Statins in ARDS
advertisement

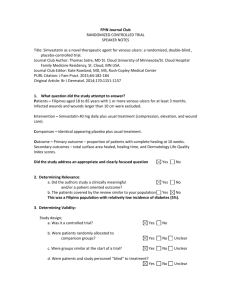
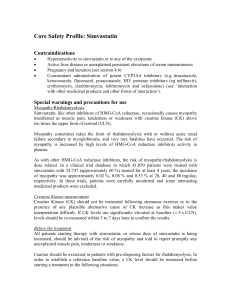
Statins in ARDS Danny McAuley Queen’s University of Belfast Scottish Combined Critical Care Conference September 2010 Novel therapies for ARDS - What is on the horizon? Conclusions • Beta agonists – Potential benefit in phase II study – Phase III multi-centre clinical trials awaited • Potential therapeutic interventions in phase II trials – APC – Statins • Novel potential future treatments – Modulation of renin-angiotensin system – Stem cell therapy Scottish Critical Care Trials Group June 2007 Statins in ARDS • • • • • Mechanism of action Observational data Statins and pulmonary inflammation Phase 2 clinical trial (HARP) HARP-2 No pharmacological treatment for ALI Cecilia O’Kane Ashbaugh et al. described using “a clinical trial of a variety of drugs, respirators and fluid regimens” with limited success Ashbaugh et al. Lancet 1967 Step-wise approach to new therapies McAuley et al. CCM (in press) Cellular effects of statins Simvastatin reduces thrombin-induced endothelial injury Jacobson et al. AJRCMB 2004;30:662 Simvastatin attenuates LPS-induced experimental lung injury Jacobson et al. AJP Lung 2005;288:L1026 Observational data to support a role for novel therapies in ALI 40% Mortality (%) 34% OR 0.27 (0.06-1.21) p=0.09 30% 21% 20% 10% No statin n = 164 Irish Critical Care Trials Group. Critical Care 2008;12:R30 Statin n = 24 Pre-treatment with simvastatin attenuates systemic inflammation following LPS challenge Steiner et al. Circulation 2005; 111:1841 Inhaled LPS as an in vivo model to study pulmonary inflammation in healthy subjects FEV1 BAL 6 hr FEV1 Plasma 50 µg LPS inhalation E. Coli serotype O26:B6 (Sigma) Breath activated dosimeter FEV1 Plasma 18 hr Inhaled LPS induces inflammatory O’Kanecompartment cytokines in Cecilia pulmonary Simvastatin in the inhaled LPS model of ALI Treatment with a clinically relevant dose of simvastatin will reduce pulmonary inflammation induced by LPS inhalation in humans Shyamsundar et al. AJRCCM 2009 179:1107-1114 Schedule for patient safety monitoring Simvastatin decreases pulmonary neutrophilia following LPS inhalation Total cells (x 105/ml) Neutrophils Macrophages Lymphocytes P Placebo Simvastatin value (n=10) (n=20) 15.2 10.7 0.2 (10.3-49.8) (4.6-17.4) 8.5 3.0 0.05 (4.4-16.2) (1.8-8.1) 7.0 5.1 0.48 (3.1-19.1) (2.1-13.0) 1.1 0.9 0.37 (0.6-3.2) (0.2-1.6) Simvastatin increases neutrophil apoptosis following LPS inhalation * p < 0.05 vs placebo Simvastatin decreases pulmonary neutrophilic activity following LPS inhalation * p < 0.05 vs placebo Simvastatin decreases pulmonary TNF following LPS inhalation * p < 0.05 vs placebo Simvastatin pre-treatment reduces systemic inflammation following LPS inhalation 80 Plasma CRP (mg/L) Placebo Simvastatin 60 * 40 20 0 * p < 0.05 vs placebo Simvastatin decreases pulmonary MMP secretion following LPS inhalation * p < 0.05 vs placebo Simvastatin pretreatment reduces nuclear NFκB translocation in monocyte-derived macrophages p = 0.0001 for control vs. placebo BALF; ** p=0.03 for placebo BALF vs. simvastatin BALF; # p=0.03 for placebo BALF vs. simvastatin + placebo BALF Lovastatin decreases pulmonary inflammation measured by FDG PET following LPS instillation Chen et al. AJRCCM 2009 180:533-539 FDG PET can detect pulmonary inflammation in patients with ALI Bellani et al. Critical Care Medicine 2009 37:2216-2222 HMGCoA reductase inhibition in ALI to Reduce Pulmonary oedema (HARP) • • • • Proof of concept single centre trial Prospective double blind Within 48 hours of onset of ALI Randomised to simvastatin 80mg or placebo for up to 14 days • Outcomes: – Extra-vascular lung water – Pulmonary function and systemic organ failure – Safety – Biological markers in plasma and BAL Craig et al. AJRCCM 2010 (in press) Exclusion criteria Cecilia O’Kane • • • • • Age < 18 years Pregnancy Drug interactions Declined consent Participation in a clinical trial within 30 days • Current treatment with statins • Creatinine kinase (CK) > 10 times upper limit • Transaminases > 3 times upper limit Patient demographics Simvastatin n=30 Placebo n=30 p value 52.5 (17.1) 52.8 (20.0) 0.95 73 73 1.00 APACHE II 25.1 (6.5) 23.3 (6.8) 0.30 APACHE II predicted mortality (%) 45.6 (25.0) 46.1 (24.7) 0.93 SAPS II 53.4 (14.4) 54.2 (14.3) 0.83 SAPS II predicted mortality (%) 51.2 (25.2) 53.6 (24.9) 0.72 15 (50) 15 (50) 1.00 Age (years) Gender (% male) Sepsis n (%) Simvastatin improves oxygenation index Cecilia O’Kane n =30 n=30 n=10 n=9 Simvastatin reduces plateau pressure Cecilia O’Kane n=30 n=30 n=10 n=9 Simvastatin improves sequential organ Cecilia O’Kane failure assessment (SOFA) score n=30 n=30 n=10 n=9 Safety profile Cecilia O’Kane Simvastatin Placebo CK > 10 times ULN (%) 4.5 8.7 0.58 ALT > 3 times ULN (%) 4.4 8 0.60 AST > 3 times ULN (%) 8.3 16.7 0.34 Adverse events (%) 47 43 0.79 Serious adverse events (%) 20 23 0.75 p value • No serious adverse events due to study drug occurred Outcome data Cecilia O’Kane Simvastatin Placebo p value ICU free days 8.2 (8.1) 7.20(7.47) 9.1 (8.7) 8.4 (8.4) 0.7 0.6 ICU survival n (%) 21 (70%) 21 (70%) 1.0 51.2 (39.3) 48.0 (37.4) 0.8 19 (63%) 19 (63%) 1.0 Ventilator free days Hospital LOS (days) Hospital survival (days) Simvastatin decreases bronchoalveolar lavage IL-8 Cecilia O’Kane pp=0.89 = NS *p = 0.05 IL-8 10000 (pg/ml) 8000 Placebo Simvastatin 6000 4000 2000 0 D0 n=17 D3 D0 D3 n=10 n=23 n=17 Simvastatin decreases bronchoalveolar lavage IL-6 p=0.43 p = NS p = 0.07 IL-6 5000 (pg/ml) 4000 Placebo Simvastatin 3000 2000 1000 0 D0 D3 n=17 n=10 D0 n=23 D3 n=17 Simvastatin decreases systemic inflammation asCecilia measured O’Kaneby plasma CRP CRP (mg/L) 400 pp=0.06 = NS *p = 0.0004 Placebo Simvastatin 300 200 100 0 D0 n=30 D14 n=9 D0 n=29 D14 n=8 Conclusions • In a human LPS model of ALI simvastatin reduces pulmonary and systemic inflammation • In patients with ALI simvastatin – Improves pulmonary and non-pulmonary organ dysfunction – Well tolerated – Reduces inflammation • Study now needed to determine if simvastatin improves clinical outcome in large clinical trials HARP-2 Cecilia O’Kane Acknowledgements HMGCoA reductase inhibition in prevention of ALI (HARP-prevention) (http://www.controlled-trials.com/ISRCTN56543987) • Proof of concept, double blind, placebo controlled, single centre study • Study population – Patients undergoing oesphagectomy – N=30 of planned sample size 36 • Simvastatin 80mg or placebo • Endpoints: – Pulmonary dead space – Respiratory compliance, oxygenation index – Biological markers in plasma and EBC