TUMOR
Dr Mohammad.ali
Department of Orthopedics
PATHOLOGY of NEOPLASM
Abnormal mass of tissue
Growth is autonomous, exceeds normal, &
persist after cessation of stimuli
Benign vs. Malignant
– Differentiation & Anaplasia
– Growth rate
– Local invasion
– Ability to metastasize
HISTOPATHOLOGY
Anaplasia
– Hallmark of
malignancy
– Pleomorphism
– Hyperchromatism
– Nuclear cytoplasmic
ratio of 1:1
– Abundant mitoses
– Tumor giant cells
BENIGN more common
MALIGNANT (SARCOMAS) are rare
Differentiation of the lesion
–
–
–
–
–
–
–
–
–
–
–
Fibrous tissue
Fibrohistiocytic
Adipose tissue
Muscle tissue
Lymph vessels
Synovial tissue
Peripheral nerves
Cartilage and Bone Forming tissue
Pluripotential Mesenchyme
Blood Vessels
Uncertain Histogenesis
DIAGNOSTIC CLUES
Size
A mass that is small (< 5 cm in its greatest
dimension) is unlikely to be malignant, while a
mass that is > 5 cm has at least a 20% chance of
being a soft tissue sarcoma
Determined by physical examination if the lesion
is subcutaneous and easily palpable, or by
ultrasound, CT or MRI
DIAGNOSTIC CLUES
Superficial or deep?
Superficial lesions are more likely to be benign
and, when malignant, may have a better
prognosis than deep lesions
The depth is best determined by physical exam,
ultrasound or MRI
The thigh and buttocks are the 2 most common
sites of sarcomas. Any large deep mass in the
thigh or buttocks should be considered at high
risk for being a malignant lesion
DIAGNOSTIC CLUES
Cystic or solid
Most cystic lesions are inflammatory or benign
lesions, such as ganglion cysts or soft tissue
abscesses
If the lesion is solid, it could represent either a
benign or malignant neoplasm
Attempt Transillumination
If deep, ultrasound or MR scan will determine this
DIAGNOSTIC CLUES
Length of symptoms
Rapidly increased in size over 2 months is more
likely to be a sarcoma than the lesion that has
slowly enlarged over a 20-year period
A mass that increases and decreases in size is
usually a cystic lesion
Caution should be taken with masses that have
been present for a long time. Soft tissue sarcomas
occasionally present with a history of many years
duration up to 30 years
TUMOUR WORKUP
History (age, sex, site and past history)
Clinical examination
– Thyroid
– Breasts
– Chest
– Liver
– Kidney
– Rectal (prostate & rectal tumors)
Bloods
– FBC (leukaemic cells etc) & ESR (often elevated)
– Biochemistry (Ca++, PO4, liver enzymes and Alkaline
Phosphatase) -> mets
– Acid Phosphatase (prostate and increased with metastatic
deposits)
– Thyroid function tests
– PSA
– Serum Protein Electrophoresis (Myeloma)
TUMOUR WORKUP (cont)
Urinalysis
Urine Bence-Jones (myeloma)
CXR
Abdominal ultrasound
Bone scan -> other sites
MRI -> soft tissue extent and association with nerves and
vessels
CT of lesion and chest (-> staging)
Angiography -> tumor blood supply and relationship to
major vessels
Biopsy
IMAGING OF SOFT TISSUE TUMOR
Plain radiograph
– Soft tissue shadow, isodense with muscle
– Specific features
Phlebolith within a hemangioma
Cartilaginous juxta-articular masses in synovial
osteochondromatosis
Mature peripheral calcification in myositis ossificans
Central calcification in extraosseous osteosarcoma
Amorphous calcium deposit in tumoral calcinosis
– Bony involvement
IMAGING OF SOFT TISSUE TUMOR
Ultrasound
–
–
–
–
Rapid inexpensive test
Differentiate solid from cystic
Determine size
Can suggest sarcoma features
As many soft tissue sarcoma present as hypoechoic mass than
the echogenic pattern seen in benign lesion, with exception of
liposarcoma
– Delineate areas of distinctly solid portion of a a mass, a
great help for biopsy
– Aid in percutaneous needle biopsy
– Study of vascular supply by Color Doppler
IMAGING OF SOFT TISSUE TUMOR
CT scan
– Detecting calcification or ossification within the lesion
– Evaluate lung metastases
– CT guided needle biopsy
Arteriography
–
–
–
–
Less frequently used
Mapping of lesions in difficult anatomy location
Identifying normal anatomic variants before surgery
Preoperatively, to embolize hypervascular lesions
IMAGING OF SOFT TISSUE TUMOR
Bone scan
– Technetium Tc 99m bone scan
– Detects area of rapid bone turnover
– Sensitive but not very specific, abnormal scan
should be further studied with plain
radiograph, CT and MRI
– Part of staging
IMAGING OF SOFT TISSUE TUMOR
MRI
– Replace role of CT and arteriography
– Advantages
superior soft tissue contrast
multiplanar imaging
no ionizing radiation & the need for iodinated contrast agent
no artifact problem
– General Roles
Accurate preoperative staging
Restriction of differential diagnosis
Assistance with biopsy placement
Monitoring response to neoadjuvant chemotherapy or radiotherapy
Identification of residual or recurrent tumor during postoperative
period
IMAGING OF SOFT TISSUE TUMOR
MRI (cont)
– Conventional T1 weighted and T2 weighted
– T1 weighted differentiate the hyperintense
fatty tissue with hypointense tumor
– T2 weighted with or without fat suppression is
the most appropriate sequence; tumor will be
hyperintense
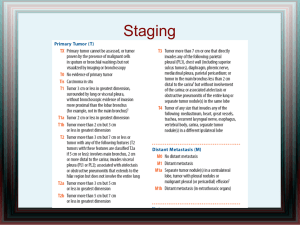
STAGING SYSTEM
Prognostic variables
– Histologic grade
– Tumor size
– Tumor depth
– Compartment status
– Metastases
STAGING SYSTEM
SURGICAL STAGING SYSTEM (SSS)
– Enneking staging system
American Joint Committee on Cancer
(AJCC)
– Cancer Staging Manual 5th Edition
Memorial Sloan Kettering Cancer Center
(MSK)
STAGING SYSTEM
SURGICAL STAGING SYSTEM (Enneking)
Stage
Stage Description
Prognostic Factors
IA Low Grade
Intracompartmental
G1 T1 M0
IB Low Grade
Extracompartmental
G1 T2 M0
IIA High Grade
Intracompartmental
G2 T1 M0
G1
G2
T1
T2
M1
IIB High Grade
Extracompartmental
G2 T2 M0
III Any Metastases
Any G, Any T, M1
Low Grade
High Grade
Intracompartmental
Extracompartmental
Any regional or
systemic metastasis
Prognostic Factors
Histologic Grade (assessment of biological aggressiveness)
– G0
Histological benign
Well differentiated and low cell to matrix ratio
– G1
Low grade malignant
Few mitoses, moderate differentiation and local spread only
Have low risk of metastases
– G2
High grade malignancy
Frequent mitoses, poorly differentiated
High risk of metastases
Features of aggressive tumors:
–
–
–
–
–
Cellular atypia
Frequent mitoses
Extensive necrosis
Significant vascularity
Small amounts of immature matrix
Prognostic Factors
Low Grade
High Grade
Myxoid Liposarcoma
Lipoma-like Liposarcoma
Angiomatoid Malignant
Fibrous Histiocytoma
Malignant Fibrous
Histiocytoma
Pleomorphic Liposarcoma
Synovial Sarcoma
Rhabdomyosarcoma
Prognostic Factors
Site (anatomic setting of the lesion)
– T0
Intracapsular
– T1
Intracompartmental
(e.g. cortical bone, joint capsule or
fascia)
– T2
Extracompartmental
(spreads beyond 'fascial' plane without
longitudinal containment)
Prognostic Factors
Intracompartment
Intraosseous
Intraarticular
Intrafascial compartments
Ray of Hand or Foot
Posterior or Anterior Leg
Ant, Med, Post Thigh
Buttocks
Volar or Dorsal Forearm
Ant or Post Arm
Pericapsular
Extracompartment
Soft Tissue Extension
Deep Fascial Extension
Extrafascial Planes/Spaces
(Neurovascular containing spaces)
Mid & Hind Foot
Mid Hand
Popliteal Fossa
Groin-Femoral Triangle
Intra Pelvic
Antecubital Fossa
Axilla
Paraspinal
BIOPSY OF TUMORS
Simple ? Low Risk Procedure ?
The planning of the biopsy is technically
demanding
All Biopsy carry extreme risk to patient’s limb and
potentially to the patient’s life
Poorly planned biopsy can affect diagnostic
accuracy and result in delay in diagnosis and
treatment
BIOPSY OF TUMORS
Planning the biopsy
– Basic understanding of diseases/tumors and an
ability to generate differential diagnosis
The differential diagnosis determines the indications
for biopsy
– Knowledge of appropriate placement of limb
salvage incisions for resection and
reconstruction
– Access to experienced musculoskeletal
pathologist
BIOPSY OF TUMORS
Type of Biopsy
– Closed Biopsy (Core Needle)
– Open Biopsy
Incisional Biopsy
Excisional Biopsy
Primary Wide Excision
BIOPSY OF TUMORS
Closed
Open
Accuracy of 85%
Accuracy of 96%
Attributed to small size of biopsy
leading to sampling error
Further minimizes risk of
misdirected treatment and its
associated morbidity
Insufficient for electron
microscopic, immunohistochemical,
and molecular genetic testing
Non diagnostic needle biopsy
results in delay in diagnosis and the
need for subsequent formal open
biopsy
BIOPSY OF TUMORS
Closed
Open
Less invasive
Invasive
Requires only LA outside formal OT
Requires Formal Anesthetics Support
and OT
Less soft tissue contamination
Needle tract contamination
Inappropriate incision placement &
soft tissue contamination that
cannot be incorporated into a limb
salvage or amputation plan
Leading to increase likelihood of the
need for soft tissue coverage and a
higher risk for amputation
Lower risk of complication
Higher risk of perioperative
complication; infection, haematoma
and pathological #
Useful in areas of difficult access, like
spine and pelvis without risking
significant contamination
Biopsy Technique
Incisional Biopsy
– Directly cutting into tumor to remove a sample without excising
lesion
– The entire field is excised en bloc with the major tumor mass at
the time of definitive resection
Excisional Biopsy
– Removing the entire lesion at the time of biopsy
– Marginal excision
Primary Wide Excision
– Entire lesion is excised while cutting through normal healthy tissue
and leaving a margin of surrounding healthy tissue against the
lesion
Biopsy Technique
Excisional Biopsy
Indication
– To obtain a large sample size
– For benign non aggressive diagnosis, is the
treatment of the lesion in single stage
Carry higher risk of extensive soft tissue &
important structures contamination
Not for lesion which is suspiciously
malignant or at high risk anatomical
region
Biopsy Technique
Primary Wide Excision Biopsy
Indication
– High suspicious of malignancy
– When the risk of contaminating major
important structures with another form
of biopsy outweighs the risks and
functional and cosmetic deficits of
excising the lesions primarily
Biopsy Procedure
Longitudinal Incision
Limb Salvage or Amputation incision
Surgical Instrument handling
Anybody fingers should not be placed directly
into the wound
Soiled sponges
The surgical field should not be in continuity
with other surgical field
Tourniquet, no exsanguinations
Biopsy Procedure (cont)
Direct approach, contaminating only one compartment,
not through planes
Hemostasis
Vessels, nerves and tendons should not be exposed
Blunt retractors draping
Biopsies the peripheral portion with ellipse shaped cut
Cultures
Volume of 1 to 2 cm3
Post biopsy hemostasis
Closure in layers
Small bite suturing
Light pressure bandaging
Immobilization and protection of weight bearing
OPTION OF DEFINITIVE
MANAGEMENT
CLINICAL AND RADIOLOGICAL DIAGNOSIS
BIOPSY
OBSERVE
STAGING STUDIES
ELIMINATION OF PRIMARY TUMOR
NON SURGERY
SURGERY
RADIOTHERAPY
CHEMOTHERAPY
GENETIC
COMBINATION OF SURGERY
AND NON SURGERY
IMMUNOLOGIC
PROTEIN BASED
PRINCIPLES OF TUMOR SURGERY
INTRALESIONAL
– Incomplete excisions, either gross or microscopic tumor remains
( MARGIN? )
MARGINAL EXCISION
– Resection at border between the tumor & the immediate adjacent tissues,
leaving no tumor, as verified by both gross and microscopic inspection
( SATELLITE LESION? )
WIDE EXCISION
– Excision through normal tissue that is not reactive or edematous, as
judged by preoperative MRI, intraoperative gross inspection and
microscopic sections ( SKIP LESION? )
RADICAL EXCISION
– Wide excision based on anatomic barriers to tumor infiltration
( METASTATIC LESION?)
? COMPLETE REMOVAL AND RECURRANCE RATE
PRINCIPLES OF TUMOR SURGERY
TUMOR RESECTION STRATEGIES
– COMPLETE RESECTION for CURE
– INCOMPLETE RESECTION with CURE obtained from LOCAL
ADJUVANT THERAPIES
– PARTIAL RESECTION without the expectation of achieving cure
(DEBULKING)
CURE means when no local or distant viable tumor cells
remain after surgical resection
Tumor debulking is to eliminate a majority of the tumor
with minimum of morbidity to prolong quality of life and
to reduce or eliminate pain
PRINCIPLES OF TUMOR SURGERY
Meticulous attention to the isolation of
clean and contaminated fields, instruments,
and personnel
Minimize perioperative exposure to
pathogens
– IV antibiotic, antibiotic cement, antibiotic in
irrigation medium
– Allograft and Prosthetic components
PRINCIPLES OF TUMOR SURGERY
HIGH GRADE SARCOMA
– The goal is to remove as much tumor to achieve cure
while removing the least amount of healthy tissue as
possible to preserve function
– AMPUTATION versus Limb Salvage Surgery
– No Significant Statistical Advantage in term of Local
Recurrence
Following amputation
Following limb salvage surgery
1 to 3%
<8%
– Functional loss can be extreme in amputation group
– Revision surgery rates for complications and revisions
are considerably lower for amputation group
PRINCIPLES OF TUMOR SURGERY
HIGH GRADE SARCOMA
– Superficial sarcoma of the trunk have better
prognosis than deep axially located tumor
– Deep axially located tumor like around the
spine and pelvis
Usually present late and often large by the time the
diagnosis is made
Do not routinely permit large volumes of normal
surrounding tissue to be removed with the tumor
PRINCIPLES OF TUMOR SURGERY
HIGH GRADE SARCOMA
– The more inflammatory, fast growing, &
infiltrative the tumor, the wider the margin
should be, & the more strongly preoperative
radiation or chemotherapy is indicated
– Final consideration is the patient’s personal
wishes.
PRINCIPLES OF TUMOR SURGERY
LOW GRADE SARCOMA
– Generally treated similar to the high grade
– Margins are typically smaller as they show;
Smaller or absent reactive zone of inflammation
Limited infiltration
– However a wider margin of excision might be
preferable it if would eliminate the need for
radiation therapy
– Cure is achieved through a carefully planned
surgical excision without adjuvant therapy
PRINCIPLES OF TUMOR SURGERY
DEFECT RECONSTRUCTION
– The second part of surgical resection
– Planned preoperatively
– Liaison with plastic surgeon
– Principles for Pure Soft Tissue Defect
Recon
Preserve Limb Viability
Restore Function
Achieve Skin Closure
PRINCIPLES OF TUMOR SURGERY
DEFECT RECONSTRUCTION
– Principles of Wound Closure
To have the most rapid biologic reconstitution of a
viable skin barrier, between the deep tissue and
outside world
Minimize ‘dead’ space in the deep tissue layer
which can harbor bacterial inoculum
– Radiation and Chemotherapy impair wound
healing
PRINCIPLES OF TUMOR SURGERY
DEFECT RECONSTRUCTION
– Dynamic Reconstruction
– Space Filling Reconstruction
– Skin Barrier Reconstruction
PRINCIPLES OF TUMOR SURGERY
DEFECT RECONSTRUCTION
– Dynamic Reconstruction
Dynamic function include stability, power, blood
transport or nerve conduction
Refers to the implant or transfer of tissues
– Ligaments deficit in knee replaced with autograft,
allograft or artificial replacement
– Vessels Reconstruction to restore blood flow
– Nerve Grafting for protective sensation and motor
function
– Tendon or Muscle Transfer restore lost motor power
PRINCIPLES OF TUMOR SURGERY
DEFECT RECONSTRUCTION
– Space Filling Reconstruction
To fills defects created by surgery
Not to restore function but to relieve tension on the
wound, obliterate dead space and place healthy
tissue in areas that will promote rapid healing and
reduce infection risk
Muscle or Myocutaneous Local, Free and
Vascularized Flap
PRINCIPLES OF TUMOR SURGERY
DEFECT RECONSTRUCTION
– Skin Barrier Reconstruction
Precise wound closure is critical
Wound breakdown can result in deep infection & subsequent
limb loss, might prevent or delay the use of chemotherapy or
local radiation therapy
Skin and subcutaneous fascial layer should be closed in layers,
with precise matching of the anatomic layers
Non braided suture & short tail to minimize foreign body
Small skin staplers with Antibiotic Ointment applied
Early & often changing of dressing
If skin closure with minimal tension cannot be achieved
– SSG of flap
PRINCIPLES OF TUMOR SURGERY
DEFECT RECONSTRUCTION
– Surgical drains
Eliminate dead space-preventing accumulating of fluid
pockets
Divert drainage from the skin incision
Prevent formation and spread of haematoma along fascial
planes-might carry tumor cells
– Drain tracks
Should not traversed uninvolved anatomic areas
Should exit the skin in line with the incision
– Critical drains can be sutured to skin but keep the
suture sites close by for easy excision with drain track
if needed
PRINCIPLES OF TUMOR SURGERY
INTRAOPERATIVE ADJUVANT THERAPIES
– Tumor killing potential
H2O2 - tumoricidal ability
Thermal kill
– Tissue Heating with diathermy, heat gun, cryosurgery using
liquid nitrogen
Produce necrosis of 1 to 10mm
– Lasers
Intraoperative Radiation
– Advantage; Precise & Direct to tumor bed, & not associated
with wound healing difficulty seen with preop, high dose
radiation therapy
Brachytherapy
– Deliver local radiation through catheters implanted surgically
after tumor excision
PRINCIPLES OF TUMOR SURGERY
THE YOUNG CHILD
– Remarkable adaptive capabilities to anatomic loss
either by tumor itself or amputation
– Preserving epiphyses through very closed resection
margins a few mm away from metaphyseal tumor
– If the child survive from the sarcoma, the extremely
long life span ahead raises the lifetime risk of
developing
Secondary radiation induced sarcomas and other radiation
associated morbidities
Secondary chemotherapy induced cancers
PRINCIPLES OF TUMOR SURGERY
THE VERY OLD
– Most common; malignant fibrous histiocytoma
– Problem; less cardiac reserve and overall
poorer physiologic function
Adjuvant chemotherapy and high dose radiation
therapy will cause more risk than benefit
More radical resection with much wider margin
– Senile and Demented Patients, Medical disease
which complicate wound healing
Aim for NO TREATMENT or PALLIATIVE
PRINCIPLES OF TUMOR SURGERY
METASTATIC SARCOMA AT PRESENTATION
– Poor prognosis
– Survival depends on removal of primary tumor &
eradication of metastatic disease through either
surgical or chemotherapeutic modalities or
combination of both
– CHEMOTHERAPY IS ESSENTIAL to eliminate the
micrometastases
– Any surgical complication that can delay or prevent
perioperative chemotherapy must be avoided
– Limb salvage has NO ROLE
PRINCIPLES OF TUMOR SURGERY
‘UNRESECTABLE’ TUMOR
– Tumor involves major vessels, nerves or other critical
structures
– Means unacceptable morbidity
– Truly unresectable situation is death as result.
– In cases with unacceptable morbidity like resection of
tumor including the sciatic nerve, producing insensate
lower limb
Amputation is better choice OR
Limb Salvage surgery with the idea of tiring and skill
demanding nerve grafting or reconstruction, in mind OR if
complication arises, amputation at a very high level is
unavoidable
– Excellent candidate for preoperative chemotherapy,
radiation therapy or more aggressive techniques like
isolated limb perfusion to gain tumor size regression.
PRINCIPLES OF CHEMOTHERAPY
Action of Chemo Agents
– Damage DNA
Alkylating agents, platinum compounds,
anthracyclines, epipodophyllotoxins
– Deplete the cellular building blocks required
for replication
Antifolates, 5-fluoropyrimidines, cytidine analogs
– Interfere with microtubule function required
for mitosis
Vinca alkaloids, taxanes
PRINCIPLES OF CHEMOTHERAPY
Chemo Agents are cytotoxic to tumor cells
through induction of apoptosis
Selectivity is due to the fact that rapidly dividing
tumor did not have sufficient time to repair the
chemotherapy induced damage
Combination chemotherapy
– Antitumor effect will be cumulative whereas the
toxicity will not
– Avoid resistant
– Effective for different phases of cell cycle
PRINCIPLES OF CHEMOTHERAPY
Indication
– Induction chemotherapy (Neoadjuvant or Preoperative)
Decrease tumor size
In tumor that are capable of metastases
(Standard of care for osteosarcoma and Ewing’s sarcoma)
– Malignant musculoskeletal tumor with systemic metastases
– Chemosensitive neoplasm
Osteosarcoma
Ewing’s sarcoma
Rhabdomyosarcoma
Synovial sarcoma
Malignant Fibrous Histiocytoma
– For chemosensitive benign tumors which is multiply recurrent or impinge
on vital structures
PRINCIPLES OF CHEMOTHERAPY
Chemoresistant tumors
– Gastrointestinal stromal tumors
– Chondrosarcoma
– Alveolar soft part sarcoma
PRINCIPLES OF CHEMOTHERAPY
Side Effects
–
–
–
–
–
–
–
Stunting of growth
Osteoporosis
AVN
Cisplatinum -> Nephrotoxicity and hearing loss
Adriamycin -> Cardiotoxicity
Vincristine
-> Neurotoxicity
Chemotherapeutic induced malignancy usually
blood forming eg leukaemias but also may -> Ca
bladder or skin (particularly associated with
cyclophosphamide)
PRINCIPLES OF RADIOTHERAPY
Radioactive focused local treatment
Using high energy photon beam produced by a
linear accelerator
Others; gamma rays, electron beams, radiation
from brachytherapy, beams from heavy particle
like protons and neutrons
Mechanism of action
– Oxygenation of water molecules within the cells,
producing free radicals that interact with DNA to
cause strand break, eventually results in cell death
PRINCIPLES OF RADIOTHERAPY
Radiation units
– Grays (Gy), a unit of absorbed dose (1Gy=1J/kg)
– In the past;
rads
1 rad = 1 centigray (cGy) or 1/100 of a Gy
Radiotherapy is delivered in small doses or
fractions over many days
– Allows a large total dose of radiation to be delivered
without exceeding the tolerance levels of surrounding
normal tissue
– Standard fractionation; 180 to 200 cGy daily, 5 days
per week
PRINCIPLES OF RADIOTHERAPY
Indication in soft tissue sarcoma
– Radiosensitive sarcoma, theoretically, well oxygenated
tumors
Rhabdomyosarcoma
PNET (extraosseous Ewing’s sarcoma)
(definitive primary radiotherapy local control rate for the above
type of tumor is 80%)
(mandatory treatment for all patient)
Other unresectable soft tissue tumor local control rate is in the
range of 25 to 30%
Current standard for high grade resectable extremity soft
tissue sarcomas is limb salvage surgery, when possible, in
conjunction with radiotherapy
PRINCIPLES OF RADIOTHERAPY
Indication in soft tissue sarcoma
– Postoperative radiotherapy
Decrease risk of local relapse for both high grade and certain high
risk low grade sarcoma.
For low grade sarcoma, consider if having microscopic positive
margin or of large tumor size (>5cm)
– Preoperative radiotherapy
Shrink tumor size
Decrease risk of tumor contamination
Intact well oxygenated tumor respond better than hypoxic tumor
bed
Disadvantages
– Delay in surgery
– Possible wound healing complication
– Less information on tumor extent and pathology
PRINCIPLES OF RADIOTHERAPY
Indication in soft tissue sarcoma
– Brachytherapy
Insertion of radiation sources into tissues after tumor resection
before closure
Radioactive source (usually cesium or iodine) placed inside the
catheters on post op D5
Excellent postoperative treatment for extremity soft tissue
sarcoma (adjuvant brachytherapy local control rate for high
grade lesion is 89%)
– Intraoperative Radiotherapy
Electron or orthovoltage beam
74% local control rate for primary retroperitoneal sarcomas
when combined with external beam radiotherapy
PRINCIPLES OF RADIOTHERAPY
Timing of radiotherapy
– Definitive radiotherapy for
rhabdomyosarcoma and Ewing’s sarcoma is
generally integrated into the middle of a
chemotherapy program
– Postoperatively, as soon as adequate wound
healing is achieved, usually 3 to 6 weeks
PRINCIPLES OF RADIOTHERAPY
Side Effects
– Acute side effects depend on the total dose of
radiation and overall treatment time
– Late side effects depend on fraction size
PRINCIPLES OF RADIOTHERAPY
Acute Side Effects
– begins after first 2 weeks and increase as the
treatment continues
– Most common is fatigue
– Majority develop erythema, and temporary
desquamation
– Uncommon; wound dehiscence, suppresses blood
counts and other complications pertaining to anatomic
site involved
– At least one clinic visit per week to see radiation
oncologist to assess and manage potential side effects
PRINCIPLES OF RADIOTHERAPY
Late Side Effects
– Months to years after receiving radiotherapy
Muscle fibrosis; stretching exercise
Weaken Bones and cause Joint Dysfunction
Edema distal to irradiated site; full circumference of limb
should never be treated to a high dose
– More then 20 years after radiation
Secondary malignancy esp. in children
Rate of secondary bone cancer after radiation treatment for
all childhood cancers was less than 1%
For those treated for Ewing’s sarcoma, the risk was 5.4%
Others; bone growth arrest and iatrogenic scoliosis in children
THANK YOU