7-23-14%20Rahil%20Shaikh%20MM
advertisement

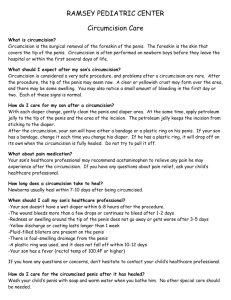
MORBIDITY & MORTALITY RAHIL “The Man Who Doesn’t Need To Shave To Look Good” SHAIKH, MD Northeast Iowa Family Medicine July 23rd, 2014 Sponsors Chief Complaint 1 day old M with unwanted foreskin. HPI Born to a 30 year old G3, now P3 mother via induced vaginal delivery (for post dates) at 40 1/7 weeks of gestation Mother’s prenatal Hx complicated by mild tobacco abuse but otherwise nothing else pertinent Baby was born on Tuesday April 29th, 2014 at 20:48 via NSVD with Apgars of 8 and 9, 3860 g (AGA) PMH, PSH, FH, SH • Nothing significant Review Of Systems Goal in life was to urinate on Dr. Shaikh multiple times Medications/Allergies None NKA Physical Examination Completely normal, healthy baby boy Assessment & Plan 1) Routine newborn cares 2) Bottle feed 3) Circumcision Timeline Of Events DATE CLINICAL STATUS 04/29 Birth at 20:48 Fed well, urinated, passed stool, VSS 04/30 Circumcision performed at lunch hour, preparations began ~ 12:30 Circumcision note signed at 14:15 Called in ~ 15:00 for bleeding circumcision site to the L of the ventral frenulum that was refractory to Surgicel Tried multiple variations of Surgicel and Surgifoam but bleeding wouldn’t stop Attending evaluated and used silver nitrate and then aluminum nitrate with temporary relief ~ 16:00 After family was with baby again, bleeding resumed Resident used Surgicel and Surgifoam technique assisted by Neonatologist to stop bleeding; baby was monitored by resident for 1 hour and hemostasis was once again temporarily achieved Called in ~ 19:00 for bleeding from same site refractory to multiple Surgicels Decision was made to re-do Surgicel/Surgifoam application and leave baby in warmer without diaper to have hemostasis achieved and maintained Timeline Of Events DATE CLINICAL STATUS 05/01 Checked in on baby ~ 05:30 and hemostasis had been achieved, same application of Surgicel that had been applied since the previous night was not soaked through with blood Discharged baby ~ 13:00 in great condition (no problems with urinating, feeding or vital signs) 05/02 Followed up in office, doing well, remnants of aluminum nitrate (black) still present but otherwise baby was in solid shape Did I do this? Was there something wrong with the way I performed the circumcision? Was it too early as well? Review Of Pertinent Literature World Health Organization: Manual For Early Infant Male Circumcision Under Local Anaesthesia, 2011 Review Of Pertinent Literature In healthy, term, stable male newborns, circumcisions can be performed anywhere between 12-24 hours after birth, as long as the baby has voided WHO and AAFP have the same stance I waited 16 hours after birth to perform the circumcision 12-24 hours does not apply to SGA babies, babies whose penile shaft length is < 1 cm, preterm babies, or those with a medical contraindication Review Of Pertinent Literature Removal of glandular adhesions should be done carefully, with frenulum on the ventral surface to be avoided Up and down motion with straight hemostat prevents frenulum damage I performed more side to side motions Review Of Pertinent Literature Gomco size 1.3 was accurate, no mismatch between bell and baseplate Risk of bleeding? 1.0% (similar to Plastibell and Mogen techniques) Most risk related to mismatching device parts Review Of Pertinent Literature After stem of the bell and foreskin are maneuvered through the hole in the baseplate, but before the device is clamped and tightened, the amount of penile shaft that remains below the clamp must be symmetrical and not stretched too tightly This crucial step was likely misjudged because there was too much foreskin taken off from the ventral surface Conclusions When performing a circumcision, be careful around the frenulum and always check below the clamp! If bleeding complication occurs, use Surgicel/Surgifoam, aluminum/silver nitrate, and worst case scenario, a suture (but obviously get help from Pediatrics/Neonatology unless you’ve done it before!); consider bleeding disorders for resistant cases Adverse Events & Outcomes CASE YES Unexpected death Medical or surgical complication NO X X Delay in care X Delay in diagnosis X Prolonged medical care in setting of poor prognosis X Other X Factors Contributing To Adverse Outcome FACTOR YES NO Communication: ex. inadequate handoffs, incomplete clinical information X Coordination of care: ex. involving multiple servies and/or care sites X Volume of activity/workload: ex. increased clinical volume and/or perception of workload X Escalation of care: ex. delay or failure to involve more senior physician or nurse X Recognition of change in clinical status: ex. delay or failure to recognize changing clinical signs +/- symptoms X Other: surgical technique X Root Cause Analysis: Fishbone Diagram Resident Circumcision Gomco vs. Plastibell Root Cause Analysis: Fishbone Diagram Improved technique Practice makes better Either method can create complications No death Comments & Discussion