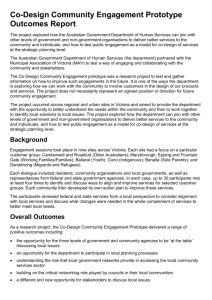
to the presentation - Health Quality & Safety Commission
advertisement
UNDERSTANDING PATIENT, STAFF AND FAMILY EXPERIENCE AND TRANSFORMING CARE THROUGH DESIGN HQSC, Partners in Care, Show & Tell Symposium, June 2014 Lynne Maher and Hilary Boyd 1 PLAN FOR TODAY At the end of the workshop participants will: • Understand how to work closely with patients and staff to co-design health services • Be introduced to a range of tools and methods to support co-design in practice • Recognise the value patients bring to improving quality, safety and experience of care • 2 Know where to go to find out more information I. ABOUT CODESIGN 3 THE CO-DESIGN APPROACH IS... • …about using experience to gain insights from which you can identify opportunities for improvement • 4 …about experiences not attitudes or opinions EXPERIENCE BASED DESIGN IS ABOUT DESIGNING BETTER EXPERIENCES 5 HEALTH SERVICE CO-DESIGN: FRAMEWORK www.healthcodesign.org.nz/about.html 6 HEALTH SERVICE CO-DESIGN PHASES 01 Engage: Establish and maintain meaningful relationships. 02 Plan: Work with patients and staff to establish project goals and how to achieve them. 03 Explore: Capture and understand patient experiences of services and identify ideas for change. 04 Develop: Work with patients to turn ideas into possible improvements. 05 Decide: Decide which improvements to make and how to make them. 06 Change: Implement the changes. www.healthcodesign.org.nz/about.html 7 TERMINOLOGY 8 • Feeling informed and being given options • Patient experience • Patient engagement • Patient involvement? • Patient satisfaction? • Patient- and family-centred care? • PFCC? • Person-centred care? • Co-design? BUT WHY? “We need to move from a service that does things to and for its patients to one where the service works with patients and whaanau to supports them with their health needs.” 9 When you start to work closely with patients to understand their needs and support them to achieve their health goals you cannot go back to your old way of working. 10 “Stories from patients are inspiring, insightful, humbling, uplifting, reassuring and above all remind us of why we are here.” [Liz Goldie, Partners in Care Programme, 2014] 11 “Those that believe patient experience is simply about making people happy have simply missed the point.” [James Merlino, Chief Experience Officer, Cleveland Clinic] 12 POSITIVE PATIENT EXPERIENCE IS ASSOCIATED WITH HIGHER QUALITY CARE Hospitals with high levels of ‘ patient care experience ’ reported by patients provide clinical care that is higher in quality across a range of conditions. [Jha A et al (2008) N Engl J Med 2008; 359:1921-1931] 13 Improved patient experience is positively associated with… • Objectively measured health outcomes • Adherence to medications and treatments • Health resource usage • Technical quality of care & adverse events [Doyle C et al BMJ Open Jan 20, 2013] 14 WE NEED TO MOVE AWAY FROM THIS... 15 WE AS CLINICIANS AND MANAGERS WORRY ABOUT THIS... 16 WE THINK PATIENTS WANT THIS... 17 WHAT MATTERS TO PATIENTS (ENGLAND, 2011) • Feeling informed and being given options • Staff who listen and spend time with me/patients • Being treated as a person, not a number • Being involved in care and being able to ask questions • The value of support services, for example patient and carer support groups • Efficient processes [Robert, Cornwall, Brearley et al., 2011] 18 A QUICK SURVEY What did you think of your journey this morning? A Very Good 19 B C D E Very Poor A QUICK SURVEY 20 • Work in two’s or ‘threes’ • One person tell their story of their journey here today- take 5 minutes • The ‘listeners’ do just that; and particularly ‘tune in’ to any words that could depict emotion. FEEDBACK - TABLES Discuss what was the difference between doing a survey and telling your story. 21 UNDERSTANDING THE NEEDS OF PEOPLE LIVING WITH MULTIPLE SCLEROSIS 22 CONVERSATIONS THAT COUNT How can we encourage conversations about planning for death and dying amongst and in communities so that people can get the care they want at the end of their lives? [Auckland District Health Board] 23 WHAT WE DID • Held several consumer workshops to understand their experiences of advance care planning and find out what they would like done differently. • Received HQSC funding to implement the peer-education idea. • Recruited consumer representatives. • Held four practical co-design workshops to understand how to structure a peer education programme and how the resources would look. 24 • Produced a 52-page modular-based toolkit and a 2-day training package. • Trained 27 volunteers who held 19 community sessions with 172 people. “I found our sessions very enlightening! I was amazed at the many topics we discussed, they truly opened my eyes as to what is available to people facing end-of-life. Not knowing what is available can lead to fear and isolation. It would be wonderful to get this information out to the community so people could make decisions for themselves, how to best look after themselves and face this phase of their life positively without fear.” [Community session participant] 25 II. CO-DESIGN IN PRACTICE 26 If I had an hour to save the world, I would spend 59 minutes defining the problem and one minute finding solutions.” [Albert Einstein] 27 HOW CAN YOU DO THIS? 28 • As a regular way to understand patient and staff experiences • In an area where you have challenges- perhaps where you know you have a number of complaints • As part of an improvement project • All of the time • Looking at services, product design, the technology design, facility design and tackling big issues PUBLIC SPACES PROJECT How can we understand people’s experience of public spaces at Auckland City Hospital? •How staff, patients and visitors use the space •What •How people access care, services and information •What •How people use the space for…existing entry points, foyers and retail spaces kinds of services we provide the entry points, foyers and public spaces work and the qualities they portray [Auckland District Health Board] 29 PUBLIC SPACES DISCOVERY WEEK • A week of discovering what people thought • Developed three new tools for intercept interviews: journey, services and qualities • Over one weekend and three weekdays had teams doing interviews • Two co-design workshops: staff and community • Online staff survey • Daily debriefing sessions to compile results [Auckland District Health Board] 30 HOW CAN WORKING WITH VERY HIGH INTENSITY USERS HELP US SOLVE THE READMISSION PROBLEM? Agnes became unwell and went to the ER. She was admitted to hospital and responded well to treatment. Agnes was discharged home with medications and information. Agnes became unwell and went to the ER. She was admitted to hospital and responded well to treatment. Agnes was discharged home with medications and information. Non-compliant patient? 31 Agnes became unwell and went to the ER. She was admitted to hospital and responded well to treatment. Agnes was discharged home with medications and information. Insanity: Doing the same thing over and over again and expecting different results.” [Albert Einstein] 32 AGNES AND TWO BLUE PILLS 33 "There comes a point you have to stop pulling people out of the river, get upstream and find out why they're falling in." [Desmond Tutu] 34 III. CAPTURE AND ENGAGE 35 ENGAGING PATIENTS AND WHAANAU 36 • You do not need high numbers of patients • Develop information about what you are planning to do and the role patients can play • Use methods of engagement that are relevant to the patient group. • Talk to patients / whaanau and ask if they would like to be involved • Identify patients /whaanau who have recently had cause to complain • Clinical staff might identify patients/whaanau WAYS OF GATHERING EXPERIENCES Collect stories and thoughts from both patients and staff • • 37 • Structured conversations • Shadowing • Still photography and film provides compelling illustration • Creation of story boards • Diaries • Intercept interviews Observe patients and staff delivering and receiving the service OBSERVATION • People do not always do what they say they do • People do not always do what they think they do • People do not always do what you think they do • People cannot always tell you what they need • Observation lets you find out what people really do and need [IDEO, 2006] 38 THE STORY OF THE TOILET ROLL HOLDER 39 INTERCEPT INTERVIEWS One-one-one, short interviews ‘on location’. Useful for gathering immediate impressions of a large number of people. Can be used in conjunction with visual aids. 40 SERVICE SELECTION 41 EXPERIENCE OF SERVICES 42 IV. EXPLORE, UNDERSTAND AND DEVELOP 43 UNDERSTAND THE EXPERIENCE 1. Identify emotions 2. Find the touchpoints 3. Map the emotions (highs and lows) to the touchpoints 44 45 IDENTIFYING EMOTIONS 46 • Watch this film and write down the emotions that the patient talks about. • Write positive emotions above the line and negative emotions below the line. • Remember that they may not be ‘pure’ emotion words but that you are gathering the emotions and memories from the patient story to understand the experience. VIDEO SHOWING EMOTIONS Movie: Sheila shares her experience (1:30) 47 48 EXPERIENCE QUESTIONNAIRE This is a tool that can be used on its own or as a starting point for understanding which part of the pathway you might want to focus on. 49 USING WORDS [Developed by the NHS Institute for Innovation and Improvement; adapted by many.] 50 51 USING SMILEY FACES 52 PERSONAS 53 • A way of describing characteristics of service users through using composite characters. • Personas often developed according to sets of behaviours. • Can be developed as part of analysing the results of interviews or as part of a co-design workshop. • Personas can help us better understand who a product or service may affect. PERSONA EXAMPLE http://precisionmedicine.files.wordpress.com 54 IV. DEVELOP, DECIDE, CHANGE AND IMPROVE [THE CO-DESIGN PART] 55 IMPROVE THE EXPERIENCE Experience based co-design positions patients as active partners with staff in quality improvement.” [Tsianakas et al 2012] 56 IMPROVE THE EXPERIENCE 57 • Involve patients/carers and staff • Create ‘co-design’ teams • Be clear about actions needed and impact desired • Use improvement tools and techniques PLANNING AN EXPERIENCE EVENT • Working in partnerships with patients can create some apprehension, but it has the potential to transform health services 58 • Plan the date in advance • Make sure everyone can get to the event • Use ‘simple English’ • Staff are often as nervous as patients/family members • Staff may try to ‘take control’ facilitation is important • Do not leave without next action steps 59 ACTION PLANNING A personal responsibility. 60 • Hugh McGrath, Patient • Julie, Clinic receptionist • John Pickles, Consultant PROTOTYPING IN ACTION • New Zealand ’ s first advance care planning Conversations that Counts Day. • The 2014 campaign was aimed at active older people. • Rough ideas. • Workshop at a retirement village. • Groups to select a pre-prepared persona and develop a prototype campaign postcard including the slogan, images and format. • Groups were then asked to pitch their postcard ideas. [Auckland District Health Board] 61 THE FINAL RESULT 62 V. CHANGE AND MEASURE 63 THE QUANTITATIVE PERSPECTIVE Reduction in Time • Reduction in duplication • Reduction in steps Increase in Safety: reduction in error and cost Improve Patient Experience • Reduction in handoffs • Reduction in complaints Increase in Effectiveness • 64 Adherence to standards/protocols; reduction in variation MEASURING What matters more than raw data is our ability to place these facts in context and deliver them with emotional impact.” [Daniel Pink, A whole new mind, 2008] 65 USING QUANTITATIVE AND QUALITATIVE REPORTING TOGETHER 66 NOTHING ABOUT ME WITHOUT ME 67 LEARN MORE • Co-design in Healthcare networking website: http://codesign.hiirc.org.nz • Design for Health and Wellbeing lab: http://dhwlab.com/ • Toolkit and website: www.healthcodesign.org.nz • Consumer engagement: www.hqsc.govt.nz/our-programmes/consumer- engagement/ 68 LEARNING FROM THE NEXT GENERATION Movie: Trevor Torres has Diabetes (4:42)) 69 70 PLAN FOR TODAY At the end of the workshop participants will: • Understand how to work closely with patients and staff to co-design health services • Be introduced to a range of tools and methods to support co-design in practice • Recognise the value patients bring to improving quality, safety and experience of care • Know where to go to find out more information Did we achieve this? 71 SUGGESTED READING • Bate P, Robert G (2006) Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care 15(5):307–310 • Bessant, J. Maher, L. (2009) Developing radical service innovations in healthcare – the role of design methods. International Journal of Innovation Management. Vol. 13, No 4. • Boyd, H., McKernon, S., Mullin, B., & Old, A. (2012). Improving healthcare through the use of co-design. Journal of the New Zealand Medical Association,125(1357). • Davies E, Cleary D (2005) Hearing the patient’s voice? Factors affecting the use of patient survey data in quality improvement. Qual Saf Health Care 14:428–432 • Department of Health (2013) Report of the Mid Staffordshire Public Enquiry www.officialdocuments.gov.uk or www.midstaffspublicinquiry.com 72 73 • Dewar B, Mackay R, Smith S, Pullin S, Tocher R (2010) Use of emotional touchpoints as a method of tapping into the experience of receiving compassionate care in a hospital setting. J Res Nurs 15 (1):29–41 • Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3:e001570. • Goodrich J, Cornwell J (2008) Seeing the person in the patient. The King’s Fund, London • Iedema R,Merrick E, Piper D, Britton K, Gray J, Verma R,Manning N (2010) Co-design as discursive practice in emergency health services: the architecture of deliberation. J Appl Behav Sci 46:73–91 • Maben J. Adams M. Peccei R. Murrellst. & Robert G. (2012) ‘Poppets and parcels’: the links between staff experience of work and acutely ill older peoples’ experience of hospital care. International Journal of Older People. Nursing 7, 83–94 74 • Maher L. (2013) Smart Guide to Developing Pathways – Using patient and carer experience. NHS Networks Accessed via . http://www.networks.nhs.uk/nhs-networks/smart-guides • Maher, L. (2011) Untapped Resource. Public Servant Journal. September 2011. • Reeves et al. Facilitated patient experience feedback can improve nursing care: a pilot study for a phase III cluster randomised controlled trial. BMC Health Services Research 2013, 13:259. http://www.biomedcentral.com/1472-6963/13/259 • Schaeper, J. Maher, L. Baxter, H. (2009) Designing from within- embedding service design into the UK health system. Touchpoint- The Journal of Service Design. Vol. 1, No 2. • Tsianakas, V. Robert, G. Maben, J. Richardson, A. Dale, C . Wiseman, T. ( 2011) Implementing patient-centred cancer care: using experience-based co-design to improve patient experience in breast and lung cancer service. Support Care Cancer with open access at Springerlink.com TABLE TASK 75 • In groups, get a piece of A1 paper and draw a vertical line in the middle of your paper • On the left hand side of the line list what tools and techniques are you using to capture patient experiences • For each item on your list, discuss what you have done with the information you learnt TABLE TASK 76 • On the right hand side of the line, list some of the things you would do differently given what you have learnt today • Discuss