Neutropenia - Grrr-OH
advertisement
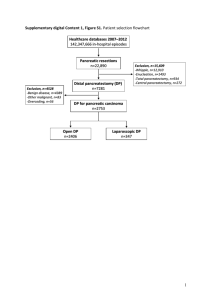
Élie AZOULAY Hôpital Saint-Louis, Service de Réanimation Médicale Université Paris-Diderot, Sorbonne Paris-Cité Groupe de Recherche Respiratoire en Réanimation Onco-Hématologique (GRRR-OH) Respiratory events in hematology patients Author Patients Incidence Time Finding Mortality Azoulay 2004 Medicine All 7-12% (203/3782) ~ Undetermined diagnosis 47.7% Puig. 2007 Leuk Lymphoma AutoBMT 15% (49/326) J11 Myeloma Neutropenia 51% vs. 8% Specchia 2003 Leuk Lymphoma AL 27.7% (80/288) / AML>ALL No remission Age Sortie d’aplasie Chaoui 2004 Leukemia AL ICU admission 35% vs. 6% 46% (30/65) / Three major advances: - Leukemic infiltrates - Non invasive diagnostic strategy - ARDS Pneumonia during chemotherapy in Patients with Acute Leukemia Garcia et al. Annals of the ATS, Vol. 10, No. 5 (2013), pp. 432-440. 85 Early Stage = 11% 148 throughout induction = 21% MDS > AML > ALL 801 AML/ ALL/ MDS 28-day Risk factor mortality for pneumonia are Age>60 6% without years, pneumonia AML,with pneumonia 26% ↑Low ICUplatelet length count, of stay ↑Low Hospital albumin length level, of stay ↑Neutropenia Costs Leukemic infiltrates: Vincent F, Rev Mal Respir 2012 Pulmonary leukostasis Leukemic infiltration Lysis pneumopathy Pulmonary leukostasis: ALI Quantitative “Pulmonary hyperviscosity” Rapidly growing hyperleukocytic AML. Constant if >200 000/mm3. Endothelial injury and activation from microvascular invasion related to hyperviscosity, leukocytic microthrombi, oxygen steal and hypoxia. Clinical manifestations of leukostasis Central nervous system circulation Headache, confusion, somnolence, dizziness, slurred speech, impaired hearing, tinnitus, diplopia, delirium, stupor, coma Retinal vein distension, retinal hemorrhage, papilledema Intracranial hemorrhage Penile circulation Priapism Cardiovascular system Acute myocardial infarction Right ventricular overload Acral lividosis Rapidly rising white-cell count Cell type (monoblasts) A postmortem examination revealed profound leukostasis in the heart, lungs, adrenal glands, liver, and spleen. Sludging of high numbers of leukocytes in small vessels (brain, lungs, and kidneys) Leukemic pulmonary infiltrates Blasts are aggregated in vascular lumens The infiltrates typically follow the lymphatic routes along the bronchovascular bundles, interlobular septa, and pleural interstitial tissue. Lysis pneumopathy: DAD Occurs immediately or early after chemotherapy Diffuse alveolar damage LEUKEMIC INFILTRATION leukemic infiltration of the alveolar capillaries LEUKOSTASIS Filling of a pulmonary artery with leukemic cells, as well as leukemic infiltration of alveolar capillaries. Catching up errors Valentino et al. CHEST. 2005,128(5):3629-3633 monoblaste Timing Poumon leucémique: prise en charge Infiltration pure: VNI, chimiothérapie classique, inhibition de l’adhésion du monoblaste sur l’endothélium pulmonaire (DXM?) Leucostase ou leucostase + infiltration: Essai de VNI, cytoréduction (Hydréa) DXM? Poumon de lyse (DAD) Intubation et optimisation des échanges gazeux Attendre et éviter l’infection Moreau AS et al. Submitted 2012 Mamez & Lengliné. In preparation Three major advances: - Leukemic infiltrates - Non invasive diagnostic strategy - ARDS Invasive or noninvasive ? Invasive: Biopsy Semi-invasive: FO-BAL Non invasive: Blood cultures Sputa Induced sputa NPA/swabs Viral PCR Pan-PCR Mass spectrometry Antigenes Echography HRCT Clinical Assessment for Identifying Causes of Acute Respiratory Failure in Cancer Patients Schnell D et al. European Respiratory Journal 2012 Culture based and non-culture based tools Culture-based Non culture-based Sang Scanner Crachats Aspergillus LBA galactomannan (GM), 1,3-beta-D-glucan Méthodes moléculaires Pathogènes colonisant Faux positifs Faux négatifs Pas de gold standard Trop sensibles? Colonisation ou infection Pertinence? The MiniMax study, Azoulay et al. 2010 Etiologies MAXI N=113 MINI N=106 Bacteria 47 (41%) 39 (37%) Viruses 7 (6%) 19 (18%) Fongi 14 (12%) 9 (8.5%) Pneumocystis 9 (8%) 10 (9.4%) Malignant infiltration 10 (9%) 6 (6%) Cardiac Pulm. Edem 7 (6%) 3 (3%) More than one diagnosis 9 (8%) 9 (8.4%) Diagnoses CPO: 10 Diagnosis made by NIT 10 (100%) Fungi: 23 22 (95.6%) Aspergilus: 18 17 (94%) Virus: 26 24 (92.3%) Malignancy: 16 13 (81%) Pneumocystis: 19 15 (79%) Bacteria: 86 57 (66.3%) Need for mechanical ventilation P=0.62 0. 0.2 Cumulative in and mec 0.0 Day-28 survival 0 5 10 15 20 25 28 0.6 0.4 0.2 0.0 Cumulative Survival 0.8 1.0 Time (days) after ICU admission 0 5 10 15 20 Time (days) after ICU admission 25 28 MiniMax dans le détail Rentabilité du LBA Rentabilité du LBA TOUS 18% Nodules centrolobulaires 5% Neutropéniques 10% Nodules sous pleuraux 4% Non Neutropéniques 20% Consolidations alvéolaires 20% Lymphoïde 40% Verre dépoli diffus isolé 40% MiniMax 2 Corrélation clinico – radiographique – morphologique Stratégie diagnostique adaptative Utilisation de PCR pan-pathogène: bactéries, fungiques, virus … Critères de jugement clinique pour éviter d’inclure 2000 patients: morbi-mortalité Three major advances: - Leukemic infiltrates - Non invasive diagnostic strategy - ARDS Five evidence in the literature Heterogeneous (at least) disease Few positive trials, good negative trials Clinical – pathological discrepancies Berlin Definition Scarce data ARDS and neutropenia Funny paradox (Frederic Ognibene) Pathophysiology Infection / infiltration / toxicity Used to be associated with poor outcomes Neutropenia recovery Two recent papers Turkoglu et al. (2013) Acute respiratory distress syndrome in patients with hematological malignancies. Hematology 18:123-130 • 68 patients with hematological malignancies and ARDS. PO2/FiO2 was 104 (74-165). 10 (15%) NIV, 21 (31%) VM, and 36 (53%) both • ICU mortality was 77% in the cohort. • >two organ failures was the only independent risk factor for mortality (P = 0.045), whereas NIV was associated with low mortality (P = 0.001). Soubani et al. (2014) The outcome of cancer patients with acute respiratory distress syndrome. J Crit Care 29:183 e187-183 e112 • ARDS Network randomized controlled trials: 116/ 2515 patients • Patients with cancer had significantly higher mortality (55.2%) compared with those without cancer (24.3%) (P < .0001): OR 2.54 (95% confidence interval [CI], 1.570-4.120). • APACHE III and age 6084 cancer patients admitted to 14 ICUs 3042(50%) patients with acute respiratory failure 1117 (36.7%) ARDS patients according to the Berlin definition Grrr-OH, 1990-2011 113 patients not included ╬ 1004 ARDS patients included Mild ARDS: 252 (25.1%) Moderate ARDS: 426 (42.4%) Severe ARDS: 326 (32.5%) Mortality: 59% Mortality: 63% Mortality: 68.5% Study population (N=1004) Survivors (N=364) Nonsurvivors (N=640) P value Male gender 642 (63.9%) 240 (65.9%) 402 (62.8%) 0.32 Age (y) 58 [48-67] 57 [47-67] 58 [48-67] 0.33 Median (IQR) or n (%) Underlying malignancy Acute leukemia 298 (29.7%) 96 (26.4%) 202 (31.6%) 0.08 Non-Hodgkin’s lymphoma 318 (31.7%) 115 (31.6%) 203 (31.7%) 0.97 Myeloma 113 (11.3%) 34 (9.3%) 79 (12.3%) <0.0001 Solid tumor 147 (14.6%) 60 (16.5%) 87 (13.6%) 0.21 Miscellaneous 95 (9.5%) 46 (12.6%) 48 (7.7%) 0.01 Allogeneic BMT/HSTC* 115 (11.5%) 36 (9.9%) 79 (12.3%) 0.23 Neutropenia 444 (44.2%) 148 (40.7%) 296 (46.3%) 0.08 Stage Progressive Partial/complete remission Newly diagnosed Unknown 0.0003 458 (45.6%) 171 (47.0%) 287 (44.8%) 237 (23.6%) 100 (27.4%) 137 (21.4%) 72 (7.2%) 33 (9.1%) 39 (6.1%) 237 (23.6%) 60 (16.5%) 177 (27.7%) Etiologies Median (IQR) or n (%). Cause of ARDS Pulmonary infection # Secondary ARDS# Fungal infection& Pneumocystis No definite diagnosis§ Organ Support NIV NIV failure Endotracheal MV Vasopressors Renal replacement therapy Study Survivors (N=364) populati on (N=1004) Non- P value* 662 (65.9%) 281 (77.2%) 381 (59.5%) <0.0001 225 (22.4%) 55 (15.1%) 170 (26.6%) <0.0001 293 (30.7%) 83 (23.2%) 210 (35.1%) 0.0001 64 (6.4%) 41 (5.7%) 30 (8.2%) 34 (5.3%) 0.07 12 (4.5%) 29 (6.4%) 0.29 survivors (N=640) 387 (38.6%) 174 (47.8%) 213 (33.3%) <0.0001 276 (27.5%) 173 (27.0%) 0.67 600 (93.8%) 490 (76.6%) 207 (32.3%) <0.0001 0.0004 0.09 103 (28.3%) 893 (88.9%) 293 (80.5%) 731 (72.8%) 241 (66.2%) 306 (30.5%) 99 (27.2%) Berlin definition Figure 3. 1 P<0.0001 0.8 0.6 Mild ARDS 0.4 0.2 Severe ARDS 0 0 20 40 60 Days 80 100 1990-2001: trends in outcomes Hospital mortality 1 0.8 0.6 0.4 0.2 0.0 Determinants of hospital mortality Solid tumor Need for emergency surgery Allogeneic BMT/HSCT mSOFA (per point) Cause of respiratory involvement No definite diagnosis Primary ARDS Secondary ARDS Invasive fungal infection Ventilation NIV NIV failure Endotracheal MV ARDS severity Mild Moderate Severe OR 95%CI 0.51 (0.34-0.77) 0.002 0.61 (0.35-1.05) 0.07 1.71 (1.07-2.71) 0.04 1.11 (1.06-1.16) <0.001 0.41 (Reference) (0.20-0.88) 0.02 0.90 (0.41-2.01) 0.80 1.72 (1.25-2.37) 0.001 2.93 (Reference) (1.80-4.79) <0.001 3.24 (2.02-5.24) <0.001 1.25 (Reference) (0.88-1.78) 0.22 1.61 (1.10-2.36) 0.01 1 1 1 P value ARDS and Aspergillus Monocyte de-activation Copland, AJRCCM, 03 T cells switch to TH2/TH3 PLötz et al, Crit Care Med, 04 Increase anti-inflammatory CK (IL-10, TNF-r1, IL-1ra) Park et al, AJRCCM, 01 In a case-control study, ARDS was independently associated with positive Aspergillus in the LRT OR= 2,36 [1,144,89] (p=0,02) Vandewoude, Crit Care, 06 8/64 patients with IPA Invasive fungal infection and ARDS Need for additional descriptive data Need for better understanding of the risk factors Differences across IFI IPA Zygo Other mould / fungi Pneumocystis Towards primary preventive strategies? Noninvasive fungal diagnostic kit Second confirmatory data set First study to be launched in the European group Observational data EORTC criteria (customized) Relationship between ARDS etiology and outcomes Prophylaxis Three major advances: - Leukemic infiltrates - Non invasive diagnostic strategy - ARDS