ACC/AHA 2007 Guidelines on Perioperative
advertisement

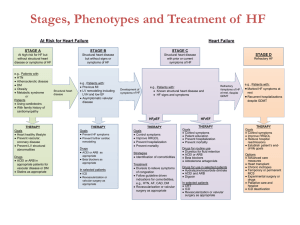
Peri-Operative Management of Drug Eluting Stents Stephen T. Thew, MD, FACC Heart Clinics Northwest Balance Bleeding Stent Thrombosis Outline/Highlights Timing of elective surgery What to do with medications • Stopping anti-platelet meds • When to restart Post operative concerns Timing of Surgery Post-Stenting Bare Metal Stents • Wait 30-45 days for elective surgery • But do it prior to 6 months (or wait > 1 yr) Drug Eluting Stents • Wait at least 6 months for elective surgery • Ideal - 1 year for elective surgery (??) Anti-platelet medications If possible continue all anti-platelet medications If Plavix (P2Y12) must be stopped do so 5-7 days before surgery and re-start ASAP with 300-600mg bolus REALLY try to continue aspirin, if stopped do so 5 days before and restart ASAP Anti-platelet medications Consider “bridging therapy” with IV administration of IIb/IIIa inhibitor (short half-life) in certain situations If bridging, start IV IIb/IIIa 2-3 days prior to surgery Post operative concerns Close monitoring for bleeding Chest pain, hypotension, tachycardia all need very prompt attention Elective surgery should be done at hospital with 24 hour availability of PCI capable cath lab Peri-op DES: Scope of the Problem In the US over 600,000 percutaneous coronary interventions (PCI) are done every year The majority of PCIs involve drug eluting stent placement Peri-op DES: Scope of the Problem Dual Anti-Platelet Therapy (DAPT) includes aspirin in addition to a P2Y12 inhibitor (Plavix, Prasugrel, Brilinta, Ticlid) Following Drug-Eluting Stent (DES) placement, DAPT is recommended for 12 months by ACC/AHA guidelines Peri-op DES: Scope of the Problem • About 5% of patients undergoing PCI will need non-cardiac surgery within 1 year • About 30,000 procedures annually • Roughly 1% of elective non-cardiac surgery pts. had PCI in the preceding year Peri-op DES What Problems are There? • Increased risk of myocardial infarction • Risk of stent thrombosis • Increased risk of bleeding due to DAPT • Migration of the stent ? • Interference with diagnostic/imaging studies? Why do Cardiologists have a love affair with DES? Because they work so well Work well for what? Compared to what? Are there alternatives besides DES? Brief history of Coronary Revascularization Surgical Bypass (CABG) • Prior to the 1960s angina was treated with Nitroglycerin • Vineberg procedure had been occasionally used (LIMA grafted directly to the anterior wall myocardium) • 1967 the first CABG was performed at the Cleveland Clinic – an SVG placed to LAD Brief history of Coronary Revascularization Limitations of CABG • Surgery required • Prolonged recovery times, in hospital and at home • Repeat procedures can be done, but limited by available conduit, increased morbidity and again prolonged convalescence Brief history of Coronary Revascularization Balloon Angioplasty (PTCA) In 1977 Andreas Gruentzig preformed the first balloon angioplasty in Zurich, Switzerland Recovery time was minimal, cost was lower, repeat procedures were more practical than re-do CABG Brief history of Coronary Revascularization Limitations to PTCA Complications • • • • Acute vessel closure Dissection Intra-coronary thrombus Emergent CABG Durability • Restenosis • Elastic Recoil • Intimal Hyperplasia Brief history of Coronary Revascularization Coronary Stenting • In 1994 the FDA approves the use of coronary stents • By the late 1990’s about 85% of coronary interventions utilized stents • Restenosis reduced from 30-40% to 20-30% • Many of the limitations of PTCA were treated/prevented with stents Brief history of Coronary Revascularization PTCA limitations now treated by stents Complications • Acute vessel closure • Dissection Durability (Restenosis) • Elastic Recoil – essential resolved • Intimal Hyperplasia – actually worsened • Net effect was still significant reduction in restenosis Brief history of Coronary Revascularization Limitations of Stents Stent Thrombosis • Ticlid in addition to aspirin markedly reduced SAT • Formed the concept of DAPT • Plavix (clopidogrel) replaced Ticlid in late 1990’s Durability – (Restenosis) • Elastic recoil resolved, but neointimal hyperplasia got worse • Restenosis rates were 20-30% • Small Vessels, Diabetics, diffuse disease all had even higher restenosis rates Brief history of Coronary Revascularization Drug Eluting Stents 2003 the first DES is approved by FDA DES deliver locally, a high dose of a chemotheraputic agent to inhibit neointimal growth Restenosis rates dropped to around 4-5% Why Cardiologists Love DES • PCI reduces mortality and morbidity in acute coronary syndromes • PCI is effective in controlling anginal symptoms • Patient recovery time is short • Essentially unlimited future procedures can be preformed if needed • Long term durability is very good Limitations of Drug eluting stents • Increased, but later, stent thrombosis in DES • Late (>30 days) • Very Late (>1 year) • Inhibition of neo-intimal growth also inhibits endothelial formation inside the stent • Long term (12 month) Plavix was recommended In-stent Restenosis/Endothelialization Bare-metal stents have essentially complete endothelialization at 4 – 6 weeks DES at 180 days may still have some incomplete endothelialization Stent Thrombosis Stent thrombosis ◦ ◦ ◦ ◦ Acute –first 24 hours Sub-acute – first month Late – first year Very late - > 1 year Overall stent thrombosis rate is 1-2 % in first year Continues to be a major concern Stent Thrombosis During surgery there is a hypercoaguable state induced Increased inflammation and platelet activation A greater degree of hypercoaguability is seen from surgery than during an MI Stent Thrombosis Post surgery rise in thrombogenic risk - increased catecholamine release - increased platelet aggregation - decreased fibrinolysis Stent Thrombosis Discontinuation of aspirin leads to a ‘rebound’ effect Anti-Platelet Agents in Addition to Aspirin Oral • • • • Ticlid Plavix Effient Brilinta IV • ReoPro • Integrlin • Aggrastat Oral Anti-Platelet Agents P2Y12 Inhibitors or ADP Receptor Inhibitors Thienopyridines • Ticlid (ticlopidine) • Plavix (clopidogrel) • Effient (prasugrel) Non-thienopyridines • Brilinta (ticagrelor) • Peak inhibition in just 2 to 4 hours Anti-Platelet Agents IV - P2Y12 Inhibitors Currently – none available Cangrelor is being studied with PCI IV administration, 3 to 5 minute half life Was studied in BRIDGE for pre-op use IV Anti-Platelet Medications Glycoprotein IIb/IIIa Inhibitors ReoPro (abciximab) • Monoclonal anti-body, irreversible binds platelet • Reverse with platelet infusion Aggrastat (tirofiban) Integrlin (eptifibatide) • Synthetic peptides, competitive binding to platelet • Platelet transfusions don’t help – (out competed) • Short ½ life – gone in 2 to 4 hours Dual Anti-Platelet Therapy (DAPT) Aspirin and a P2Y12 inhibitor Duration: 4 weeks following bare metal stent 12 months following DES 12 months following MI Continuation of aspirin indefinitely Bleeding Risk During Surgery Burger, et al – 49,000+ patients, increased bleeding by 1.5, but mostly ‘nuisance’ bleeding Intracranial procedures did have increased fatal bleeding TURP may have increased severity level of bleeding Bleeding Risk with Surgery • There is a decrease in CVAs during CEA with pts on aspirin • Better patency of grafts in CABG and vascular by-pass in patients on aspirin • Increased need for blood products, but no increased mortality in CABG patients on Plavix and aspirin Bleeding Risk with Surgery Burger, et al – 49,000+ patients Stopping aspirin had higher cardiac, cerebral and peripheral vascular events Surgical Risk and Timing Non cardiac surgery done less than 6 weeks after PCI has the highest mortality The single biggest predictor of stent thrombosis is discontinuation of anti-platelet therapy Surgical Risk and Timing Retrospective study – Ontario, Canada ONLY elective surgeries Increased MACE when <45 days Bare-metal – optimal time 46 – 180 days DES – optimal time >180 days > 1 year and risk has plateaued, is no higher than 2-10 years post PCI Wijeysundera, et al Surgical Risk and Timing At > 1 year since PCI the risk approximates that of a intermediate nonrevascularized patient with 1 or 2 clinical risk factors Wijeysundera, et al Peri-op Management of DES • Currently no definitive standard of care, mostly expert opinion • Without good prospective data, management is carried out on individual case basis • Length of stent, location, bifurcation, multi-vessel Strategies for Peri-op Management of DES ELECTIVE SURGERY • Elective surgery should be delayed at least until 6 months post DES • Ideally postponed 1 year post DES • P2Y12 - if stopped - 5 to 7 days pre-op, continue aspirin if at all possible • Resume P2Y12 ASAP with 300 or 600mg loading dose Strategies for Peri-op Management of DES • • • • • • • “Bridging Therapy” with GP IIb/IIIa inhibitor Has NOT been rigorously studied Integrlin or Aggrastat, NOT ReoPro Stop Plavix 5-7 days pre-op Admit 2-3 days pre-op and start IIb/IIIa Continue aspirin throughout if possible Restart Plavix as soon as possible post-op Strategies for Peri-op Management of DES URGENT SURGERY • Urgent-Emergent surgeries have 4-fold higher mortality Strategies for Peri-op Management of DES URGENT SURGERY • Continue DAPT if possible - stent thrombosis risk is high • Closed/confined space – intracranial, spinal medullary, posterior chamber ophthalmic surgeries will need DAPT discontinued • If P2Y12 inhibitor stopped, try to maintain aspirin • Restart the P2Y12 inhibitor post surgery (within 24 hours if possible, with 300mg bolus). Strategies for Peri-op Management of DES Post Op issues Resumption of DAPT as soon as possible • Using bolus dose of P2Y12 inhibitor Intensive post–op monitoring if off DAPT Prompt evaluation and intervention for stent thrombosis or any bleeding Strategies for Peri-op Management of DES Post-op Stent Thrombosis • Usually presents as ST elevation MI • Fibrinolytic therapy is contraindicated • Primary PCI is the treatment of choice • When DAPT is interrupted prematurely for surgery it should be done at hospitals with 24 hour cath/PCI availability Strategies for Peri-op Management of DES Post-op Bleeding • Platelet transfusion is only somewhat effective with P2Y12 agents • It’s not effective with Integrlin or Aggrastat, but with short ½ life normal platelet function is restored in about 6 hours • RBC transfusion as needed Summary/Highlights Timing of elective surgery What to do with medications ◦ Stopping anti-platelet meds (DAPT) ◦ When to restart Post operative concerns Timing of Surgery Post-Stenting Bare Metal Stents • Wait 30-45 days for elective surgery • But do it prior to 6 months (or wait > 1 yr) Drug Eluting Stents • Wait at least 6 months for elective surgery • Ideal - 1 year for elective surgery (??) Anti-platelet medications If possible continue all anti-platelet medications If Plavix (P2Y12) must be stopped do so 5-7 days before surgery and re-start ASAP with 300-600mg bolus REALLY try to continue aspirin, if stopped do so 5 days before and restart ASAP Anti-platelet medications Consider “bridging therapy” with IV administration of IIb/IIIa inhibitor (short half-life) in certain situations Post operative concerns Close monitoring for bleeding Chest pain, hypotension, tachycardia all need very prompt attention Elective surgery should be done at hospital with 24 hour PCI capable cath lab availability Proposed Approach to the Management of Patients with Previous PCI Who Require Noncardiac Surgery Previous PCI Balloon angioplasty Drug-eluting stent Bare-metal stent <365 days Time since PCI <14 days Delay for elective or nonurgent surgery PCI, percutaneous coronary intervention >14 days >30- 45 days Proceed to the operation room with aspirin <30- 45 days Delay for elective or nonurgent surgery >365 days Proceed to the operating room with aspirin Proposed Treatment for Patients Requiring PCI Who Need Subsequent Surgery Acute MI, H risk ACS, or H risk cardiac anatomy Bleeding risk of surgery low Stent & continue dual antiplatelet therapy Not low Timing of surgery 14-29 days Balloon angioplasty 30-365 days Bare-metal stent >365 days Drug-eluting stent Thank you Preoperative Coronary Revascularization With CABG or Percutaneous Coronary Intervention Coronary revascularization before noncardiac surgery is useful in patients with stable angina who have: I IIa IIb III ● significant left main coronary artery stenosis ● 3-vessel disease (survival benefit is greater when LVEF <0.50) ● 2-vessel disease with significant proximal LAD stenosis & either EF<0.50 or demonstrable ischemia on noninvasive testing. Coronary revascularization before noncardiac surgery is recommended for patients with: ● high-risk UA/NSTEMI ● acute STEMI Preoperative Coronary Revascularization With CABG or Percutaneous Coronary Intervention I IIa IIb III I IIa IIb III In patients in whom coronary revascularization with PCI is appropriate for mitigation of cardiac symptoms & who need elective noncardiac surgery in the subsequent 12 months, a strategy of balloon angioplasty or bare-metal stent placement followed by 4-6 weeks of dual-antiplatelet therapy is probably indicated. In patients who have received DES & who must undergo urgent surgical procedures that mandate the discontinuation of thienopyridine therapy, it is reasonable to continue ASA if at all possible & restart the thienopyridine as soon as possible. Preoperative Coronary Revascularization With CABG or Percutaneous Coronary Intervention The usefulness of preoperative coronary revascularization is not well established in: I IIa IIb III High risk ischemic patients (e.g. abnormal dobutamine stress echo with at least 5 segments of wall-motion abnormalities) I IIa IIb III Low risk ischemic patients with an abnormal dobutamine stress echo (segments 1-4) Preoperative Coronary Revascularization With CABG or Percutaneous Coronary Intervention It is not recommended that routine prophylactic coronary revascularization be performed in patients with stable CAD before noncardiac surgery I IIa IIb III Elective noncardiac surgery is not recommended within: ● 4-6 weeks of bare metal coronary stent implantation or within 12 months of drug-eluding coronary stent implantation in patients in whom thienopyridine therapy, or ASA & thienopyridine therapy, will need to be discontinued perioperatively. ● 4 weeks of coronary revascularization with balloon angioplasty Drug Eluting Stents (DES) and Stent Thrombosis A 2007 AHA/ACC/SCAI/ACS/ADA science advisory report concludes that premature discontinuation of dual antiplatelet therapy markedly increases the risk of catastrophic stent thrombosis and death or MI. To eliminate the premature discontinuation of thienopyridine therapy, the advisory group recommends the following: • Before implantation of a stent, the physician should discuss the need for dual-antiplatelet therapy. In patients not expected to comply with 12 months of thienopyridine therapy, whether for economic or other reasons, strong consideration should be given to avoiding a DES. • In patients who are undergoing preparation for PCI and who are likely to require invasive or surgical procedures within the next 12 months, consideration should be given to implantation of a bare metal stent or performance of balloon angioplasty with provisional stent implantation instead of the routine use of a DES. Drug Eluting Stents (DES) and Stent Thrombosis • A greater effort by healthcare professionals must be made before patient discharge to ensure that patients are properly and thoroughly educated about the reasons they are prescribed thienopyridines and the significant risks associated with prematurely discontinuing such therapy. • Patients should be specifically instructed before hospital discharge to contact their treating cardiologist before stopping any antiplatelet therapy, even if instructed to stop such therapy by another healthcare provider. • Healthcare providers who perform invasive or surgical procedures and who are concerned about periprocedural and postprocedural bleeding must be made aware of the potentially catastrophic risks of premature discontinuation of thienopyridine therapy. Such professionals who perform these procedures should contact the patient’s cardiologist if issues regarding the patient’s antiplatelet therapy are unclear, to discuss optimal patient management strategy. Drug Eluting Stents (DES) and Stent Thrombosis • Elective procedures for which there is significant risk of perioperative or postoperative bleeding should be deferred until patients have completed an appropriate course of thienopyridine therapy (12 months after DES implantation if they are not at high risk of bleeding and a minimum of 1 month for bare-metal stent implantation). • For patients treated with DES who are to undergo subsequent procedures that mandate discontinuation of thienopyridine therapy, aspirin should be continued if at all possible and the thienopyridine restarted as soon as possible after the procedure because of concerns about late stent thrombosis.