Osa power point
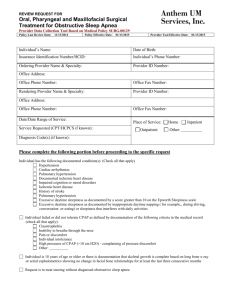
advertisement

By Lucy suliman Sleep related breathing disorders defintions Apnea: Apnea is the cessation, or near cessation, of airflow for 10 seconds. Oronasal thermal sensor (or alternative) drops by ≥90% of baseline. Duration ≥ 10 sec. At least 90% of events duration must meet apnea amplitude reduction criteria . Obstructive apnea An obstructive apnea occurs when airflow is absent or nearly absent, but ventilatory effort persists. It is caused by complete, or near complete, upper airway obstruction. Central apnea A central apnea occurs when both airflow and ventilatory effort are absent Breathing cessation is proven by an absence of diaphragmatic activation, measured by electromyography (EMG). Mixed apnea During a mixed apnea, there is an interval during which there is no respiratory effort (ie, central apnea pattern) and an interval during which there are obstructed respiratory efforts .The central apnea pattern usually precedes the obstructive apnea pattern during mixed apnea Hypopnea Hypopnea is a reduction of airflow to a degree that is insufficient to meet the criteria for an apnea. The most recent definition, endorsed by the American Academy of Sleep Medicine, recommends that hypopnea be scored when all of the following four criteria are met: Airflow decreases at least 30 percent from baseline There is diminished airflow lasting at least 10 seconds at least 4 percent oxyhemoglobin desaturation Associated with arousal or Airflow decreases at least 50 percent from baseline There is diminished airflow lasting at least 10 seconds 3 percent oxyhemoglobin desaturation or an arousal Respiratory effort related arousals — Respiratory effort related arousals (RERAs) exist when there is a sequence of breaths that lasts at least 10 seconds, is characterized by increasing respiratory effort or flattening of the nasal pressure waveform leads to an arousal from sleep does not meet the criteria of an apnea or hypopnea Hypoventilation Hypoventilation during sleep is defined as an increase in the arterial carbon dioxide (PaCO2) of 10 mm Hg during sleep (compared with an awake supine value) that lasts at least 25 percent of the sleep time. Directly measuring the pCO2 in an arterial blood gas during a sleep study is optimal, but impractical. Transcutaneous CO2 measurements and expired end tidal CO2 are alternatives . Polysomnography indices Apnea index The apnea index (AI) is the total number of apneas per hour of sleep Apnea-hypopnea index — The apnea– hypopnea index (AHI) is the total number of apneas and hypopneas per hour of sleep. The AHI is most commonly calculated per hour of total sleep. Respiratory disturbance index The respiratory disturbance index (RDI) is the total number of events (eg, apneas, hypopneas, and RERAs) per hour of sleep. Desaturation — Oxygen desaturation is a frequent consequence of apnea and hypopnea. Several measures are used to quantify the severity of desaturation and should be included in polysomnography report . Oxygen desaturation index (ODI) This is the number of times that the oxygen saturation falls by more than 3 or 4 percent per hour of sleep Minimum levels Arousal index The arousal index (ArI) is the total number of arousals per hour of sleep. It is generally lower than the AHI or RDI because approximately 20 percent of apneas or hypopneas are not accompanied by arousals syndromes of sleep related breathing disorders Obstructive sleep apnea syndrome Obstructive sleep apnea syndrome encompasses obstructive sleep apnea (OSA) in adults and OSA in children. OSA in adults is defined as either : More than 15 apneas, hypopneas, or RERAs per hour of sleep (ie, an AHI or RDI >15 events/hr) in an asymptomatic patient OR More than 5 apneas, hypopneas, or RERAs per hour of sleep (ie, an AHI or RDI >5 events per hour) in a patient with symptoms (eg, sleepiness, fatigue and inattention) or signs of disturbed sleep (eg, snoring, restless sleep, and respiratory pauses). Central sleep apnea syndrome Central sleep apnea syndrome (CSAS) can be: idiopathic (eg, primary central sleep apnea [CSA]) secondary. Examples of secondary CSAS include Cheyne-Stokes breathing, CSA due to high altitude periodic breathing, CSA due to a medical condition, and CSA due to a drug or substance. More than 75 percent of events should be central to qualify for this syndrome category. Complex Sleep Apnea (CompSA) CompSA consists of all or predominantly obstructive apneas which convert to all or predominantly central apneas when treated with a CPAP or bilevel devices Cheyne-Stokes breathing — Cheyne-Stokes breathing refers to a cyclic pattern of crescendodecrescendo tidal volumes and central apneas, hypopneas, or both. It is commonly associated with heart failure or stroke. Hypoventilation syndromes — Patients with a hypoventilation syndrome generally have mild hypercarbia or elevated serum bicarbonate levels when awake, which worsen during sleep. Two hypoventilation syndromes: congenital central hypoventilation syndrome (CCHS) obesity hypoventilation syndrome (OHS), Cheyne-Stokes breathing Obstructive sleep apnea :(OSA) is a disorder that is characterized by obstructive apneas and hypopneas caused by repetitive collapse of the upper airway during sleep. The diagnosis should be considered whenever a patient presents with risk factors or clinical manifestations that are compatible with OSA. RISK FACTORS : obesity. craniofacial abnormalities. upper airway soft tissue abnormalities. Potential risk factors include: heredity,smoking, nasal congestion, and diabetes . EPIDEMIOLOGY 26 percent of adults are at high risk for OSA . 20 percent if defined as an apnea hypopnea index greater than five events per hour . 2 to 9 percent is defined as an AHI greater than five events per hour accompanied by at least one symptom that is known to respond to treatment Age :The prevalence of OSA increases from 18 to 45 years of age. There is a two- to three-fold higher prevalence among individuals who are 65 years and older, compared to those who are 30 to 64 years old. Grades of OSA Mild :AHI between 5 and 15 events per hour Moderate:an AHI between 15 and 30 events per hour Severe:AHI greater than 30 events per hour, as well as an oxyhemoglobin saturation below 90 percent for more than 20 percent of the total sleep time Diagnosis of OSA History Physical examinations laboratory Subjective questionnaire:Berline questionnair Epworth Sleepness scale Polysomnography. Mallampati airway cassification modified Mallampati Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep 2006 Laboratory 1)protinuria — Less than 10 percent of patients with OSA have proteinuria 2) Hypercapnia — Although uncommon in OSA alone, awake hypercapnia (and hypoxemia) may be present if obesity hypoventilation syndrome coexists 3)Hypothyroidism — OSA can be caused or exacerbated by hypothyroidism Imaging Studies lateral cephalometry, endoscopy, fluoroscopy, CT scanning, MRI. Epworth sleepiness scale: The chance to doze off or fall asleep in the following situation: 1-sitting and reading 2- watching TV 3- sitting inactive in public place 4-as a passenger in a car for an hour without a break 5-lying down to rest in the afternoon when circumstances permit 6-sitting and talking to someone 7- sitting quietly after a lunch without alcohol. 8- in a car while stopped for few minutes in traffic Berline questionnaire Cardiovascular effects of obstructive sleep apnea SYSTEMIC HYPERTENSION PULMONARY HYPERTENSION CORONARY ARTERY DISEASE CARDIAC ARRHYTHMIAS Cerebral stroke. polysomnographic finding of OSA EEG FINDINGS Increased stage N1 Reduced stage N3 Reduced stage R (REM sleep) Increased respiratory arousals RESPIRATORY FINDINGS Snoring Obstructive, mixed apneas, and central apneas Obstructive hypopneas AHI: mild 5 to <15/hr, moderate 15–30/hr, severe > 30/hr AHI supine > 2 × AHI nonsupine – postural OSA AHI REM > AHI NREM common Apnea duration REM > NREM ARTERIAL OXYGEN DESATURATION Lowest SaO2 during REM sleep Longest REM periods in the early morning hours typically have the worst desaturation CYCLIC VARIATION IN HEART RATE Slowing of heart rate at apnea onset and speeding at event termination. diagnostic criteria of OSA 1) an obstructive respiratory disturbance index (RDI) greater than 15 events per hour. 2) an obstructive RDI between 5 and 14 events per hour that is accompanied by daytime sleepiness, loud snoring, witnessed breathing interruptions, or awakenings due to gasping or choking. Academy of Sleep Medicine: The AASM Manual for Scoring of Sleep and Associated Events: American Academy of Sleep Medicine, 2007. Types of Polysomnography Full-night, attended, in-laboratory polysomnography (PSG) is considered the goldstandard diagnostic test for OSA. It involves monitoring the patient during a full night's sleep Patients who are diagnosed with OSA and choose positive airway pressure therapy are subsequently brought back for another study, during which their positive airway pressure device is titrated Split-night attended, in-laboratory polysomnography is similar, except the diagnostic portion of the study is performed during the first part of the night only. Those patients who are diagnosed with OSA during the first part of the night and choose positive airway pressure therapy can have their positive airway pressure device titrated during the second part of the night Portable monitoring There are a variety of devices that are used for in-home, unattended, portable monitoring. M Indications for treatment 1. 2. 3. respiratory disturbance index (RDI) greater than 15 events per hour an obstructive RDI between 5 and 14 events per hour that is accompanied by daytime sleepiness, loud snoring, witnessed breathing interruptions, or awakenings due to gasping or choking. The AHI is greater than five events per hour and the patient performs mission critical work (eg, airline pilot, bus driver) 4.The frequency of respiratory effort related arousals (RERAs) is abnormal in a patient with subjective or objective daytime sleepiness, even if the AHI is five events per hour or less 5.The AHI is greater than five events per hour and the patient has excessive daytime sleepiness alone that has been objectively measured and confirmed by an abnormal multiple sleep latency test, maintenance of wakefulness test Choosing a therapy The American Academy of Sleep Medicine recommends offering positive airway pressure therapy to all patients who have OSA The choice of an OSA-specific therapy:- positive airway pressure, an oral appliance, upper airway surgery. Medical treatment. depends on the severity of the OSA . severe OSA (AHI >30 events per hour and/or severe clinical sequelae we use positive airway pressure as first-line therapy. This is based on the variable efficacy of oral appliances in this patient population. For patients with mild or moderate OSA (AHI ≤ 30 events per hour with severe clinical sequelae we prefer positive airway pressure to an oral appliance because it is superior at reducing the frequency of obstructive events. In contrast, for patients with mild or moderate OSA without severe clinical sequelae we initiate an oral appliance rather than positive airway pressure. This is based on our recognition that most patients prefer an oral appliance and both modalities have a similar effect on symptoms surgical therapy when positive airway pressure or an oral appliance is declined, ineffective (after at least a three month trial of therapy), or not an option For patients whose OSA is due to a surgically correctable obstructing lesion, surgical resection of the obstructing lesion is first-line therapy BEHAVIOR MODIFICATION Weight loss Sleep position Alcohol avoidance Medication avoidance