Infection Control Issues in the Dialysis Setting
advertisement

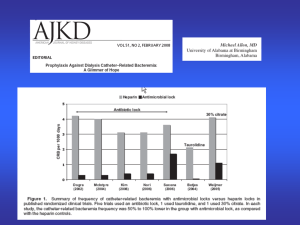
Infection Control Issues in the Dialysis Setting Stuart L. Goldstein, MD Associate Professor of Pediatrics Baylor College of Medicine Medical Director, Renal Dialysis Unit Texas Children’s Hospital Houston, Texas Helen Currier, RN, BSN, CNN Assistant Director Renal Dialysis and Pheresis Texas Children’s Hospital Houston, Texas Infections in the Dialysis Setting Significant cause of hospitalization Significant cause of mortality Data compiled from the United States Renal Data System (USRDS) Change in hospital admissions since 1993 Figure 6.3 Period prevalent dialysis patients. Rates adjusted for age, gender, race, and primary diagnosis. ESRD patients 2005 used as reference cohort. Adjusted admissions for principal diagnoses, by modality Figure 6.5 Period prevalent ESRD patients; adjusted for age, gender, race, & primary diagnosis. ESRD patients, 2005, used as reference cohort. Adjusted cause-specific hospital admissions, by age Figure 6.7 Dialysis patients, 2005, used as reference cohort. Rates adjusted for gender, race, & primary diagnosis. Period prevalent dialysis patients age 20 & older. At the end of 1998 a new ICD-9-CM code was added for infections due to internal devices in peritoneal dialysis patients; data prior to this date are omitted. Infections in this category include those related to vascular access devices or peritoneal dialysis catheters. Percent change in hospitalization rates for prevalent dialysis patients, 1995–2005, by demographic characteristics & primary diagnosis Figure 6.6 Period prevalent dialysis patients; rates for all patients are adjusted for age, gender, race, & primary diagnosis; rates by one factor are adjusted for the remaining three. Direct comparison of adjusted rates is appropriate only within each graph, not between graphs. Dialysis patients, 2005, used as reference cohort. Vascular access data include hemodialysis patients only. Geographic variations in cause-specific admissions, per 1,000 patient-years, 2005, by state: HD, infection Figure 6.10 (continued) Period prevalent hemodialysis patients, 2005. Excludes patients residing in Puerto Rico & the Territories. Percent change in infectious admission rates, 1995–2005, by state Figure 6.11 (continued) Period prevalent hemodialysis patients, 1995–2005. Excludes patients residing in Puerto Rico & the Territories. All-cause mortality: patients with major diseases, 2005 Figure 6.15 ESRD & general Medicare patients with diagnosis in 2005; adjusted for gender & race. Medicare patients, 2005, used as reference cohort. Survival rates after major disease diagnosis in the ESRD & general populations Figure 6.17 Prevalent general Medicare & ESRD patients with diagnosis between 1992 & 2004. Medicare patients, 2005, used as reference cohort. Adjusted cause-specific mortality: infection Figure 6.21 Incident dialysis patients. Rates by age adjusted for gender, race, & primary diagnosis; rates by race adjusted for age, gender, & primary diagnosis. Incident ESRD patients, 1996, used as reference cohort. Outline Review dialysis treatment procedure/logistics Challenges for infection control Blood borne pathogens Respiratory Contact contamination Regulatory requirements Center DSHS CDC QA/QI for Medicare & Medicaid Services (CMS) Dialysis Procedures Hemodialysis Blood cleaned directly through a closed extracorporeal circuit Blood accessed via Arterio-venous fistula (AVF) Arterio-venous graft (AVG) Percutaneous central venous catheter Can be performed in-center or at home Peritoneal Dialysis Catheter placed percutaneously into peritoneal cavity Patient exchanges fluid via that catheter at various intervals during the day or night Performed at home Hemodialysis Logistics Patients dialyze for 3-4 hours thrice weekly Open ward setting Unit schedules can run up to 4 shifts per day depending on census Patients follow each other in same chair Same machines Different disposables Dialyzers re-used for same patient up to 10 treatments Nurse/Technician to patient ratio 1:1 to 1:4 depending on acuity Disinfection Procedures Patient station surfaces Any soap Between each patient shift Medical Equipment Hospital disinfectant (low level) Between patient use Blood spills Tuberculocidal/1:100 Immediate bleach (intermediate level) Disinfection Procedures Bloodborne Pathogen Challenges Hepatitis B virus Hepatitis C virus HIV Hepatitis B Desired Patient Outcomes The patient will not convert to HbsAg+ status Hepatitis B will not be transmitted in the dialysis unit Nephrology Nursing Standards of Practice and Guidelines for Care (2005) Hepatitis Susceptibility Testing Hepatitis B Vaccination Hep B vaccine dose is higher for patients with ESRD 40 mg Hepatitis B Vaccination HepB+ Patient Management Hepatitis B virus is readily transmitted across the dialysis filter membrane Hepatitis B+ patients require isolation in separate room (new units) or a separate area Do not re-use dialyzers Patient education Hepatitis C Desired Patient Outcomes The patient will not convert to a positive antiHCV status The patient with a positive anti-HCV will not transmit the disease Nephrology Nursing Standards of Practice and Guidelines for Care (2005) Hepatitis C Monitor hepatitis C surveillance laboratory test results Antibody to hepatitis C virus (anti-HCV) and alanine aminotransferase (ALT) on admission for all patients ALT monthly for anti-HCV negative patients Anti-HCV semiannually for all negative anti-HCV patients Supplemental or confirmatory testing with more specific assays for patients with an initial positive antiHCV Hepatitis C Surveillance HepC+ Patient Management Hepatitis C is NOT readily transmitted across the dialysis filter membrane Patient isolation is not required Machine isolation is not recommended May re-use dialyzers HIV Routine surveillance not required Isolation not required May re-use dialyzers Respiratory Infection Control Challenges Host Transmission Tuberculosis Varicella Immunocompromised Host Susceptibility ESRD complicates other systemic illness Stem cell transplantation Solid organ transplantation Respiratory Infection Control Measures Isolation rooms required for all new dialysis units Negative pressure is usual Only one room required per unit Mask isolation All patients with suspected TB or VZV should be isolated or wear masks during evaluation Negative pressure rooms should have at least 6 air exchanges per hour Tuberculosis Desired patient outcomes The patient will not convert from a negative to a positive tuberculosis (TB) skin test The patient will not progress to active TB disease The patient with active TB will not transmit the disease Nephrology Nursing Standards of Practice and Guidelines for Care (2005) Tuberculosis Monitor laboratory test results related to TB screening, diagnosis, and treatment Mantoux skin test CXR Sputum smear and culture Assess for S/S of TB Productive or persistent cough Cloudy or blood-tinged sputum Unexplained weight loss Night sweats Elicit hx of exposure to TB Tuberculosis Assess for risk factors that increase the risk of development of active TB disease after exposure Immunosuppression HIV Hx of TB or + skin test without treatment or completion of prescribed medication Monitor adherence to home medication regimen for patients receiving therapy Tuberculosis Intervention Provide TB screening per current CDC recommendations IC policies and procedures that are consistent with current CDC guidelines Coordinate care with other health care providers and agencies, e.g. local health department, as indicated Tuberculosis Patient Education Rationale for TB surveillance Teach respiratory IC practices Reinforce importance of adherence to prescribed medication regimen Teach S/S of disease progression to report to nurse Hand Hygiene Educational Design Objectives 1. Identify risk for infection in the hospital or home 2. List one hand hygiene myth and one hand hygiene fact. 3. Identify key steps for hand washing: * Soap and water *Alcohol-based hand sanitizer 4. Demonstrate correct hand washing techniques: *Soap and water *Alcohol-based hand sanitizer 5. Name four instances when hands should be washed to limit the transfer of bacteria, viruses and other microbes. 6. Identify hand washing issues unique to children. Related Content I. Germs: What are they? II. Reducing the risk of infection III. Myths and Facts IV. Lesson on hand washing techniques A. Steps for soap and water B. Steps for alcohol- based hand sanitizers V. When to wash hands VI. Issues unique to children Contact Contamination Nurse/technical staff care for >1 patient at a time Caregivers must wear appropriate personal protective equipment Gloves, gowns and masks with face shields when accessing AVF, AVG, catheter Gloves must be used for All All patient contact machine contact All medication preparation Gloves must be changed Between patients Between machines When moving from one area to another Bacterial Infection Desired Patient Outcomes The patient will be free of signs and symptoms associated with localized infection or sepsis The patient’s risk for bacterial colonization or infection due to a drug-resistant organism will be reduced Nephrology Nursing Standards of Practice and Guidelines for Care (2005) Bacterial Infection Assessment Intervention Laboratory analyses/cultures Avoid culturing vascular catheter tips surrounding skin or catheter hub Catheter exit site or wound cultures Collaborate with MD/APN to avoid over use of vancomycin Monitor patient response, e.g. resolution of infection, development of sepsis Bacterial Infection Intervention Unit infection control policies and procedures consistent with the CDC guidelines (2001) Patient education Potential for bacterial colonization and infection of access Importance of permanent vascular access placement rather than long-term use of a hemodialysis catheter Bacterial Infection Patient education Good Care of vascular access; Washing prior to dialysis Glove use when holding vascular access site to stop bleeding Peritoneal catheter exit site care Use hygienic practices of prophylactic antibiotic therapy new PD catheter Topical exit site antibiotics (mupirocin, gentamicin) Importance of immunizations Unit QA/QI Practices Ongoing assessment of current and trend analyses of relevant infection rates MRSA Catheter related bacteremia Catheter exit site and tunnel infections Peritonitis Surveillance for Hepatitis virus susceptibility status Facility Infection Trends Percent of Facility Census with Infections By Type During Month %100 95 90 85 80 75 70 65 60 55 50 45 40 35 30 25 20 15 10 5 0 Jan Feb Graft/Fistula 45 40 Catheter 23 28 Wound/Limb 5 10 Sepsis/Bacteremia 2 3 HBaAg+ 0 0 MRA-VRE 2 4 Other 23 15 Facility Name Mar Apr May Jun Jul Aug Sep Oct Nov Dec ESRD Network of Texas The Water Treatment System Water Treatment System Testing/Standards (AAMI) Testing performed monthly Maximal level of bacteria in water to prepare dialysis fluid/reprocess dialyzers must NOT EXCEED 200 CFU AAMI action level is 50 CFU Maximal level of endotoxin must not exceed 2 EU/ml AAMI action level is 1 EU/ml Testing Sites Testing Sites