Laboratory Test Utilization
advertisement

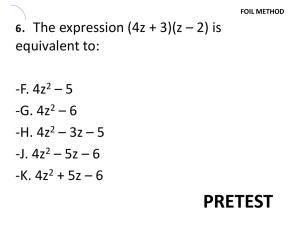
Laboratory Test Utilization: The Good, the Bad and the Overused Tim Hamill, MD Director, UCSF Clinical Laboratories The Good, The Bad & The Ugly • A ‘Good’ test: • Provides information that is useful in patient management decisions • Screening: High sensitivity & NPV • Diagnosis: High specificity & PPV • A ‘Bad’ test: • Uses resources but fails to provide information useful in patient management decisions • The ‘Ugly’ test: • Uses resources and provides information that is misleading or irrelevant UCSF Test Utilization • In 2009 UCSF performed an average of 486,000 tests per month • Annual test volume 5.8M • Inpatient tests : Outpatient tests = 1:1 • Inpatients: 15 tests/day • Outpatients: 4 tests per visit • Stat : Routine = 1:3 overall (1:1 inpatient) UHC Comparison Data UCSF Ranks #1 in Tests Used per Patient Discharged Causes of Test Overutilization* • Ordering test panels rather than ala carte’ • Ordering tests as groups • Repetitive test orders (esp. normal results) • Incomplete understanding re: impact of low pre-test probability • Poor understanding of the consequences of overutilization • Patient pressure • Defensive testing • Perverse financial incentives (more tests = more revenue) * Astion ML. 2006. Interventions that improve laboratory utilization: from gentle guidance to strong restrictions. Laboratory Errors and Patient Safety. 2(4):8-9 The Origin of Test Panels • Technicon SMAC (1974): • Sequential Multiple Analyzer with Computer Modern ‘Discreet’ Analyzers Ordering Test Panels • A study of orders for repeat electrolyte panels indicated that 10% were medically unnecessary and in 65% of cases a single test could have substituted for the entire panel. (Baigelman et al, Intensive Care Med, 11(6) 1985) Comparison of Electrolyte Orders: Individual vs. Panel Orders 140000 120000 Test Volume 100000 80000 Overall total Total as separate orders 60000 40000 20000 5013 4061 995 966 Na K Cl CO2 0 Impact of Electrolyte Reduction Ordering Tests in Groups • Redundant tests: • BUN & Creatinine • Troponin & CK-MB • ALT & AST • Tests that just seem to trip off the tongue: • Calcium, magnesium, phosphorus • PT & PTT • T3, T4 & TSH Separating BUN & Creatinine Repetitive Testing • A study of the impact on serum potassium orders using a simple algorithm based on prior tests being normal or abnormal could reduce potassium testing by 34% (Schubart et al, MEDINFO 2001) • Renal function: BUN, Creatinine • CBC & CBC w/differential Problems with Test Overutilization • Patient issues • Pain & morbidity from repeated venipunctures • Iatrogenic anemia • Medical issues • Follow-up on clinically irrelevant abnormals • Tracking just the ‘numbers’ instead of the entire clinical picture • Instituting inappropriate therapies • Economic & Environmental issues • Lack of reimbursement for inpatient testing • Biohazardous waste generation Studies on iatrogenic anemia • Smoller et al NEJM 314, 1986: • General wards: 1.1 draws/d, Ave. 12.4 mL/d, Total 175 mL for hospitalization • ICU: 3.4 draws/d, Ave. 41.5 mL/d, Total 762.2mL • ICU w/Art line: 4.0 draws/d, Total 944 mL • Low et al Chest 108(1) Jul, 1995: • Presence of Art. Line in ICU patients increased blood volume loss from phlebotomy by 44% Impacts of Iatrogenic anemia • Critically ill patients may not have the bone marrow reserve or erythropoietin drive to compensate for iatrogenic blood loss. • Transfusion to correct for this anemia has been shown to negatively impact long term survival • Other risks of phlebotomy: • Nerve damage, arterial damage, venous sclerosis, infection Irrelevant ‘abnormals’ • Virtually all quantitative laboratory test ‘normal ranges’ are based on the mean +/- 2 SD (95% confidence interval) for a subject population 2.5% 2.5% • 5% of normal patients will have values that lie outside this range (magnified for ill patients) Irrelevant ‘abnormals’ • If a patient has 10 tests ordered, each with a 5% chance that the test may have a result outside the normal range. Then there is a 50% chance that at least one test will have an ‘abnormal’ result • This is especially true with ordering chemistry ‘panels’ Economics & Environment • The vast majority of inpatient care is covered by DRG or per diem payments • Laboratory tests are not individually reimbursed and merely represent cost against the what the hospital is paid • The 3 UCSF Clinical Laboratories generate approx. 11,500 lbs of biowaste per month • Cost to incinerate this waste is approx. $88K per year The Solution? • Approaches that have been tried • • • • • • Place limits on housestaff orders Provide information on test costs Requisition design EMR warnings and reminders Education Incentives Factors that Impact Laboratory Test Results & Interpretation • Pre-analytic issues • Diagnostic testing issues • • • • • Pre-test probability Appropriateness of test in your patient Impact of the test result on care decisions Chasing ‘diagnostic certainty’ Impact of other disorders, therapy on results • Monitoring issues • Which test is going to be used? • How fast does the test change? • What is the impact of monitoring on clinical care? Factors Impacting Laboratory Tests Pre-analytic Test Issues • • • • Time of sample collection Proper collection technique Proper labeling Proper storage and transport Time of Collection • Relative to time of management decisions • Relative to therapy • Platelet counts after transfusion • Drug levels: relative to dose • Peak: PO vs. IV • Trough • Relative to time of day • Cortisol Proper Collection Technique • Prolonged use of tourniquet • IV’s and line draws • Order of collection • Trace metal (Royal blue), Blood cultures • Blue; Gold/Red; Green; Purple • Proper filling • Proper mixing • Special needs Proper Labeling • The person who collects a sample should label it • Double check the label before submitting • Special Blood Bank requirements • Check specimen • Body fluids • Lab policies on handling unlabeled and mislabeled samples Proper Storage & Transport • Refrigeration vs. Room temperature • Protection from light • Transport to the lab • Effects of cellular metabolism • Blood gas samples • Serum chemistries • Pneumatic tube considerations What is the effect of Pre-test probability? • The pretest probability of disease is critically important to test ordering • If the disorder has a low pretest probability then even a very sensitive and specific test may have little clinical utility • If the pretest probability is very high tests may not provide much (if any) additional ‘certainty’ of the diagnosis Low pretest probability example • You are thinking of ordering a test that is 95% sensitive and specific • The pretest probability that the disorder is present is, however, only 10% in your patient • Positive predictive value: 68% • Negative predictive value: 99% • only represents a 9% increase in certainty over the pretest probability • At a pre-test probability of 1% the PPV is only 16% and the NPV is 100% High pretest probability • The same theoretic test (95% sensitive and 95% specific) but in a patient with a 90% likelihood of having the disorder: • Positive predictive value: 99% (9% incr.) • Negative predictive value: 68% When do tests add the most information? • When the pretest probability is in the range of 30-70% • At a pretest probability of 50%, a test that is 95% sensitive and specific yields: • Positive predictive value: 95% • Negative predictive value: 95% Is the test appropriate for your patient? • How does the patient’s diagnosis impact the test? • VTE and Protein C/S levels • How does the patient’s treatment impact the test? • Galactose or Maltose containing medications and POCT Glucose testing • D-dimer in a surgical patient • How do other disorders impact the test? • HgbA1c and shortened red cell lifespan Impact of the test on patient care decisions? • Ask yourself….’What will I do if the test is negative/normal vs. positive/abnormal’ if the answer is essentially the same for both then the test has little utility • E.g. Haptoglobin in anemia • Will the result be available before the patient is discharged? • Chasing diagnostic ‘certainty’ • How much information is needed before a treatment is initiated or withheld? Questions to ask about tests used to monitor a patient • How fast do I expect the test to change? • What is the best monitoring test for the disorder in question? • Is more than one test needed? • How much change would trigger a therapeutic intervention? • Once an intervention is made is monitoring still needed? With the same test? At the same frequency? How fast do tests change? • While many test results can change rapidly in an individual there are other tests which may only change slowly or not at all over time • Positive serologic studies • Enzyme levels: AST T1/2 = 17 hr, ALT T1/2 = 48 hr, Alk Phos T1/2 = 7 d,, GGT T1/2 = 9 d (28 d in hepatic Dz) • D-dimers • WBC differential (if no change in WBC) • Understanding how rapidly a given analyte may change is important to selecting how often it should be ordered Laboratory Manual • The UCSF Clinical Laboratories maintain an online laboratory manual that is constantly updated • http://labmed.ucsf.edu/labman/ • It has important information about: • Sample type and amount, incl. minimums • Test availability and turnaround time • Patient preparation, collection instructions and sample handling • Test utilization tips