Non-Invasive Safety and Wellness Technologies
advertisement

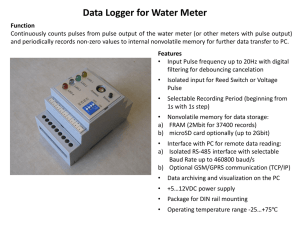
Non-Invasive Safety and Wellness Technologies Mike McEvoy, PhD, NRP, RN, CCRN Sr. Staff RN – Cardiothoracic Surgery Chair – Resuscitation Committee – Albany Med Ctr EMS Coordinator – Saratoga County, New York EMS Editor – Fire Engineering magazine Mike McEvoy - Books: Disclosures • I am on the speakers bureau for Masimo Corporation. • I am the EMS editor for Fire Engineering magazine. • I do not intend to discuss any unlabeled or unapproved uses of drugs or products. • Slides at: www.mikemcevoy.com Nurses Week 2012 – Albany Medical Center (NY) How Good Are You? • HR • LOC • BP • Resps Not As Good As You Might Think: • 50% of physical assessments wrong • Therapeutic interventions altered with invasive assessment 34 - 56% of the time: • • • • • • • 1980 Del Guercio 1984 Eisenberg 1990 Bailey 1991 Steinberg 1994 Minoz 1998 Staudinger 2002 Jacka, etc, etc… How Good Are Your Monitors? Pulse Oximetry Problems: • Accuracy • Motion & artifact • Dyshemoglobins • Perfusion Oxygenation • Pulse Oximetry Oxygenation • Pulse Oximetry Model of Light Absorption At Measurement Site Without Motion Absorption AC Variable light absorption due pulsatile volume of arterial blood DC Constant light absorption due to non-pulsatile arterial blood. DC Constant light absorption due to venous blood. Time DC Constant light absorption due to tissue, bone, ... Model of Light Absorption At Measurement Site With Motion Absorption AC Variable light absorption due pulsatile volume of arterial blood DC Constant light absorption due to non-pulsatile arterial blood. AC Variable light absorption due to moving venous blood Time DC Constant light absorption due to venous blood. DC Constant light absorption due to tissue, bone ... Influence of Perfusion on Accuracy of Conventional Pulse Oximetry During Motion Good Perfusion (Conventional PO) SpaO2=98 SpvO2=88 SpO2=93 Poor Perfusion (Conventional PO) SpaO2=98 SpvO2=50 SpO2=74 Conventional Pulse Oximetry Algorithm R & IR Digitized, Filtered & Normalized MEASUREMENT R/IR CONFIDENCE Post Processor % Saturation 3 options during motion or low perfusion: 1. Freeze last good value 2. Lengthen averaging cycle 3. Zero out Next Generation Pulse Oximetry Next Generation Pulse Oximetry Masimo SET: Signal Extraction Technology R/IR (Conventional Pulse Oximetry) MEASUREMENT CONFIDENCE MEASUREMENT DSTTM R & IR Digitized, Filtered & Normalized CONFIDENCE MEASUREMENT FSTTM CONFIDENCE Confidence Based Arbitrator Post Processor % Saturation DST SET – 97% MEASUREMENT SSTTM CONFIDENCE 0 MEASUREMENT Proprietary Algorithm 4 CONFIDENCE Masimo SET “Parallel Engines” SET “Parallel Engines” 50% 66% 97% 100% SpO2% A Solution for Patient Motion Discrete Saturation Transform (DST) In the presence of motion, SET separates the venous and arterial saturation values resulting in accurate saturation readings (compared to conventional oximetry that averages the values to produce a reading) Variable Constant Variable Averaging inaccurate SpO2 0 50% 66% 86% Constant 97% 100% SpO2% Conventional Pulse Oximetry 0 50% Separating accurate SpO2 66% 86% 97% 100% SpO2% Measure Through Motion Pulse Oximetry Certainty… Pulse Oximetry Problems: Accuracy Motion & artifact • Dyshemoglobins • Perfusion Carbon Monoxide (CO) • Gas: • Colorless • Odorless • Tasteless • Nonirritating • Leading cause of poisoning deaths worldwide! CO: The Leading Cause of Poisoning Deaths 30-50 % of CO-exposed patients presenting to Emergency Departments are misdiagnosed Barker MD, et al. J Pediatr. 1988;1:233-43 Barret L, et al. Clin Toxicol. 1985;23:309-13 Grace TW, et al. JAMA. 1981;246:1698-700 Show me the money…Is this real? 104 CCU admissions UAP: 3 CO toxic, 5 others minor exposure (> smoker). Balzan et al, Postgrad Med J, 1994;70:699-702 Up to 10% of UAP, ACS, seizure, and h/a admits 168 acute neuro admits: 5 CO toxic (2 from group w/ seizures) CO poisoning Heckerling et al,have Clin Toxicol, 1990;28:29-44. 307 acute neuro admits: 3 CO toxic (all from group of 29 w/ decr. LOC absent focal s/s). Balzan et al, Postgrad Med J, 1996;72:470-3. 48 h/a pts: 7 COHb > 10% (14.6%, all unrelated to smoking) Heckerling et al, Am J Emer Med, 1987;5:201-4. 146 h/a pts: 4 COHb > 10% (3%, all unrelated to smoking) Heckerling et al, Ann Intern Med, 1987;107:174-6. Limitations of Pulse Oximetry Conventional pulse oximetry can not distinguish between COHb, and O2Hb From Conventional Pulse Oximeter SpCO-SpO2 Gap: The fractional difference between actual SaO2 and display of SpO2 (2 wavelength oximetry) in presence of carboxyhemoglobin From invasive COOximeter Blood Sample [Blood] Barker SJ, Tremper KK. The Effect of Carbon Monoxide Inhalation on Pulse Oximetry and Transcutaneous PO 2. Anesthesiology 1987; 66:677-679 Signs and Symptoms SpCO% <5% Clinical Manifestations None 5-10% Mild headache, tire easily 11-20% Moderate headache, exertional SOB 21-30% 41-50% Throbbing headache, mild nausea, dizziness, fatigue, slightly impaired judgment Severe headache, vomiting, vertigo, altered judgment Confusion, syncope, tachycardia 51-60% Seizures, unconsciousness 31-40% Carbon Monoxide Poisoning Presents Like the Flu! Laboratory CO-oximetry Pulse CO-oximetry Hgb Signatures: Physics of O2 Pathways FDA Validation Rainbow SET Compared to Reference Methodology Noninvasive measurement provides clinically equivalent results for HbCORed without invasive blood draw (+ 3% from 0 – 40%) 14,438 Patient Brown University Study • Partridge and Jay (Rhode Island Hospital, Brown University Medical School), assessed carbon monoxide (CO) levels of 10,856 ED patients • 11 unsuspected cases of CO Toxicity (COT) were discovered. Overall mean SpCO was 3.60% • Occult COT was 4 in 10,000 during cold, 1 in 10,000 during warm months • They concluded “unsuspected COT may be identified using noninvasive COHb screening and the prevalence of COT may be higher than previously recognized” Non-Invasive Pulse CO-Oximetry Screening in the Emergency Department Identifies Occult Carbon Monoxide Toxicity. Suner S, Partridge R, Sucov A, Valente J, Chee K, Hughes A, Jay G. J Emerg Med 2008 Department of Emergency Medicine, Rhode Island Hospital, Brown Medical School, Providence, RI. Methemoglobinemia • Cyanotic Chemical Guardian Protocol – Health surveillance for cyanosis causing chemical handlers (pre-placement, routine, high risk assignment clearance and symptomatic workers). Causes of Acquired Methemoglobinemia Iatrogenic Causes: • • • • • • • • • • Benzocaine & Cetacaine sprays Dapsone EMLA Creams Chloroquine Flutamide Lidocaine Nitrates Nitric oxide Nitroglycerin Nitroprusside Ash-Bernal R, et al. Acquired Methemoglobinemia A Retrospective Series of 138 Cases at 2 Teaching Hospitals. Medicine Sept 2004;83(5):265-273. Others (community based): • Soda and other foods with phenol based preservatives • Nitrogen based fertilizers • Nitrate laden preservatives (such as saltpeter used to cure BBQ meats) • Infantile diarrhea (high intestinal pH promotes gram-negative organism growth, converts dietary nitrates to nitrites) Symptoms of Methemoglobinemia SpMet% Clinical Manifestation 0-3% Normal concentration, no symptoms 3-15% Slight skin discoloration (palor, gray, or blue) may be present 15-20% Patient may be relatively asymptomatic, cyanosis likely 25-50% Headache, dyspnea, lightheadedness, weakness, confusion, palpitations, chest pain 50-70% Altered mental status, delirium Methemoglobinemia Can Present Like the Flu! Source: David C Lee, MD, Research Director, Assistant Professor, Department of Emergency Medicine, North Shore University Hospital and New York University Medical School Traditional Diagnosis of MetHb Traditional marker: “chocolate brown” color of arterial blood Laboratory CO-oximeter Limitations of Pulse Oximetry From Pulse Oximeter The 85% SpO2 “Push”: The difference between actual SpO2 (blue) and display SpO2 (red) (2 wavelength oximetry) in presence of methemoglobin From invasive CO-Oximeter Blood Sample [Blood] Barker SJ, Tremper KK, Hyatt J. Effects of Methemoglobinemia on Pulse Oximetry and Mixed Venous Oximetry. Anesthesiology 1989;70:112-117 Noninvasive Pulse CO-Oximetry Oxygenated Hb and reduced Hb absorb different amounts of Red (RD) and Infrared (IR) Light (Two-wavelength oximeters cannot measure dyshemoglobins) FDA Validations Rainbow SET Compared to Reference Methodology 14 12 SpMet (%) 10 8 6 4 2 0 0 2 4 6 8 10 12 14 HbMet (%) Noninvasive measurement clinically equivalent results for MetHb without invasive blood draw Equivalent precision and accuracy (+ 1% from 0-25%) Perfusion Nellcor Capnoprobe™ l US approval Jan 2003. l Research study: Children's Medical Center – Dallas TX. l 11 kids infected Burkholderia cepacia, 2 died. l Traced to saline solution packaging of probes. l 5,600 units @ 30 centers recalled Perfusion Index Saturation Infrared Red Infrared Signal • Perfusion index is the ratio of the variable absorption (AC) to the non-variable (DC) of the infrared signal. 0.254-0.253 = 0.001 0.253- 0 = 0.253 AC DC 0.001/0.253 = 0.4% • PI display ranges from 0.02% (very weak) to 20% (very strong) Perfusion Index • Perfusion Index is an objective method for measuring a patient’s peripheral perfusion • Perfusion Index is an early indicator of deterioration Datex-Ohmeda PIr® Range 0.3%-10% Most Patients >0.7% Increases the validity of the SpO2 by locating the strongest pulse signal Philips Range 0.3%-10% Optimal >1.0% < 0.3% is marginal reposition the site Masimo Range 0.02%- 20.0% Perfusion Index Select site with highest value What is the “Normal” PI value? • 108 healthy adults and 37 critically ill patients (finger sensors) • PI range: 0.3% to 10%, median 1.4% • ROC used to determine the “cutoff” value • 1.4% PI best discriminated normal from abnormal Lima, et al. CCM 2002 R IR Absorption Photoplethysmography Pleth Waveform Photodetector Time Pleth Waveform Definition of PVI • Pleth Variability Index (PVI) is a measure of dynamic changes in PI that occur during the respiratory cycle • PVI is a percentage from 1 to 100%: 1 = no variability 100 = maximum variability • PVI: fluid volume status • High variability (high PVI) = volume depletion Research on PI and PVI Ongoing… Can we get oximetric hemoglobin? • SpHb added in 2008 Jan 2012: Pronto-7 (for adults > 30 kg) • Noninvasive, quick, and accurate spot-check hemoglobin testing • Measures (Under 1 Minute) • • • • Total Hemoglobin (g/dL, g/L, mmol/L) – SpHb (±1 g/dL at 1 SD) Oxygen Saturation - SpO2 Pulse Rate - PR Perfusion Index - PI • Touch Screen Navigation • Multiple Printing Solutions • Blue Tooth • Wireless • Multiple Patient Reports • Stores Patient Test Information Pronto 7 Accuracy Frasca D et al. Crit Care Med. 39(10); 2011; 2277-2282. Ocular Scanner EyeMarker Systems™ Retinal imaging Pattern recognition: • Botulism, neurotoxins • Nerve Agents • Carbon Monoxide • Cyanide Pulse CO-Oximetry Applications • Screening during routine exams • CO, Met, Hb baseline values • Early detection and prevention • Urgent screening • Rapid assessment of exposed/injured workers • Triage and assessment (including PI) • Health and safety tool • Monitoring high risk areas/workers Questions? mikemcevoy.com