EBV positive DLBCL of the elderly
advertisement

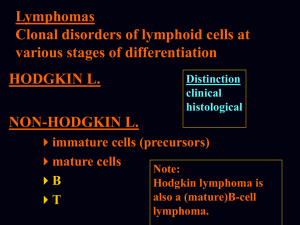
EBV positive DLBCL of the elderly 2013/04/01 住院總醫師 王智慧 報告 感謝 蕭樑材大夫 指導 Am. J. Hematol. 86:663–667, 2011. • diffuse large B-cell lymphoma (DLBCL)~ 31% of all non-Hodgkin lymphoma • Burkitt , plasmablastic, NK/T-cell, angioimmunoblastic, Hodgkin, hydroa-like T-cell lymphoma and lymphomas associated with HIV infection, posttransplant lymphoproliferations, and after exposure to certain cytotoxic or immunomodulator agents. Patients and Methods • January 2002-December 2009, • all newly diagnosed DLBCL from the medical records • CD20,CD10,bcl-6,MUM1/IRF4 (cutoff: 30%) • EBER in ≧20% of malignant cells • EBV-positive DLBCL of the elderly were defined: • (1) age ≧ 50 years, • (2) no clinical and/or laboratory evidence of immunodeficiency, • (3) diffuse large cell morphology with positive expression of CD20, • (4) EBV-encoded RNA positivity in the tumor cells. -exclusion• Transformed and primary cutaneous variants of DLBCL • coinfection by HIV, hepatitis B, hepatitis C, or human T-lymphotrophic virus-1 • clinical suspicion of immunodeficiency such as chronic infections, chronic diarrhea, and chronic eczema • chronic disease associated with leucopenia or lymphopenia, or low immunoglobulin levels Oyama score includes age≧ 70 years and presence of B symptoms as adverse risk factors three risk groups, low (0 factors), intermediate (1 factor), and high risk (2 factors). AWOD: alive without disease, AWD: alive with disease, NR: no response • Multivariate survival analyses were not attempted due to the small number of cases. Results • A total of 199 new cases of DLBCL were identified, 28 patients met the criteria, incidence rate of 14% . • Median age at diagnosis: 75 years (51~95) . • 17 men, 11 women (61% and 39%) 1.5:1. • Hb <10 g/dL, platelets <150 x 10^9/L, lymphocytes <1.0x 10^9/L in 61%, 21%, and 37% of the patients, respectively. • ECOG >1 18 patients (64%), • LDH levels elevated in 11 (41%), • advanced clinical stages (Stage III or IV) in 14 (50%). • N=14 (50%) presented exclusively with nodal disease, • n=11 (39%) had nodal and extranodal involvement, • n=3 (11%) had primary extranodal disease, involving the stomach in all cases. • extranodal sites of involvement were GI tract (n=6), lung (n=3), oropharynx (n=3), bone marrow (n =2), adrenals (n=1), skin (n=1), bone (n=1). • B symptoms in 12 cases (43%) • IPI scores >2 in 16 cases (57%). • Low, intermediate, high Oyama scores in 5 (18%), 12 (43%), and 11 (39%) patients Histology • diffuse pattern, large cells • (68%) Monomorphic with a centroblastic or immunoblastic morphology, frequent mitoses, usually necrosis • (32%) polymorphic large neoplastic cells with immunoblastic morphology admixed with variable amounts of small lymphocytes and histiocytes. • All cases showed scattered RS- like cells. • 19 patients (68%) had a non-germinal center (NGC) and 9 (32%) had a germinal center (GC)-like phenotype. Blood. 2004;103:275-282 Blood. 2004;103:275-282 Therapy N CHOP R-CHOP No chemo 12 8 8 CR 50% (n= 10) PR 5% (n= 1) NR 45% (n= 9) Rapid progress or poor PS CR CR 33% (p= 0.3) CR 63% - Alive 33% (p= 0.17) 75% - 8 mos 20 mos OS 1.5 mos (p=0.002) • median follow up of 32 months, 18 patients (64%) have died; 83% from lymphoma progression. • OS for the entire group was 5 months and 3-year OS was 33% Worse OS • age ≥70 years (n= 14; P= 0.002), advanced clinical stage (n= 9; P= 0.02), ALC <1.0x10^9/L (n= 4; P= 0.004). • ECOG performance status > 1, hemoglobin <10 g/dL , platelets <200x 10^9/L, elevated LDH levels showed a trend 64 mos 5 mos 64 mos 8 mos Discussion • age >70, advanced stage and ALC <1.0 3 109/L ~ a worse OS rate, • R-CHOP may derive better CR and OS rates than CHOP • Asian studies, incidence 5 ~11% • in Western populations, incidence < 5% • Immunosenescence characterized by decreased number and function of T-cells in peripheral blood and lymph nodes, apoptosis dysregulation, and elevation of levels of proinflammatory molecules • Park et al. showed that EBER-positive DLBCL patients showed poorer clinical response and worse OS rates than EBERnegative patients • In a prior study from our group, the presence of EBER in DLBCL patients was also independently associated with a worse prognosis • these studies did not include patients treated with rituximab-containing regimens Clin Cancer Res 2007;13:5124–5132. Materials and Methods • Diagnosis. when more than 50% of the proliferating, often neoplastic appearing cells showed both of the expression of one or more pan–B cell antigens (CD20/CD79a) and/or light-chain restriction and positive signal for in situ hybridization using EBV-encoded small nuclear early region (EBER) oligonucleotides on paraffin section for patients more than 40 y/o without predisposing immunodeficiency • Among 149 cases fulfilling these criteria, 96 cases with available clinical data set were enrolled • For the control group, 107 patients aged over 40 years with EBV-negative DLBCL treated consecutively at Aichi Cancer Center between 1993 and 2000. Sites of extranodal involvement • N= 17 (20%), limited to extranodal sites. • N= 27 (31%) had only lymphadenopathies without extranodal involvement, • N= 43 (49%) had lymphadenopathies with extranodal involvement. polymorphic subtype scattered distribution of Hodgkin and Reed-Sternberg - like giant cells EBNA2 stain CD 20 (+) Histologic features • diffuse and polymorphic proliferation of large lymphoid cells with a varing degree of reactive components such as small lymphocytes, plasma cells, histocytes, and epithelioid cells ,sometimes accompanied by necrosis and an angiocentric pattern. • Often featured by a broad range of B-cell maturation, containing morphologic centroblasts, immunoblasts, and Hodgkin and Reed-Sternberg (HRS)–like giant cells with distinct nucleoli • morphologically divided into two subtypes: • large cell lymphoma (LCL): n=34, having notably dominant areas where large lymphoid cells with relatively monomorphic appearance. • polymorphic LPD subtypes: n=62, scattered distribution of large cells in the polymorphous composition. • The histology was frequently varied from area to area, indicating a continuous spectrum • no significant difference in any clinical characteristics and immunophenotype between these two groups Phenotypic features • LMP1 was positive on the large atypical cells in 67 (94%) out of 71 tested cases. • EBNA2 was detected in the nuclei of 16 (28%) of 57 tested cases • CD30 was stained more common in agerelated EBVpositive B-cell LPDs than in EBV-negative DLBCL (75% vs 13%, P < 0.0001). • CD10 expression (18% vs 38%, P = 0.015) Response to treatment and Kaplan-Meier survival estimates • chemoregimens containing anthracycline for 62 patients (79%) and without anthracycline for 7 patients (9%)~EBV+ • 40 (63%) of 64 evaluable patients with achieved a CR with initial therapy~EBV+ • 95 (91%) of 104 evaluable cases with DLBCL achieved a CR (P < 0.0001). • 57 deaths in 96 cases of age-related EBVpositive B-cell LPDs , 34 deaths in 107 cases of DLBCL. • causes of death available for 47 cases for age-related EBV-positive B-cell LPDs and 29 for DLBCL. • Deaths (PD and complications such as infections) in 38 and 9 cases, in agerelated EBV-positive B-cell LPDs, 23 and 6 cases in EBVDLBCL. • The observed differences between two disease groups were not significant (P = 0.870). – more than 70 y/o- not significant (P = 0.747). A significant difference was still found even when accounting for age 24 mos H-I/High IPI Low/L-I IPI score of 0 (n = 18), no adverse factors 56.3 mos score of 1 (n = 39), one factor25.2 mos Oyama score of 2 (n = 21) , two factors 8.5 mos score 56 mos 25 mos 8.5 mos Switzerland, Austria, Italy 8/258 (3.1%) Median age: 67.5 y/o OS: 5.5 mos (EBNA2+): 103 mos (DLBCL > 50 y/o) EBV-positive DLBCL of the elderly in the Asian population seems to be more frequent at extranodal sites, e.g. up to 80% no correlation between age and prevalence of EBV in any of the studied DLBCL collectives