Wound Care
Reimbursement 101:
Keys to Success
Melissa Johnson PT, DPT, CWS
Southside Regional Director
Wound Care and Hyperbaric Services
Piedmont Healthcare, Atlanta GA
WHO SHOULD KNOW THE
RULES?
Any
provider providing services to
patients
Any
provider documenting and billing
services
All
of YOU should know the basics
Our Challenge in Today's
Healthcare
Using
diagnosis codes to support
medical necessity
Keeping up with constant change
with coding
Meeting documentation requirements
Adapting to changing payment
systems
Surviving an audit
Continuing to maintain or make
revenue
3 Focus Areas for Success
Coverage
– Are the procedures I am performing
covered?
Coding
– Are the ICD 9 codes and CPT codes
medically necessary?
Payment
– Am I getting reimbursed for the
treatment I am performing?
Tools For Success
Every year you should?
– Purchase or have available an updated CPT
book and ICD 9 book
– Know your Practice Act in your state
– Know your MAC (Medicare Administrative
Contractor)
– Read and monitor all local coverage decisions
(LCD) and national coverage decisions (NCD)
for your MAC jurisdiction throughout the year
– Verify insurance and payer to ensure prior
authorizations for procedures are not required
(ie; negative pressure, debridement, etc.)
Definitions
CPT – (Current Procedural Terminology)
Procedure/treatment being performed
ICD – 9 – Diagnosis code for what is being
treated; ex: diabetic foot ulcer – 250.80 and
707.15
MAC – Medicare Administrative Contractors
LCD – Local Coverage Decision
NCD – National Coverage Decision
Definitions continued
Medical Necessity - Per guidelines the
procedure being performed meets medical
necessity for the diagnosis being treated
Modifiers –two digit code that modifies a
service/procedure so they can be billed
together
Revenue Codes – identifies who is doing
the procedure or treatment; i.e. physical
therapist is revenue code GP 420
Physician Fee Schedule – the fees that are
billed to Medicare patients for procedures
provided
What is your MAC?
MAC – Medicare administrative contracts
were formed to replace the contractors for
Medicare that process claims
19 MACS were formed (15 for part A and
B, then 4 others for durable medical)
Jurisdictions were created in 2009 to
replace fiscal intermediaries in each state
MAC MAP
Review All Medical Policies Related
to Your Business
Private Payers, Medicare Managed Care,
Medicaid, Workers Compensation, etc.
– Medical Policies for top 10 private payers
– Obtain prior authorization if required
Ex:
Negative Pressure
Medicare
– Local Coverage Decisions
– National Coverage Decisions
http://www.cms.gov/medicare-coverage-
database/overview-and -quick-search.aspx
Local and National Coverage
Decisions
These are your playbook
Documentation guidelines, CPT and ICD 9 codes
for medical necessity, descriptions, etc
Opportunities to respond and impact LCD in your
MAC regions
Need any LCD or NCD pertaining to all
procedures performed in the clinic
– Examples of NCD
Hyperbaric Oxygen
– Examples of the LCD
Physical Therapy
Debridement
Skin Biologicals
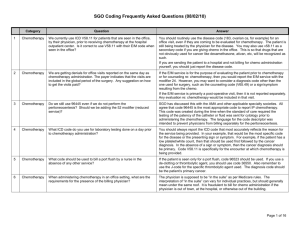
How do I know what I can bill
together?
National Correct Coding Initiative Edits
(NCCI)
– Allows bundling of services together by using a
modifier
– Shows what services can not be billed
together.
– Resource Website http://www.cms.gov/Outreach-andEducation/Medicare-Learning-NetworkMLN/MLNProducts/downloads/How-To-UseNCCI-Tools.pdf
Example of NCCI Edit
CPT only copyright 2011 American Medical Association. All rights reserved.
National Correct Coding Edits
Column I Code: Comprehensive procedure
includes all the codes listed in column II
component codes
Column II Code: Component of
comprehensive procedure
Indicator 0- Not allowed even with
modifier
Indicator 1- Allowed with appropriate
modifier ( usually but not always 59
modifier
Indicator 9 – Edits are no longer active;
code combinations are billable, and no
modifier is needed
Types of Modifiers
Modifier 25 – separate identifiable
evaluation and management service by
same physician or other healthcare
professional on same day of procedure
Modifier 59 – separate and distinct
procedure
Modifier 50 – bilateral procedure
NCCI Edit Example
Mr
Jones has been treated in your
clinic for a abdominal wound where
debridement and negative pressure
wound therapy has been performed.
He has Medicare.
Will
both procedures be reimbursed?
Can
we add a modifier?
Questions
Review 2012 Coding Updates
Medical debridement (active wound
management)
– 97597 first 20 sq cm
– 97598 each additional 20 sq cm
Surgical debridement codes, depth of
tissue not per wound
– First 20 sq cm (11042, 11043, 11044)
– Each additional 20 sq cm (11045, 11046 and
11047)
– “Only bill for the area of the wound that was
debrided “– CPT Assistant May 2012
Example
MR.
Jones is a patient that has a 5 x
5 x 3 pressure ulcer on his sacrum.
You sharply debride devitalized
tissue from the entire wound surface.
How would you bill?
5x5 = 25 sq cm;
Bill one unit of 97597 and one unit of
97598
Questions?
Multi-Layer Compression
29581
redefined- include leg (below
knee), including ankle and foot
Addition of Multilayer Compression
Codes
– 29582 – Application of multi layer
compression system; thigh and leg,
including ankle and foot
– 29583- ……; upper arm and forearm
– 29584 …….; upper arm, forearm, hand
and fingers
Skin Substitute Graft Codes
All
Graft codes now are the same
15271, 15272- apply to trunk,
arms,
legs,
15275, 15276- scalp, eyelids,
mouth , neck , hands, and feet
For Grafts over 100 sq cm based on
% of body
15273, 15274, 15277, 15278
Medicare Physician Fee Schedule
Fee schedule is a list of CPT codes that are
given a value based on a formula for
payment
Fee schedule is set by your MAC
Medicare pays 80% of physician fee
Patient pays 20% or if they have a
secondary insurance
Documentation
If
its not documented it didn’t
happen
Documentation should reflect
objective data and goals
Documentation should reflect
services that are medically necessary
and meet utilization guidelines
Audits
Do
internal audits of documentation
often identify areas of improvement
Prepare
The
for auditors
question is not if I will be
audited or when?
Meaningful Use
American
Recovery and
Reinvestment Act of 2009 specifies 3
components:
– Use of certified HER in a meaningful use
as E- Prescribing
– Use of EHR technology for electronic
exchange of health information to
improve quality of care
– Use of HER to submit clinical quality and
other measures
Therapy Cap and G Codes
Taxpayer
Relief Act 2012
– Outpatient hospitals will fall under
therapy cap through 2013
– Exceptions extended through
12/31/2013
– Therapy provided in critical access
hospitals (CAH) now subject to cap
Therapy Cap
Therapy
Cap
– $1900 dollars for Physical Therapy and
Speech Therapy combined
– KX modifier required if cap is exceeded
and greater than $1900
– If dollars extend greater than 3700 the
record is subject to medical manual
review
Functional Limitation Reporting
All outpatient rehab, part A and part B will
be required to report functional limitations
in Jan 1 to July 1, 2013 as a testing period
Claims submitted after July 1, 2013
without G codes will be unpaid
Data collection is to assist in future
payment system
Therapist driven, not billing
– Functional reporting must be documented by
therapist based on individual function
Documentation
Documentation
needs to include:
– Functional Limitation documented in
chart
– Assign Category and G codes
– Assess and Report Severity
Example of G Codes
Severity Codes
APTA STATEMENT
Program Basics
Therapists will use valid and reliable
assessment tool(s) and/or objective
measure (s) in determination of the
severity of the functional limitation
– Multiple tools may be used
– Therapist judgment may be used in the
severity modifier determination in combination
with the data gathered
– Documentation of G-codes and the rationale
for selection must be included in the medical
record
2013 Wound Care Updates
Surgical Package Definition
– Identifies any supplies that are being billed
outside of what is required for procedure
3 collagen dressing codes have been
redefined with removal of word “pad”
Manual Therapy Code
– Considered by CPT a separate and distinct
service and can be reported together when
performed with multi layer compression
More Updates
6 New Q codes for biologicals
- Q4131 – Q4136 – may not be covered by some
MACS
Definition of Modifier 25 has been revised
Definitions changed throughout CPT
“Providers” to “professionals”
“Practitioners” to “individuals”
“Physician” to “qualified healthcare professional
or individual”
New Negative Pressure
NOT a replacement for 97605 and 97606
G0455 – Negative Pressure Wound
Therapy using a mechanical powered
device, not durable medical equipment,
including provision of cartridge and
dressing , topical application and
instructions for ongoing care; total wound
surface area less than 50 sq cm
G0456 - …………; Greater than 50 sq cm
Websites
Physical Therapy State Practice Act
– www.fsbpt.gov
www.apta.org
http://www.apta.org/Payment/Medicare/
CodingBilling/FunctionalLimitation/
www.cms.gov
– Local coverage and national coverage decisions
Questions?
melissa.johnson@piedmont.org