Case Presentation - asja
advertisement

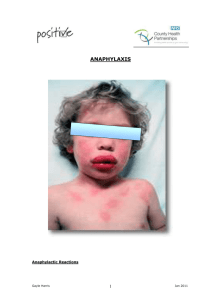
Case Presentation By Dr Ahmaed Nabil Assistant Lecturer Of Anesthesia Ain Shams University Case : A 23-years-old man is scheduled to undergo an ORIF of a carpal scaphoid fracture, using a bone graft to be harvested from the iliac crest. Induction of general anesthesia and intubation were uneventful. When cefazolin 1 g is administered intravenously a rash appears over the face and chest. The heart rate is 135 beats per minute and the blood pressure drops to 70/40 mmHg Questions What is the mechanism of anaphylaxis? What is the difference between anaphylactic and anaphylactoid reactions? What treatment should be administered to this patient? What else should be checked on physical examination? What are the medications most often implicated in anaphylaxis? In anaphylactoid reactions? Questions What is the percentage of patients allergic to penicillin who will have a reaction when challenged with a cephalosporin? What antibiotic would you use for “clean” orthopedic surgery in a patient reporting a penicillin allergy or a reaction to cephalosporins? What is the mechanism of anaphylaxis? Anaphylaxis is an IgE-mediated allergic reaction. The most common mechanism for an anaphylactic reaction is the degranulation of mast cells and basophils with the subsequent release of inflammatory mediators, which are responsible for the symptoms and signs. What is the difference between anaphylactic and anaphylactoid reactions? Anaphylactoid reactions are clinically indistinguishable from anaphylaxis. However, the mechanism of action differs in that IgE is not involved. Anaphylactoid reactions are a result of direct degranulation of mast cells and basophils with release of the same mediators as in anaphylactic reactions Anaphylactoid reaction In practice, it does not matter whether or not the reaction is IgE or non-IgE mediated. The immediate management of the patient is the same the patient will need to avoid the drug in the future, irrespective of the mechanism of the reaction What else should be physical examination? checked on 1st we have to know that true anaphylaxis during anesthesia is very rare. Many anesthetists may never see such a reaction and few will see more than one during their working life. However, because the consequences of anaphylaxis can be serious and potentially lifethreatening, it is important for anaesthetists to know what the clinical signs are and how to deal with them. Physical Examination The reported incidence of anaphylactic reactions during general anaesthesia varies considerably between 1 in 950 to 1 in 20,000 anaesthetic procedures. Physical Examination Clinically, a mild reaction is manifested as: flushing urticaria redness localized edema. Physical Examination While a severe reaction is manifested by: shock (severe hypotension) bronchospasm widespread edema massive intravascular fluid loss resulting in dramatically reduced filling of the heart and subsequent severe hypotension What treatment should be administered to this patient? Causes need to be excluded first; Exaggerated hypotensive response to the induction agent Bronchospasm resulting from the mechanical effects of endotracheal intubation in susceptible patients Vagal response causing severe bradycardia (e.g. During laparoscopy , ophthalmic procedures, etc); Other causes; Covert hemorrhage. Unexpectedly extensive sympathetic blockade during epidural or intrathecal neuraxial anesthesia; Acute exacerbation of pre-existent asthma independent of an aesthesia; For treatment: 1.Call for help and inform the surgical team 2.Stop administration of the drug(s) likely to have caused the reaction. It is recommended to stop all the drugs that are possible to stop, as at this time the causative agent can not be determined. 3.(ABC) , Maintain airway: give 100% oxygen. 4.Lie patient flat with feet raised Epinephrine Is the drug of choice when resuscitating patients during anaphylactic shock Epinephrine Epinephrine acts by two mechanisms: It reverses vasodilatation by its α-agonist effects It blocks further degranulation of mast cells or basophiles through its β-agonist effects. It may also improve cerebral perfusion independent of its effect on blood pressure by β2-mediated vasodilatation, and it is very effective in the treatment of bronchospasm. For treatment (cont’d); 5.Give adrenaline (epinephrine): 50–100 μg (0.5–1 mL of a 1:10,000 solution found in pre-filled syringes, or 0.05–0.1 mL of the more commonly used 1:1,000 solution), or 0.01 mg/kg in children. Should be administered subcutaneously if the patient is merely hypotensive, and may be repeated as needed. Higher doses and the intravenous route should be used if the reaction is severe, or if cardiac arrest supervenes. For treatment (cont’d); The European guidelines say that Intravenous administration should be done instead of the subcutaneous route ; Titrated doses (10-20mic for moderate cases and 100-200 mic for severe cases) are given To be repeated every one to two minutes until restoration of arterial blood pressure. For treatment (cont’d); I.V infusion at a dose of 0.05 to 0.1 mic /kg might be used instead of repeated bolus administration of epinephrine. If I.V route is not immediately availbale, the I.M route can be used(0.3-0.5 mg) with injection to be repeated every 5-10 minutes depending on the patient hemodynamic status. In the same situation, the intra tracheal route can be used if the trachea is intubated knowing that one third of the dose will enter the circulation For treatment (cont’d); High doses of epinephrine are more efficacious but cases of myocardial ischemia or even infarction after epinephrine administration have been reported. Other measures include Start rapid i.v volume expansion with crystalloid or colloid. Increased vascular permeability can transfer 50% of intravascular fluid into the extravascular space within 10 minutes. The amount of fluid administered should be based on hemodynamic parameter Other measures include Intravenous steroids (e.g., methylprednisolone 1–2 mg/kg intravenously or hydro cortisone 100-500mg (I.V); repeat q4–6 hourly as needed). Steroids may have no effect for 4–6 hours, but may prevent persistent or biphasic anaphylaxis. Other measures include Anti-H1 medications (e.g., diphenhydramine 25– 100 mg IV). Anti-H2 medications (e.g., ranitidine 1 mg/kg IV). Glucagon (1–5 mg IV) in severe reactions. Glucagon directly activates adenyl cyclase and bypasses the β-adrenergic receptor. It may reverse refractory hypotension and bronchospasm. Glucagon or atropine should be used in β-blocked patients to increase an inappropriately slow heart rate. Other measures include In case of refractory hypotension, military antishock trousers (MAST) may significantly improve hemodynamics. Other measures include Save any blood samples that have been collected prior to or during the procedure. These may be required for testing. Other measures include If cardiac arrest supervenes, advanced cardiac life support (ACLS) protocols should be followed, including epinephrine, atropine, etc. Prolonged resuscitative efforts are encouraged, since recovery is more likely to be successful in anaphylaxis, in which the subject is often a young individual with a healthy cardiovascular system Further management The chest should be auscultated since bronchospasm is often triggered by anaphylactic or anaphylactoid reactions. If bronchospasm does not respond to the treatment administered for anaphylaxis, inhaled β2-agonists and possibly aminophylline should be added to the regimen. Volatile anesthetics can also be used (if that is not already the case, and if the blood pressure allows) for their bronchodilating properties. Note If pregnant; start with ephedrine(10 mg to be repeated every 1-2 minutes)because of the risk of hypoperfusion of the placenta caused by epinephrine and the patient should be placed in the left lateral decubitus. In case of ineffectiveness, switch to epinephrine To summarize: Immediate measures a. Assess airway, breathing, circulation b. Administer epinephrine SQ 50–100 μg or 0.01 mg/kg in children; repeat as needed(or iv/im) General measures a. Expedite surgery; position the patient supine; elevate lower extremities b. Administer 100% oxygen c. Administer normal saline or colloids if there is severe hypotension To summarize: Specific measures a. Glucocorticoids: methylprednisolone 1–2 mg/kg IV; repeat q 4–6 hourly as needed b. H1 antagonists: diphenhydramine 25–100 mg IV c. H2 antagonists: ranitidine 1 mg/kg IV d. Glucagon: 1–5 mg IV e. Nebulized β2-agonists f. Aminophylline: 5 mg/kg IV over 30 min, then 0.9 mg/kg/hr IV; follow serum levels (therapeutic range 8– 15 μg/mL) g. Military antishock trousers (MAST) To summarize: Supervening cardiac arrest, in addition to ACLS protocol a. Rapid volume expansion b. Prolonged resuscitative efforts What are the medications most often implicated in anaphylaxis? In anaphylactoid reactions? The commonly anaphylaxis are: Antibiotics Aprotinin IV anaesthetics, e.g. thiopental, propofol, midazolam Latex rubber Local anaesthetics Neuromuscular blocking agents (NMBAs) Non-opioid analgesics, e.g. NSAIDs Opioid analgesics, e.g. morphine, alfentanyl, fentany used drugs during Others Plasma volume expanders, e.g. gelatins, starches Pre-medication drugs Preservatives Protamine Radiocontrast media Skin antiseptics, e.g. chlorhexidine, iodine Others The rate of anaphylactic reactions with iodinated contrast has significantly decreased because sensitive individuals are being pretreated with steroids and antihistamines, and non-ionic contrast with less potential to cause allergic reactions is being used. Latex has emerged as a cause of anaphylactic reaction , probably because of the increasing use of latex gloves and barriers. Patients who have undergone multiple surgeries, and healthcare workers are especially at risk Others Anaphylactoid reactions are commonly caused by morphine, d-tubocurarine, certain antibiotics (e.g., vancomycin, ciprofloxacin), aspirin (possibly through inhibition of cyclooxygenase), and succinylcholine What is the percentage of patients allergic to penicillin who will have a reaction when challenged with a cephalosporin? In patients with true allergy to penicillin, a 3–7% rate of allergic reaction to cephalosporin is expected, versus 1–2% in patients with no history of penicillin allergy. History is the most important element here. What is the percentage of patients allergic to penicillin who will have a reaction when challenged with a cephalosporin? A morbilliform rash (i.e., resembling measles), consisting of macular lesions that are red and are usually 2–10 mm in diameter but may be confluent in places, is a benign reaction that does not qualify as “allergic”. In a patient who had a morbilliform rash, cephalosporins can be given safely. What antibiotic would you use for “clean” orthopedic surgery in a patient reporting a penicillin allergy or a reaction to cephalosporins? If true allergy to penicillin or cephalosporins is reported, it is prudent to use clindamycin 600 mg intravenously. Vancomycin 1,000 mg intravenously administered over 30–60 minutes can be used as well. Rapid vancomycin administration may cause the “red man syndrome” secondary to a non-immune-mediated release of histamine, i.e.an anaphylactoid reaction. Case (cont’d) Once blood pressure and heart rate returned to normal, the rash was subsiding and the chest auscultation was clear. Should surgery be allowed to proceed or should the case be cancelled? What will you tell the patient postoperatively? Answer The case can probably be allowed to proceed after rapid resolution of the event. Upper airway edema should be excluded prior to extubation. The presence of a leak around the endotracheal tube should be determined by deflating the endotracheal tube cuff and occluding the tube manually. Postoperative Recommendations This patient should be told that the administration of any β-lactam antibiotic might be fatal. He should be given a letter detailing the reaction and specifically naming the medication involved, and he should be instructed to wear a bracelet indicating his allergy. Allergy specialists sometimes perform skin tests to identify the causative drug Who are at risk for anaphylaxis during anesthesia? Patients who are allergic to one of the drugs or products likely to be administered or used during anaesthesia and for which the diagnosis had been established by a previous allergy investigation(e.g Deprivan and eggs). Patients who have shown clinical signs suggesting an allergic reaction during a previous anaesthesia. Patients who have experienced clinical manifestations of allergy when exposed to latex Other patients Children who have had multiple operations, especially those with spina bifida, because of the high rate of sensitization to latex Patients who have experienced clinical manifestations of allergy to kiwi, banana, chestnut,buckwheat, etc., because of the high rate of cross-reactivity with latex. Others Patients who are atopic (for example, those with allergic asthma or hay fever) or those who are allergic to a drug or other product that is not likely to be used during the course of the anesthesia are not to be considered at risk for anaphylaxis during anesthesia Note For those patients who are at risk as defined above , an allergy investigation looking for specific sensitization should be proposed before any anesthetic procedure. Nevertheless, no matter which tests are used, they do not guarantee an absolutely correct diagnosis. 1ry prevention Total avoidance of contact with latex from the first surgical procedure and in the medical environment of infants with spina bifida prevents the acquisition of latex sensitivity . There is actually no way to prevent primary sensitization to muscle relaxants. Anaphylactic reactions to these agents can occur in the absence of their prior administration 2ry prevention The only effective secondary preventive measure is to IDENTIFY THE RESPONSIBLE ALLERGEN and then completely avoid it. For patients sensitized to latex, a latexfree environment is effective for the prevention of an anaphylactic reaction. The latex-free environment must include the operating rooms, the postoperative recovery room and some other sectors of the hospital Note The intravenous administration of antibiotics for preoperative prophylaxis should be started in the operating room with the patient awake and being monitored, 5 to 10 minutes before anesthesia induction. Because there is no evidence of crossreactivity between propofol and muscle relaxants, the use of propofol in patients allergic to a muscle relaxant is not contraindicated.