Reproductive
System
NUR 302
Unit II
Sexually Transmitted Diseases
Gonorrhea & syphilis reportable to
health dept, genital herpes & warts not
Often STDs coexist
30% gonorrhea - resistant strains
25-40% cases– teenagers, young adults
Incidence of syphilis declining
Chlamydia trachomatis- most prevalent
Contributing Factors to STDs
Earlier maturity, increased longevity
Sexual freedom, media, changes in
women, marriage, religion, family
Drug abuse correlates with STDs
Methods of contraception
Gonorrhea
Niesseria gonorrhoeae – in male
urethra, cervix, rectum, oropharynx
Spread by direct physical contact
Killed by drying, heating, washing with
antiseptic soln
Incubation- 3-4 days
Inflam. response->fibrous tissue,
adhesions, scarring
Clinical Manifestations
Men: urethitis, dysuria, purulent disch.
Women: no s/s, vaginal discharge,
dysuria, freq urination, menstr.
changes, red, swollen, purulent urethral
drainage, cervix->abscess, & spreads
Anorectal – no s/s, proctitis, pharyngitis
Complications & Diagnosis
Men: prostatitis, ureth strictures, sterility
Women: PID, Bartholin abscess, ectopic preg,
infertility, DGI- skin lesions, fever, arthritis
Opthalmia neonatorum
Dx: culture of drainage, gram stain, history,
rectal culture, DNA probe technique &
poymerase chain reaction
Drug Therapy
Penicillin
Cipro
Rocephin
Cefixine
Vibramycin
Treat all sexual contacts of pts
Abstain from alcohol & sex. intercourse
Syphilis
Trepomema pallidium
Destroyed by heating, drying, washing
Enters via small breaks in skin or mucous
membrane, needle sharing, contact with
infected lesions, congenital
Incubation: 10-90 days (3 weeks)
Capillary dilation & swelling, proliferation of
endothelium, new blood vessels form, scar
tissue forms when healing
Clinical Manifestations
Primary stage: chancres
Secondary stage: systemic, spread to all
organs, rash, alopecia, adenopathy
Latent period: no s/s, immune system
suppresses infection, + antibodies
Late (Tertiary): gummas, ht failure,
aneurysms, paresis, psychosis, mental
deterioration, ataxia, jt damage
Complications & Diagnosis
Gummas->bone, liver, skin damage
Cardiovascular – ruptured aneurysms,
scarring of aortic valve
Neurosyphilis – sudden pain anywhere
in body, mental changes, ataxia, vision
loss, prob walking
Dx: H&P, dark field microscopy of lesion
scrapings, VDRL, RPR
Drug Therapy
Treatment can not reverse damage
IV Penicillin
Doxycycline, tetracycline, erythromycin
Treat maternal syphilis before week 18;
treatment in 2nd half preg-> premature
labor
Neurosyphilis – management also
depends on neuro s/s
Chlamydial Infections:
Urogenic Infections
Chlamydia trachomatis, many strains
Urethitis & cervicitis, assoc with
gonococcal infections, incub:1-3 weeks
S/S: urethitis, epididymitis, proctitis,
cervicitis, freq urination, barthinitis,
PID, perihepatitis
Complic: infertility, Reiter’s disease, PID,
ectopic preg
Diagnosis & Care
Dx: exclude gonorrhea – smear of ureth
discharge(men), first catch urine,
culture, nonculture tests
Drugs: Vibramycin, Zithromax, Floxin
If pregnant: Erythromycin, Amoxicillin
Follow up care, treat partners, use
condoms, if s/s persist seek care
Lymphogramuloma Vernereum
Stain of C. trachomatis, chronic STD
Africa, India, SE Asia, Caribbean, S America
Enter skin & m membrane via abrasion,
spread via bld & enters CNS
Penile, anal, vulvar infection, ing & fem lymph
enlargement,necrosis, abscesses, fibrosis,
lymph node dysfunction, complic – fistulas
Rx: pt & partner, tetracycline
Genital Herpes
Herpes Simplex Virus (HSV)
HSV-1: infection above waist
HSV-2: genital tract & perineum
Dormant on sensory nerve ganglion
Recurrences: HSV moves down nerve axion
to skin or mucous membrane
Virus enters thru mucous membrane or
breaks in skin.
Viral shedding in absence of lesion
Incubation: 1-45 days, (ave. 6)
Clinical Manifestations
Initial burning tingling
Vesicular lesion on penis, scrotum, vulva,
perineum, perianal, vagina, cervix
Rupture, ulcer, crust, epithelialization
Pain, fever, headache, malaise, myalgia,
lymphadenopathy
Dysuria, retention, vag discharge
Lesions last 17-20 days, new dev 6wks
Clinical Manifestations:
Transmission of HSV
Transmission with or without lesion & if
asymptomatic
Barrier contraception decreases
transmission
Avoid sex when lesion present
Antiviral agents reduce but not prevent
viral shedding
Complications & Diagnosis
CNS- aseptic meningitis, lower neuron
damage
Virus spread to fingers, lips, breast
HSV & pregnancy – hi risk transmission
to infant, C- Section
Dx: s/s, history, culture
Care & Drug Therapy
Wear loose cotton underwear, keep
lesions dry, hairdryer, good hygiene, sitz
bath, pour water when urinating
Health promotion: use condoms,
abstain from sex if have lesions
Pain: lidocaine, codeine, ASA
Zovirax, Valtrex, Famvir
Condylomata Acuminata:
Genital Warts
Human papilloma virus (HPV), highly
contagious, incubation 1-6 mo
Single, multiple growths, grow rapidly
during preg, may transmit to baby
Link with cervical & vulvar cancer & in
men anorectal & penile cancer
Dx: by appearance of lesion, Virapap
Tx: remove symptomatic warts
Nursing Management of STDs
Assessment
Health promotion: “safe sex”, teaching
pt with STD, screening cervical cancer &
STDs, case finding, community educ
Acute care: psychol support, explain tx
& s/e, follow up rx, teach hygiene,
abstinence from sex
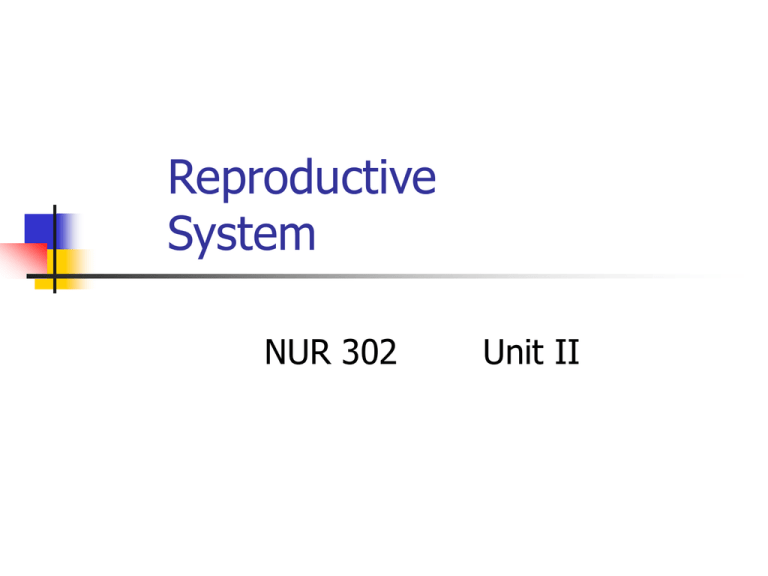
Breast Disorders:
Health Promotion Practices
Risk factors for breast cancer
Monthly breast self exam over age 18
Physical exam q3yrs age 20 – 40 & over
40 q year
Mammography
Follow up care
Assessment of Breast
Disorders
Males: 1% breast cancer, gynacomastia
Breast cancer mostly post menopause
Family history significant
Assess: pain, nipple discharge, lump
size, location, rate of growth,
correlation with menstrual cycle,
consistency, mobility, shape, single or
multiple ducts, one or both breasts
Diagnostic Studies
Mammography
Biopsy – only definitive dx for cancer
Fine needle aspiration
Open surgical biopsy
Stereotactic core biopsy
Benign Breast Problems
Mastalgia – Pain, coincides with menstrual
cycle
Mastitis – inflammation, lactating women,
staph via cracked nipple, fever, red, warm,
tender, continue breast feeding , use shield or
express milk
Lactational breast abscess – no response to
antibiotics, I&D, C&S, express & discard milk
Fibrocystic Changes
Benign, excess fibrous tissue, cyst, pinches
nerve endings->pain
No risk for cancer, nodules in bilateral upper
outer quadrant
Common age 35 – 50, response to estrogen
& progesterone
Lump well rounded, delineated, movable,
enlarge with menstrual cycle
DX: mammogram, ultrasound
Fibrocystic Changes
Aspirate or biopsy esp if hi risk for
breast cancer
Teach breast self exam, follow up
exams thu life, report new lumps or
changes
Wear good bra, lo salt diet, decrease
chocolate & caffeine, diuretic,
hormones, vit E, Danazol, decr stress
Fibroadenoma
Benign, cause of breast tumor in
women under 25, African Americans
Increased estrogen sensitivity
Small, painless, round, movable, soft or
rubbery, slow growth, no relation to
cycle but increase if pregnant
Dx: biopsy, tx- excision
Teach self breast exam, follow up
Benign Breast Problems
Nipple discharge – milky,serous, bloody,
green, brown
Intraductal papilloma – warts in
mammary ducts
Ductal ectasia– peri & postmenopausal,
sticky, multicolored discharge, burning,
itchy, bloody discharge, nipple
retraction, abscess
Gynecomastia
Male enlargement of one or both
breasts, benign
Imbal of androgen & estrogen, can be
s/s of other problem
Pubertal gynecomastia – age 1317,disappears 4-6 months
Senescent gynecomastia
Breast Cancer
Risk Factors
Female, age 50 or over
Family history
BRCA-1, BRCA-2 gene mutations
H/O breast, colon, endometrial, ovarian cancer
Early menarche
Full term pregnancy after age 30, nulliparity
Benign breast disease with atypical epithelial
hyperplasia
Obesity after menopause
Exposure to ionizing radiation
Clinical Manifestations
Lump
commonly found in upper outer quadrant
hard, irreg shape, not delineated
fixed, nontender
Dimpling of skin
Nipple discharge, retracted nipple
Orange peel skin
Diagnostic Studies
Mammography
Ultrasound
Biopsy
Fine needle biopsy
Stereotactic core biopsy
Axillary lymph node status – 4 or more +
nodes ->greatest risk of recurrence
Lymphatic mapping & sentinel lymph node
dissection
Types of Breast Cancer
Ductal cancer
Lobular cancer
Insitu vs invasive
Paget’s disease – malignant persistent
lesion of areola & nipple
Inflammatory breast cancer – rare,
most malignant, red, warm, orange peel
or hives look
Prognosis Variables
Tumor size & differentiation
Axillary node involvement
DNA content analysis
Genetic marker HER-2/neu (c-erb-B2 or
neu)
Estrogen & progesterone receptor
status
Cell proliferation indices
Collaborative Care
TNM Classification: size of tumor, nodal
involvement, metastasis -> staging 0-IV
Breast conservation surg (lumpectomy) with
radiation
Modified radical mastectomy with/out
reconstruction
Axillary node dissection
Follow up care rest of life- reoccurrence at
surg site or opposite breast
Recurrence & Metastasis
Local – skin
Regional – lymph nodes
Distant metastasis
Skeletal
Spinal cord
Brain
Pulmonary
Liver
Bone marrow
Radiation Therapy
Primary radiation therapy – after tumor
removed, external beam, s/e
esophagitis, tracheitis, fatigue, skin,
breast edema
Radiation as adjunct to therapy- pre-op
Palliative – rx of metastasis to bone,
brain, chest, soft tissue, relieves pain,
decrease reoccurrences
Chemotherapy
Very responsive to chemo
Combinations of drugs- effects on cell
growth & division at different stages
Cytoxin, 5FU, Vincristine & Prednisone
Andriamycin, 5FU, Taxol, Taxotere
S/E: GI tract, bone marrow, hair
Hormonal Therapy
Estrogen can promote growth of breast
cancer
Oopherectomy, adrenalectomy,
hypophysectomy
Determine estrogen & progesterone receptor
status of tumor
Tumor regression with hormone manipulation
Tamoxifen, Toremifene, Arimidex
Nursing Care: Breast Cancer
Psychol support during dx & tx
Provide info on tx choices, diag tests
Pre-op teaching
Help restore arm function on affected
side- elevate, finger/arm exercises
Lymphedema- arm never dependent, no
BP, bld work, or injections
Pain, fear, body image disturbance
Nursing Care: Breast Cancer
Reach to Recovery Program
Accurate answers to questions
Teach follow up care
Report fever, inflammation, redness, swelling,
weakness, new pain, SOB
Prosthesis, breast reconstruction
Implications on sexual identity
Depression
Mammoplasty
Surgical change in breast size or shape
Breast augmentation – saline implants
Breast reduction
Post-op – drains, observe s/s
hemorrhage or infection, wear good
supporting continuously for 2-3 weeks,
no strenuous exercise
Ovarian Cancer
Risk factors: family history, hi fat diet, age,
BRCA-1 gene mutation
Protective: mult preg, breast feeding, preg at
early age
Asymptomatic early, pain, increase in
abdomen, ascites, bowel & bladder prob
Dx: CA-125, yrly exam, ultrasound
Rx: total hysterectomy, chemo, radiation
Nursing Implementation
Health Promotion: routine screening, teach
risks for cancer
Psychological support - grieving
Hysterectomy- vaginal or abdominal
Mod amt blding 1st 8 hrs, urinary retention,
abd distention, menopause, thrombophlebitis
Discharge: no lifting, brisk walking, dancing,
can swim, no menses, 4-6 wks no sex
Endometrial Cancer
Risk factor- unopposed estrogen, incr age,
obesity, hi BP, DM
Adenocarcinoma common, grows slow, mets
late, early dx & tx-> + prognosis
Mets to liver, lung, bone,brain
S/S: abnormal uterine bleeding
Dx: endometrial biopsy; tx total
hysterectomy, radiation, progesterone, chemo
Cervical Cancer
Slow progression, repeated cervical injury;
HPV with smoking
No s/s early, leukorrhea, intermenstral blding,
anemia, wt loss, cachexia
Dx: Pap test, Schiller iodine test, biopsy,
colposcopy
Rx: classII- 3-4mo follow up, class III>
biopsy, conization; invasive- hysterectomy,
radiation
Pelvic Inflam. Disease (PID)
Untreated cervicitis ascends; may involve
fallopian tubes, ovaries, pelvic peritoneum
S/S: lower abdom pain, spotting, vag
discharge, fever
Dx: s/s, pelvic exam
Complications: septic shock, Fitz-Hugh Curtis
symdrome, abscess, peritonitis, emboli
Long term: ectopic preg, infertility, chr pain
PID: Collaborative & Nsg Care
Antibiotics, no sex 3 wks, BR- Semi Fowler’s
position, fluids, exam partners, repeat exam
48-72 hrs, analgesics
Prevention- teach risk factors, early recog &
tx cervicitis
Monitor pain, heating pad lower abd, sitz
bath, teaching prevention- barrier methods,
reason for BR, VS, monitor vaginal discharge
Benign Tumors
Leiomyomas (fibroids, myomas)
S/S: none, heavy blding,abd pressure
Rx: observe over time, surgery
Cervical polyps:cherry red, soft, seen on
pelvic exam. Rx: excise
Benign ovarian tumors: cystic &
neoplasms; <8cm or solid->laporoscopy
Problems with Pelvic Support
Uterine prolapse-uterus into vagin.canal
Cystocele- weak bet bladder & uterus
Rectocele- weak bet uterus & rectum
Rx: Kiegal exercises, pessary, surgery
Post-op care: perineal care 2x day & after
urination, ice pack, later heat
Discharge: laxatives, douches, no lifting, long
sitting, standing, no sex til MD oks
Male Reproductive Problems
Benign Prostatic
Hypertrophy(BPH)
BPH etiology &
pathophysiology
Increase in epithelial cells in prostate,
does not predispose to prostate cancer
Age related endocrine changes
Dihydroxytestosterone, estrogen
Inner part of prostate enlarges->
compresses urethra->obstruction
Risk factors – family history, diet with
zinc, butter margarine
BPH Symptoms
S/S: gradual, decr in force of urinary
stream, hesitancy starting, end dribble,
feeling of retention, nocturia, urgency
Irritation due to infection – frequency,
nocturia, dysuria, incontinence
BPH Diagnosis
Digital rectal exam – symmetrical, enlarged,
smooth
U/A with C/S
PSA(Prostate Specific Antigen) r/o prostate
cancer
Creatinine
Transrectal ultrasound with biopsies –r/o
cancer
Cystoscopy, uroflow
Treatment – Conservative
(based on s/s)
Watch & wait, diet decrease caffeine, artificial
sweeteners, avoid cold meds &
anticholinergics, restrict fluids at nite
Meds – Proscar blocks enzyme to convert
dihydroxytestosterone to testosterone
Alpha adrenergic recteptor blocker->relax
smooth muscle –Cardura, Hytrin, Flomax
Herba – saw palmetta
BPH Treatment
Nonsurgical: intermittent cath, foley,
coils, stents, balloon dilatation, TUMA
Surgery: laser ablation, TURP, TUIP,
suprapubic resection, retropubic
resection, perineal resection
Complications: hemorrhage, infection,
bladder spasm, urinary incontinence,
erectile problems
Treatment - Invasive
Transurethral resection of prostate
(TURP)
Transurethral microwave thermotherapy
Transurethral needle ablation (TUNA)
Transurethral electrovaporization of
prostate
Laser prostatectomy
Urethral stents
BPH Nursing Care
Health promotion: age 40 yrly medical
history, >50 & s/s diagnostic screening
Avoid sudafed, phenylephrine, caffeine,
alcohol
Void every 2 hrs, maintain fluid Intake
Pre-op Care
Relieve obstruction – c oude (curved) cath,
fillifrom (rigid) cath, lidocaine as lubricant
Antibiotics if infection
Restore drainage with foley, hi fluid intake
Address sexual concerns – all procedures
result in retrograde ejaculation so ejaculation
diminished, semen eliminated when pt voids
Post-op Care BPH
3 way foley with CBI
Read text p1442-1443 !!
Maintain patency of foley, aeseptic technique
Blood clots are expected 24-36 hrs BUT bright red
blood not-> hemmorrhage
Bladder spasms
Sphincter control poor>dribbling, incontinence
Check for s/s
Infection
Stool softeners
BPH Home Care
Discharge Teaching
S/S infection
Urinary incontinence
Avoid lifting
Avoid constipation
Fluid intake 2000-3000cc
Address sexual questions
No driving or sex til cleared by MD
Follow up with MD
Prostate Cancer
Most common cancer among men excluding
skin cancer
Risk factors – age, family history, African
American, hi fat diet, exposure to chemical
cadium
Incidence increases at age 50, 80% mostly
65 & older
Androgen dependent cancer
Outer aspect prostate gland
Spreads direct extension, by lymph or blood
Prostrate Cancer
Slow growing, spreads via lymph, blood,
direct extension to lungs, liver, head of
femur, pelvic bones, lower spine
Pain – problem after metastisis
S/S: none early, BPH s/s, pain down legs +
urinary s/s->metastasis
Dx: screening with PSA, rectal exam->
asymmetrical, large, nodules, biopsy, CT
scans for metastasis
Radical Prostatectomy
Remove all prostate, seminal vesicles, neck of
bladder
Long term survival, use for men under 70, good
health, no metastasis
Retropubic approach or perineal resection
Post-op – foley in urethra with 30cc balloon, left 2
weeks and drain in incision site
Complications – erectile dysfunction & incontinence
Nerve sparing procedure can preserve erectile
function
Conservative Treatment
Slow growing, may defer tx, watch and
wait
Life expectancy Less 10 yrs
Comorbid disease
Low grade, low stage tumor
Followed with PSA, rectal exams
Collaborative Care
TURP or total prostatectomy
Radiation: external beam radiation,
seed implants (brachytherapy)
Drug therapy: antiandrogen therapy –
Lupron, Zoladex, Casadex, Proscar
Orchidectomy or estrogen therapy
(diethylstilbestrol)
Prostatic cryotherapy
Prostatitis
Bacterial, chr. bacterial, nonbacterial,
prostatodynia
S/S bacterial: fever, chills, dysuria,
urethral disch, low rectal, back, pelvic
pain, post ejaculation pain, prostrate
swollen, tender, warm, firm
Dx: s/s, WBC, u/a
Tx: antibiotic, Cipro, analgesics
Testicular Cancer
Age 20-40, had undescended testes, family history,
germ cell tumors
Dx: palpation, sonogram, MRI, blood markers-AFP
(alpha fetoprotein) &hCG (human chorionic
gonadatropin),orchidectomy & staging of tissue
S/S: lump, feeling of heaviness, swelling
Teach self exam, radical orchidectomy
Discuss sperm banking, potential to interfere with
erections & fertility
Metastasis – back pain, cough, dysphagia, seizures,
alterations vision