ITP - Dr/Mervat Hesham
advertisement

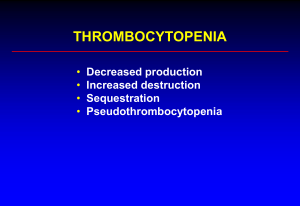
َ قالُوا ُس ْب َحا َن َك ال ِع ْل َم َل َنا إِال َ ْ ْ َ َما َعلَّ ْم َت َنا إِ َّن َك أنت ال َعلِي ُم ْ م ال َح ِكي ُ dr2003eg@hotmail.com (البقرة)32: INTRODUCTION dr2003eg@hotmail.com Immune thrombocytopenic purpura (ITP) is an acquired disease in which autoantibodies to platelets cause their sequestration and destruction by mononuclear macrophages, principally in the spleen. the number of circulating platelets decreases (thrombocytopenia), resulting in a characteristic bleeding tendency (purpura) . Immune thrombocytopenic purpura (ITP) is traditionally divided in acute and chronic forms based on the duration of the disease. A minority of children with idiopathic or immune thrombocytopenic purpura (ITP) have the refractory chronic form with bleeding problems (stage III or IV). • Characters: • Immune (idiopathic) thrombocytopenic purpura (ITP) is a syndrome characterized by: • 1: Thrombocytopenia (platelet count less than 100 x 109 /L). • 2: Shortened platelet survival.(chromium -51 labeled platelets have a life span of a few minutes to 1-4 hours). • 3: Presence of antiplatelet antibody in the plasma. • 4: Increased megakaryocytes in the bone marrow. Classification: This condition may be acute, chronic or recurrent. 1. Acute form, the platelet count return to normal (>150 x 109/L) within 6 months after diagnosis and relapse does not occur. 2. Chronic form, the platelet count remains low after 6 months. 3. Recurrent form, the platelet count decreases after having returned to normal levels. In adults, the chronic form is more common, whereas in children, the acute form is more common. ●A minority of children with idiopathic or immune thrombocytopenic purpura (ITP) have the refractory chronic form with bleeding problems (stage III or IV). Chronic refractory idiopathic thrombocytopenic purpura (ITP) is defined as ITP with persistent thrombocytopenia despite conventional initial management with Prednisone and splenectomy Pathophysiology • Recent articles have revealed the dominance of a proinflammatory state in ITP following a relatively benign viral or environmental trigger • In addition, several articles have documented the persistence of inflammatory cytokines. and disturbed T cell apoptosis in childhood ITP. every child and adult has the potential to form autoantibodies to platelets. For unclear reasons, these self-reactive antiplatelet clones are not deleted during fetal development and persist in the antibody repertoire of the mature individual Pathogenesis can be summarized in three steps: 1:Platelet Autoantibodies and Antigens: There are two types of mechanisms for the role of auto antibodies in ITP: A: Autoantibodies against Platelets: B: Autoantibodies against Megakaryocytes: 2: Platelets Clearance: 3: Infections Diagnosis of ITP A. clinical Findings Typically, children with acute ITP appear healthy and the physical examination is unremarkable except for Skin Ecchymoses and petechiae Mucous membranes A small number of patients have ‘wet purpura’ with oral blood blisters or mucocutaneous or subconjunctival Bleeding from the nose gums, Mucous membranes, gastrointestinal tract, or kidneys is not uncommon, Menorrhagia may occur and may be severe. Hematemesis and melena are infrequent. Internal organs Bleeding may occur into the following organs: 1. Central nervous system a serious complication 2. Retinal hemorrhage 3. Middle ear: uncommon leading to hear impairment 4. Deep muscle hematoma and hemarthrosis: rare. Signs With exception of hemorrhagic manifestation, the physical examination is not significant Usually, there is neither pallor nor hepatosplenomegaly. A palpable spleen is usually suggestive of a secondary cause (leukaemia, systemic lupus erythematosus, infectious mononucleosis, or hypersplenism) but the splenic tip may be palpable in 5–10% of patients with acute ITP. Cervical lymphadenopathy is not present unless the precipitating factor is viral illness B. Laboratory Findings A complete blood count (CBC) and peripheral blood smear examination remain the most important laboratory tests The CBC should be within normal limits for age (normal hemoglobin levels, red blood cell count indices, and total and differential white blood cell counts) except for the low platelet count and mildly elevated platelet size. A peripheral smear should demonstrate normal morphology of all cell lines with a few large platelets. Tests to consider when a patient does not meet the criteria forchildhood immune thrombocytopenic purpura or has persistent thrombocytopenia ---------------------------------------------------------------------------------Bone marrow aspiration Coagulation profile: prothrombin time, partial thromboplastin time Specific serum antibody assays for glycoprotein IIb/IIIa Viral serology (HIV, EBV, CMV, parvovirus B19, VZV, hepatitis A, B, C, roseola) Antinuclear antibodies, lupus anticoagulant Direct antiglobulin test Thyroid function studies Quantitative serum immunoglobulins with IgG subclasses Reticulated platelet count Platelet function tests ---------------------------------------------------------------------------------- Common laboratory tests obtained in the thrombocytopenic patient at presentation. Complete blood count and differential review Rule out: Multilineage involvement leukemia or aplastic/myelodysplasia smear Evaluate platelet size (giant or "dust-like") Reticulocyte count Hemolytic anemia or chronic blood loss Blood type, Rh, antibody screen Possible anti-D antibody treatment Autoimmune hemolytic disease Chemistry panel Eliminate systemic disease, i.e., hemolytic uremic syndrome, hepatitis, hemolysis, occult malignancy with elevated LDH or uric acid DIC screen Sepsis, Kasabach-Merritt syndrome Quantitative immunoglobulin levels Rule out: common variable immune deficiency, Wiscott-Aldrich Viral titers/PCR Cytomegalovirus, Epstein-Barr virus, human immundeficiency virus Collagen vascular panel (ANA, anti-DNA) Older patients, especially those with more chronic onset History and physical findings not consistent with (ITP) of childhood. History/Findings Alternative Diagnosis Thrombocytopenia present from birth Amegakaryocytosis Primary thrombocytopenia Giant platelet syndromes Weight loss and recurrent fevers Malignancy, immune deficiencies Bloody diarrhea Wiskott Aldrich Hemolytic uremic syndrome Recurrent infections or failure to thrive Primary immune disorder, HIV History or presence of jaundice Autoimmune hemolytic disease Hepatitis, cirrhosis with splenomegaly Splenomegaly,lymphadenopathy Autoimmune lymphoproliferative syndrome (ALPS), primary immune disorders, Gauchers malignancies, hypersplenism syndromes Forearm or hand anomalies Thrombocytopenia absent radii (TAR) Fanconi’s syndrome Malar rash, dermatomyocytis, polymyocytis, eczema Collagen vascular disease, Wiskott Aldrich Cardiac malformation with or without DiGeorge Chromosome 22 microdeletions with large syndrome platelets, with or without Evans syndrome C.Other Laboratory Tests Additional tests should be considered in children with persistent ITP of 3–6 months’ duration or in whom secondary thrombocytopenia is suspected . A-Specific serum antibody assays for glycoprotein IIb/IIIa have a role in distinguishing immune from non-immune thrombocytopenia in adults with ITP; their value in pediatric patients is limited , B- Assessment of platelet maturity by measuring reticulated platelets may be helpful in the diagnosis of ITP in children with atypical presentations. Elevated reticulated platelet counts are indicative of increased production. Differential diagnosis of childhood immune thrombocytopenic Purpura Congenital syndromes Fanconi anemia, thrombocytopenia-absent radii, Wiskott-Aldrich, Alport, and Bernard Soulier syndromes, May-Hegglin anomaly, gray platelet syndrome Decreased platelet production Acute leukemia, lymphoma, aplastic anemia, amegakaryocytic thrombocytopenia, myelodysplastic syndrome, metastatic infiltration Of bone marrow Increased platelet destruction Disseminated intravascular coagulation, thrombotic thrombocytopenic Purpura, hemolytic uremic syndrome, Evans syndrome. • Criteria for the diagnosis : 1. Clinical examination: purpura with an otherwise essentially normal physical examination, with no significant splenomegaly and no lymphadenopathy 2. Platelet count and blood smears: thrombocytopenia only, with no evidence of red cell or white blood cell abnormalities 3. Bone marrow: normal to increased number of megakaryocytes with normal myeloid and erythroid elements 4. Exclusion of secondary causes of thrombocytopenia, such as hypersplenism, microangiopathic hemolytic anaemia, disseminated intravascular coagulation, drug- induced thrombocytopenia, SLE, infections such as EBV, HIV, and parvovirus Prognosis 1. Excellent; 50% recover usually within 1 month and 70-80% recover Within 6 months. 2. Spontaneous remission after 1 year is uncommon, although may occur even after several years. 3. When a demonstrable underlying cause of ITP exists, the prognosis is related to cause. 4. Age older than 10 years, insidious onset, and female gender are associated with the development of chronic ITP. 5. Of all chronic patients, 50-60% eventually stabilize without any therapy and without recourse to splenectomy Khalid @Show • the recently published BSH (the British Committee for Standards in Hematology, 2003) practice guidelines for ITP in children clearly recommend that treatment be considered on the basis of clinical symptoms and cutaneous signs and not just platelet count alone. • The ASH (the American Society of Hematology ) practice guidelines published in 1996 differ from those of the BSH in that the triggers for initiating treatment for children with ITP are based on a low platelet count and the very small but definite risk of ICH, rather than symptoms. (George et al, 1996) and minor purpura do not require treatment or hospitalization. Children with platelet counts of <20 000/uL and significant mucous membrane bleeding, or children with platelet counts of <10 000/uL and minor purpura, should receive treatment with IVIG, IV RhIG, or corticosteroids to increase the platelet count . • Firstly, the severity and bleeding risk of the patient have to be considered. A patient with stage I or II will only be actively treated in special circumstances. In patients with stage III or IV, the aim of treatment is to reach stage II or stage I. Staging of immune thrombocytopenic purpura (ITP) Stage I II Symptoms/platelet count No bleeding; mean platelet Count above 30 x109/L Mild skin bleeding; mean platelet count above 30 x strategy of III IV Moderate skin and/or mucosal bleeding; mean platelet count 10–30 x 109/L Severe bleeding with drop in hemoglobin/hematocrit level; platelet count below 10 x109/L Recommendation No drug intervention Reach individual consensus 109/L parents/patient fo watchful observation Aim: normal lifestyle without drug treatment, appropriate intervention with regard to sport, special events, surgery etc Drug treatment in the presence of active bleeding Aim: reach stage II or stage I Intervention, including drug treatment and eventually substitution of thrombocytes and/or A: Pharmacologic Therapy Comparison of acute (ITP) treatment regimens in children. Treatment Response IV Immunoglobulin (1-2 g/kg) Anti-D Immunoglobulin (75 µg/kg) Response > 20,000 at 60-70% of patients 48 hours 70–80% of patients 77% of patients Common side effects Post-infusion headache, vomiting, allergic reactions, fever, chills Hemolysis, headache Rare but reactions Prednisone (4 mg/k/day 1-7, max 60 mg) Weight gain, irritability, hypertension, stomach pain, hyperglycemia chills, fever, severe Gastic ulcer, reflux, bleeding, hypertensioninduced ICH Anaphylaxis, aseptic Massive hemolysis with meningitis, renal associated back failure Pain myalgia, anemia Duration of initial Wide range of response (days) response after 30 days of weaning from initial dose to 0 21-72 days with 21–48 days based on the75 platelet count greater µg/kg dose than 20,000/mm3 Figure 2. Mechanisms of Action of Therapies for Immune Thrombocytopenic Purpura. 1. Corticosteroids Corticosteroids block the destruction of antibodycoated platelets by the reticuloendothelial system, reduce bleeding by stabilization of capillaries, and decrease the synthesis of antiplatelet antibodies ●Oral prednisone in a dose of 1–4 mg/kg (usually 2 mg/kg/day or 60 mg/m2/day continued until platelet recovery and for 3–4 weeks) has been the gold standard for treating ITP in children for several decades. •For more urgent treatment of acute severe thrombocytopenia (platelet counts of <10 000/UL) with mucosal or other acute bleeding, intravenous methyl prednisolone (30 mg/kg/day for 3 days or 500mg/m 2/day; maximum 1g /day is the drug of choice. Recently, The ASH guidelines endorse the use of : A - Prednisone: 4 mg/kg/day on days 1–7, 2 mg/kg/day on days 8–12, 1 mg/kg/day on days 13–17, tapered on days 18–20 with discontinuation at day 21 or prednisone 4 mg/kg/day for 4 days B - Dexamethasone: 20 mg/m2/day for 4 days every 28 days for six courses, but it appears to be effective and well tolerated if given in newly diagnosed patients daily for 4 days as a single treatment. Most pediatricians in the UK prefer to use corticosteroids as first-line treatment for ITP in children. The BSH guidelines endorse the use of high-dose prednisolone 4 mg/kg/day as a very short course (4 days) or low- dose prednisolone (1–2 mg/kg/day) for no more than 14 days, regardless of response, for children with mucous membrane and significant cutaneous bleeding. • Continuing prednisone treatment beyond 2–3 weeks (even at minimal doses), or titrating it against the platelet count is not recommended as it is likely to induce additional adverse effects of hypercortisolism, including facial swelling (moon facies), weight gain, growth retardation, cataracts, osteopenia, hypertension, and increased susceptibility to infections. For these reasons, prednisone is recommended for acute, short-term (induction) treatment of ITP in children, but long-term (maintenance) treatment is strongly discouraged, particularly since less toxic alternative treatments are now available. 2. Intravenous Immunoglobulin Mechanisms of action of high-dose IVGG include: A. Reticuloendothelial Fc-receptor blockade. B. Activation of inhibitory pathways. C. Decrease in autoantibody synthesis. Indications of IVGG in acute ITP A. Neonatal symptomatic immune thrombocytopenia and infants less than 2 years of age who are generally more refractory to steroid treatment B. Alternative therapy to corticosteroid therapy but is much more expensive, has significant side effect, is not significantly clinically better than steroid therapy to justify expense and side effect of its use. Dosage A. Acute ITP: a total dose of 2g/kg body weight given as follow: (1)0.4g/kg IVGG per day for 5days OR (2)1g/kg per day for 2 days. Lower doses of 800mg/kg/day as a single dose or 250 mg/kg/day for 2 days have been used with success, and fewer side effects are seen, in younger children. B. chronic ITP: (1) Initial IVGG dose of 1g/kg body weight daily for 2 days, followed by periodic single infusions (0.4-1g/kg depending on response) to maintain platelet count at a safe level (<20,000/mm2) (2) alternate-day corticosteroids is useful adjunctive therapy when IVGG is used 3. Intravenous Anti-D Rhesus (Rh) 0 Immunoglobulin • Compared with IVIG, IV RhIG has the advantages of ease of administration and lower treatmentrelated costs . • increasing the dose of IV RhIG from the standard 50 µg/kg to an off-label dose of 75 µg/kg, administered as an infusion, may increase efficacy without increasing adverse effects. • The principal disadvantages of IV RhIG are its lack of efficacy for Rh (D)-negative patients and for patients who have undergone a splenectomy. The principal adverse effect of IV RhIG is anemia due to anti-D-mediated immune hemolysis. • Rarely, patients have experienced acute hemoglobinemia, hemoglobinuria, or acute renal failure after an infusion of IV RhIG. To avoid the possibility of symptomatic anemia associated with excessive hemolysis, IV RhIG should not be infused in a patient whose hemoglobin is <10 g/dL. • B: Surgical Interventions ●Splenectomy • Splenectomy was the only reliable treatment for ITP. Response rates as high as 92% following splenectomy have been reported in surgical journals • However, these optimistic assessments were based on relatively short-term, post-surgical follow-up and a general lack of understanding of the importance of the spleen in limiting bacterial infections. A current assessment of the relatively few reports of long-term, follow-up of children who have had splenectomies for ITP revealed remission rates of 70–80% . Short-term morbidity and mortality associated with splenectomy have been reduced by the use of less invasive laparoscopic techniques. Post-splenectomy mortality due to bacterial sepsis, which carried a fatality rate as high as 15 %,has been dramatically reduced by immunizing children against encapsulated organisms prior to splenectomy followed by prophylactic penicillin for at least 1 year after splenectomy. However, a splenectomy is rarely indicated today in children with ITP as spontaneous remissions continue to occur up to at least 15 years from diagnosis, Several relatively new effective non surgical treatments are available, and all patients following splenectomy continue to have a small, but life-long, potentially fatal risk of bacterial sepsis. However, splenectomy should be considered in children with chronic, persistent, and severe ITP that has been present for more than 12–24 months and is having a significant impact on their quality of life . All children scheduled for a splenectomy require a review of their immunization status. At least 2 weeks prior to undergoing asplenectomy, children aged ≥ 2years should be immunized with 23-valent pneumococcal polysaccharide vaccine. Haemophilus influenzae type b vaccine and heptavalent pneumococcal conjugate vaccine should also be provided depending on the patient’s age and immunization history. The meningococcal vaccine is also used for children aged ≥ 2 years. Daily penicillin prophylaxis is recommended for children aged ≤ 5 years and should be continued for at least 1 year after a splenectomy. Treatment of children with life threatening hemorrhage: 1: platelet transfusion 2: methylprednisolone 500mg/m2 IV per day for 3day 3: IVGG 2g/kg 4: emergency splenectomy. These measures can be used singly or in combination, depending on severity and response to treatment. Management of Children with Refractory ITP: 1 .Vinca Alkaloids • An IV dosage of vincristine 1.5 mg/m2, maximum 2mg, or vinblastine 0.1 mg/kg bodyweight is given every 7 days for 4–6 weeks. 2. Azathioprine • Azathioprine is given in a dosage of 1–4 mg/kg bodyweight per day orally. • Azathioprine should be given for at least 4 months, but no longer than 12 months. 3. Cyclophosphamide • Cyclophosphamide is effective in 30–40% of patients and is given orally at 1–2 mg/kg bodyweight per day. If a response occurs within 2 months, the treatment should be continued for a total of 3 months and then stopped. 4. Cyclic High-Dose Methylprednisolone • Cyclic high-dose methylprednisolone (IV 20– 30 mg/kg bodyweight) or dexamethasone (oral 1 mg/kg bodyweight) can be given on 3– 4 consecutive days every 4 weeks for 4 months. 5. Splenectomy 6. Plasmapheresis Immunoadsorption or Protein A • Plasmapheresis or protein A immunoadsorption transiently reduces (auto) antibodies and platelet activation. • The response rate is low and the costs are high. In children, this procedure is indicated in those with high platelet-associated antibody levels and severe bleeding. Possible Future Treatment Options for Refractory ITP 1-Treatment influencing antigenemia: Platelet counts were improved after antibacterial eradication of Helicobacter pylori 2-Treatment response: influencing the T-cell immune A-Cyclosporine. B-CTLA-4-Ig 3-Treatment influencing the B-cell immune response: A- anti-CD20monoclonal antibody (rituximab): Within three to four courses of rituximab (IV 375 mg/m2/week X four weeks), approximately two-thirds of patients had an increase in platelet count and some had longlasting responses (>6 months). B-Anti-CD52 Monoclonal Antibody (Alemtuzumab C- interferon- 4-Other options: A- thrombopoietin. B-autologous hematologic stem celltransplantation Future Therapies for ITP A-Thrombopoietin (TPO) Agents AMG 531 and eltrombopag are the second-generation TPO receptor agonists that share no sequence homology with native TPO. B-Specific Inhibitors of PhagocyteMediated Consumption of Platelets A humanized antibody, GMA-161, has been developed and used in 2 low-dose cohorts of 8 adults with chronic, refractory ITP. Mervat hesham