Pediatric Transfusions - Keck School of Medicine
advertisement
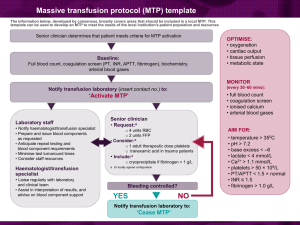
Transfusion Medicine Cynthia H. Ho, M.D. July 2012 Introduction Average volume of blood in an adult is 5 liters. Volume of blood products Packed red blood cells (PRBCs): 250-350 mL per unit. Fresh frozen plasma (FFP): 250–300 mL per unit. Platelets: 40–50 mL per unit (single donor), 250-350 mL per unit (pheresis). Cryoprecipitate: 10–12 mL per unit. Red Blood Cells RBC antigens are polymorphic, inherited, carbohydrate or protein structures on RBC membranes. Immunization against blood group antigens occur through transfusion, pregnancy, and needle sharing. What is in a bag of donor blood? Anticoagulants Citrate Heparin Preservatives Citrate Adenine Dextrose Byproducts of RBC Storage Citrate Causes hypocalcemia when patients are given large volume transfusions. Potassium Na/K pump inactivation. Hemolysis. Microaggregates of platelets, WBCs, fibrin can cause pulmonary edema. Red Blood Cells One unit of PRBC will increase Hgb by 1g/dL and increase Hct by 3%. Indications for transfusion Acute blood loss: Depends on 1) risk of tissue hypoxia, 2) symptoms, 3) ongoing blood loss, 4) planned interventions, 5) hemoglobin. Chronic anemia: Hgb is low but plasma volume is normal. Treat underlying illness first. Critical illness: Consider at Hgb<7.0. Sickle cell disease: Acute chest syndrome, stroke, perioperative. Chemotherapy-related anemia: Consider at Hgb<8.0. Perioperative Transfusions Blood loss <10% blood loss – usually no need for transfusion. 10-20% blood loss – crystalloids usually sufficient for resuscitation. >25% blood loss – blood products usually indicated. No clear cut off, but consider at Hgb<7g/dL. More important to individualize to your patient. Coronary artery disease – most cardiologists suggest transfusion at Hgb<10g/dL (no studies to support this practice). Red Blood Cells Packed Red Blood Cells (PRBC) Component of choice for replacement. Leukocyte-reduced PRBC Filtered to remove most WBCs. Decreases risk of alloimmunization, transmission of viruses (including CMV), febrile non-hemolytic transfusion reactions. Transplant patients, history of febrile nonhemolytic transfusion reactions, transfusion-dependent chronic anemia, patients receiving chemo or XRT. Irradiated blood Avoids Graft vs Host disease. Transplant patients, immunodeficiency, neonates, patients receiving chemo or radiation therapy. CMV negative Transplant recipients. consider in potential transplant patients. Red Blood Cells Platelet Transfusions Whole blood derived platelets contain 50mL plasma and platelets from 5-6 donors per unit. Apheresis units are from a single donor. More expensive. Circulate longer (gentle handling). Exposure to fewer donors. Decreased risk of infections. Decreased alloimmunization risk has not been substantiated. Platelets One unit raises platelet counts by 5,000-10,000/uL. Give over 20-30 minutes (~10mL/min). Keep >50,000 for bleeding patients. Consider keep >100,000 for intracranial hemorrhage. Prophylactic Platelet Transfusions Studies of prophylactic transfusions in leukemia patients with platelet counts of 10,000 versus 20,000 showed no increased risk of bleeding when 10,000 used as cutoff. Prior to invasive procedures – no randomized trials Lumbar puncture – 10,000. Central lines – 20,000-30,000. Prophylactic Transfusions Prior to Surgery For most surgeries – Keep platelets > 50,000 – based on retrospective studies. For neurosurgery, retinal surgeries – Keep platelets> 70,000-100,000 – based on tradition, no studies. Adverse effects of platelet transfusions Increased risk of bacterial infections compared with other blood products. Stored at room temperature for 5 days maximum. 1 in 3,000 platelet units have bacterial contaminant. Clinically apparent bacterial infections occur in 1 in 25,000 transfusions. Allergic and febrile nonhemolytic transfusion reactions. Hemolytic transfusion reactions. TRALI Rh(D) sensitization Platelet Refractoriness Non-immune causes Fever Sepsis Bleeding Splenomegaly DIC Immune causes Antibodies against HLA or platelet specific antigen (HPA) ABO incompatibility Platelet Refractoriness Suspect immune cause if 18-24 hour posttransfusion platelets increased by less than 5,000. Check post-transfusion platelets 10 minutes to 1 hour after transfusion. >5,000-10,000 rise suggests non-immune mediated cause. <5,000-10,000 rise suggests immunemediated cause. Contraindications to platelet transfusions TTP ITP HIT Aplastic anemia MDS ***Unless life-threatening bleeding. Plasma Acellular component of blood 90% water 7% protein and colloids 2-3% nutrients, crystalloid, hormones, and vitamins Proteins – Fibrinogen, vWF, protein C, protein S, and soluble clotting factors (V,VII,IX,XI). Plasma Give transfusions over 20-30 minutes. One unit is 200-280mL. Give 8-10mL/kg. If critically ill, give 30mL/kg. Plasma FFP is frozen at -18°C or colder within 6 hours of collection. Can be stored for one year. Thawed over 20-30 minutes. F24 is most commonly used in the U.S. Frozen within 24 hours of collection. Virtually equivalent to FFP except decreased amount of fibrinogen, factors V, VIII, and XI. Indications for plasma transfusion Give over 20-30 minutes (~10mL/min). Bleeding associated with clotting factor deficiencies, prior to invasive procedures, reversal of warfarin. Adverse reactions to Plasma transfusions Febrile non-hemolytic and allergic reactions. TRALI. Anaphylaxis (IgA deficiency). Infections. Cryoprecipitate Contains Factor VIII, fibrinogen, fibronectin, von Willebrand's factor and Factor XIII. Give 2-10 units for every 10 kg -> will raise fibrinogen 60-100 g/dL. Indications: Bleeding associated fibrinogen deficiency (<100), e.g. DIC. Transfusion-related labs Type and cross: Matches patient's blood to specific donor units. Type and screen: Tests patient's serum for common antigens. Good for 72 hours. Direct Coomb’s DAT: Tests if patient's cells are IgG or complement coated (e.g. hemolytic transfusion reactions, autoimmune hemolytic anemia). IN VIVO. Indirect Coomb’s: Tests patient's serum with common antibody (other than ABO) to RBC's (e.g. autoimmune hemolytic anemia, delayed hemolytic transfusion reaction). IN VITRO. Pre-Transfusion Medications Fever from a transfusion is usually due to febrile nonhemolytic transfusion reaction and responds to antipyretics. However, fever can also occur with bacterial contamination or more serious transfusion reactions (TRALI). Therefore, do not routinely pre-treat with acetaminophen. Unless the patient has a history of allergic reactions or shows signs of an allergic component to a febrile non-hemolytic transfusion reaction (flushing, hives, or pruritus) there is no benefit from the use of antihistamines for febrile reactions. Diphenhydramine should be reserved for pretreatment or treatment of possible allergic reactions in patients who have had a history of a mild allergic reaction. Labs after Transfusion In the absence of increased red blood cell destruction or sequestration, the expected rise in Hgb is usually not measurable until 24 hours after transfusion, when the plasma volume has had time to return to normal. Checking platelets 1-2 hours after transfusion may be helpful to determine if platelets increase appropriately or if possible alloimmunization has occurred. When to draw post-transfusion labs depends on what your goal is, anticipated ongoing losses, anticipated procedures (anesthesia), etc. Transfusion reactions Hemolytic transfusion reactions Febrile non-hemolytic transfusion reactions Allergic transfusion reaction Bacterial contamination TRALI Circulatory overload Anaphylaxis Post-transfusion purpura Graft versus host disease Hypothermia Electrolyte abnormalities Febrile Non-hemolytic Transfusion Reaction Increase in temperature by 1°C with no other explanation. Antibody-leukocyte or antibody-platelet reactions -> cytokine release -> fever. Fever and chills usually occur shortly after a transfusion has begun. Less common, but fever and chills can occur hours after transfusion. Usually resolves after 8-10 hours. What to do if your patient has a fever during a transfusion Stop the transfusion R/o hemolysis Confirm patient and donor blood type Repeat type and cross Evaluation for hemolysis – BMP, CBC, LFT, LDH, DAT, haptoglobin, U/A with microscopy R/o infection Examine your patient, consider blood culture is bacterial contamination suspected. Treatment Tylenol. Consider hydrocortisone for patients with history of severe FNTR with fever despite Tylenol. Consider demerol for patients with significant chills from FNTR Allergic Transfusion Reaction Can present as urticaria, pruritis, vasomotor instability, bronchospasm, anaphylaxis. Most common presentation is pruritis followed by urticaria. Due to antibodies (IgE or other) against donor plasma proteins. Severity is not dose related. Common – occurs in 1% of transfusions. Treatment – stop transfusion, give 25-50mg diphenhydramine, monitor. Restart transfusion if urticaria gone. Do not restart transfusion if patient has fever, bronchospasm, dyspnea, hypotension, tachycardia. Bacterial Contamination Contamination occurs from skin at the time of collection. Some bacteria grow optimally at room temperative but others grow optimally under refrigeration (Pseudomonas, Yersinia, Enterobacter, Flavobacterium). Presents with fever, rigors, skin flushing, abdominal cramps, myalgias, DIC, renal failure, cardiovascular collapse (warm shock). Bacterial Contamination Treatment Stop transfusion, check labs (r/o acute intravascular hemolysis) Send culture of donor blood Start broad spectrum antibiotics Between 1998 and 2000 Transfusion transmitted bacteremia 9.98 per million single donor platelets 10.64 per million pooled platelets 0.21 per million RBC units Fatal reactions 1.94 per million single donor platelets 2.22 per million pooled platelets 0.13 per million RBC units Transfusion Related Acute Lung Injury Occurs in 1,000 to 5,000 transfusions. Range in presentation - mild dyspnea, desaturation, fever, chills, hypotension, respiratory failure. CXR with acute development of bilateral infiltrates. Develops within 1-6 hours of transfusion. Non-cardiogenic pulmonary edema (PCWP<18). Circulatory Overload More common among elderly and patients with predisposition to volume overload (renal failure, CHF). As a general rule, unless a patient is actively hemorrhaging, do not transfuse faster than 23mL/kg/hour. Slowest rate of transfusion in 4 hours per unit of PRBC. Can ask blood bank to give blood in smalller aliquots if needed to slow down the rate further. Post-transfusion Graft versus Host Disease Occurs in bone marrow transplant patients. Immunocompetent donor WBCs attack host tissues. Fatal in 90% of cases. Occurs 8-10 days after transfusion. Pancytopenia, rash, liver test abnormalities, multiorgan failure. No effective treatment. Irradiated leukocyte reduced PRBC decreases risk of GVHD. Post-transfusion Purpura Rare, self-limited cause of thrombocytopenia after transfusion. Patients with history of exposure to platelet specific antigen (usually PLA1) that they lack form an antibody. With subsequent exposure to the platelet specific antigen, the antibody destroys donor platelets and triggers an autoimmune response to host platelets as well. Treatment – IVIg, plasma exchange, steroids, splenectomy. If bleeding and transfusion needed, give platelets without the platelet specific antigen that the host is lacking. Risk of Transmission of Viral Infections HBV – 1 in 137,000 HCV – 1 in 1,000,000 HIV – 1 in 1,900,000 Type Signs/Symptoms Treatment Acute hemolytic Fever, chills, back pain, hypotension, intravenous site burning, pallor, jaundice, dark urine. •Occurs during or immediately after transfusion. •Evidence of immune-mediated hemolysis (DAT positive, indirect hyperbilirubinemia, high LDH, low haptoglobin, elevated retic, urine dipstick positive blood without RBC) •Stop transfusion, maintain BP & volume. Delayed hemolytic Pallor, jaundice, fever. •Occurs days to weeks after transfusion. •Evidence of immune-mediated hemolysis (DAT+). •Stop transfusion, monitor for severe hemolysis, send pink top tube to blood bank. Non-immune hemolytic Pallor, dark urine. •Evidence of hemolysis (DAT negative). •Stop transfusion, supportive treatment. Febrile nonhemolytic Fever, chills, malaise. •Once hemolysis ruled out, give anti-pyretics. Allergic reaction Hives, rash, pruritis, wheezing, anaphylaxis. •Hold transfusion, monitor for signs of more serious allergy, give diphenhydramine. •If rash only, should resolve in 30 min after treatment and can resume transfusion. •This is the only reaction that a transfusion reaction workup does not need to be sent. Anaphylaxis or Anaphylactoid Sudden onset flushing, wheezing, and hypertension followed by hypotension, edema, respiratory distress, and shock. •No evidence of incompatibility (DAT negative). •Watch for DIC, ARF, respiratory failure, hyperkalemia. •Stop transfusion, give 1ml/kg im epinephrine (0.01mg/kg) of 1:1000 solution. •Hydrocortisone 1mg/kg iv. •Maintain BP and volume, consider dopamine, O2. •Consider IgA deficiency. -1- LAC+USC HEALTHCARE NETWORK Practice Parameters For Transfusion of Blood Products (For Adult Patients) RED BLOOD CELLS I. ACUTE BLOOD LOSS 1. Evaluate for risk of ischemia Usually Needed Acute blood loss >30% to 40% Hb <6g/dL 2. Estimate degree of blood loss 3. Measure hemoglobin Gray Zone (30%-40% rapid blood loss) Transfuse based on clinical assessment (vital signs, EKG changes etc.) Hb = 6-10 g/dL Usually Not Needed Acute blood loss <30 to 40% in previously healthy person Hb >10g/dL II. CHRONIC ANEMIA 1. Treat with specific pharmacologic agent (B12, iron, folate, erythropoietin) 2. Transfuse to minimize symptoms and risks of anemia (typically at Hb 5-8g/dL range) III. DO NOT TRANSFUSE RBC 1. For volume expansion only 2. In place of specific pharmacologic therapy 3. To enhance wound healing PLATELETS I. THERAPEUTIC TRANSFUSION - Patients with active bleeding or high-risk of bleeding at major surgery, and normal platelet function Usually Needed <50,000/uL II. Gray Zone (50,000 -100,000u/L) Transfuse based on patient’s risk for more significant bleeding PROPHYLACTIC TRANSFUSION - Stable patient with intact vascular system and normal platelet function Usually Needed <10,000/uL III. IV. Usually Not Needed >100,000/uL Gray Zone (10,000 - 50,000u/L) Transfuse based on patient’s risk for more significant bleeding Usually Not Needed >50,000/uL Platelet transfusions at higher counts may be needed for patients with platelet dysfunction DO NOT TRANSFUSE PLATELETS - Patients with ITP, TTP, and/or Heparin Induced Thrombocytopenia unless there is clinically significant bleeding or significant surgical challenge FRESH FROZEN PLASMA (FFP)/THAWED PLASMA THERAPEUTIC TRANSFUSION - Usually Needed I. · · II. Urgent reversal of warfarin therapy when patient requires emergency major or CNS surgery or is bleeding. A second dose may be required after 4-6 hours due to the short half-life of Factor VII. Treatment of acute TTP or HUS · Severe trauma with massive bleeding PROPHYLACTIC TRANSFUSION Usually not needed for prophylaxis when both INR is <1.7 and PTT is <45 seconds III. DO NOT TRANSFUSE FFP/THAWED PLASMA · · When coagulopathy is correctable more effectively with specific therapy (Vitamin K, FVIII or FIX conc.) For volume expansion · As a nutritional supplement CRYOPRECIPITATE Usually Needed · Factor XIII deficiency · Fibrin glue · · Fibrinogen deficiency Active DIC · Dysfibrinogenemia References: 1. Anesthesiology 1996;84:732-743 2. Arch Pathol Lab Med 1998;122:130-138 3. Transfusion 1998;38:796-797 4. Am J. Clin Path 2006;126:133-139 Approved: August 26, 2008 (Blood Utilization Committee) Summary RBC transfusions Platelets Transfuse for bleeding patient with decreased clotting factors. Cryoprecipitate One unit increases platelets by 5,000-10,000. Check platelets after 1 hour if concern for immune mediated cause of refractoriness to platelet transfusion. Plasma One unit increases Hgb by 1g/dL. Give over 2-3mL/kg/hour, slowest is one unit over 4 hours. Leukocyte reduction decreases risk of CMV and FNHR. Irradiation decreases risk of GVHD. Transfuse for bleeding patient with decreased fibrinogen <100. Transfusion reactions Can be acute or delayed, hemolytic or non-hemolytic. Stop transfusion, call the blood bank! Reference Hoffman: Hematology: Basic Principles and Practice, 5th edition. 2008 Churchill Livingstone, An Imprint of Elsevier.