued since program inception
D 50
Noticeably Less Medical Emergencies
PROGRAM REVIEW OUTCOMES
Hemoglobin A1c (HBA1c) Values by groups
Group one n=10
Pre baseline
Post baseline
Group two n=29
Pre baseline
Post baseline
Group three n=22
Pre baseline
Post baseline
N=61
Minimum Maximum Mean Std. Deviation
Target Glycemic Control
5.9 6.8 6.4 0.3
Ø
5.9 6.9 7.0 1.0
Mild-Moderate Glycemic Control
7.1 9.5 8.1
7.1 9.5 8.7
Poor Glycemic Control
9.6 14.8 10.7
9.6 12.2 10.0
HBA1c expressed as %
0.7
1.4
1.2
1.1
CLINICIAN BARRIERS
Definition of good glycemic control
(treatment complacency)
Accountability for glycemic monitoring and interventions
Complexity: BS, BP, lipids, weight, personal behaviors for the incarcerated
Specialist and expert availability
GOALS FOR PATIENT CENTERED CARE
√
Education
√
Nutritional support
√ Physical activity
√ Medications
√ Self-monitoring blood glucose
(SMBG)
NEXT STEPS-TIME TO WORK TOGETHER
Marshalls
Commissary
Health Services
1200
Custody
2100
INMATE
1500
Food Service
1800
Unit Management Recreation
MOVING FORWARD
Group medical visits
Group session for education; train the trainer
Staff and inmate lead physical activity sessions
Quality of life groups for psychosocial support
Foot clinic – Best Practice
Self-Management clinic (food, activity, medication and insulin)
Certified Diabetic Educator resources; Bureau of Prisons has issued an announcement for regional diabetic nurse consultants
Inmate self referrals (dental, eye, foot care)
Community partnerships – health fair, education for credit
What we learned is we cannot manage diabetes without a strategic self-management plan
Thank You…
FCC Butner, Diabetes Center of Excellence Committee
(DICE)
Quality Management Department