Stopping Smoking Before Surgery : Advantages and Issues
advertisement

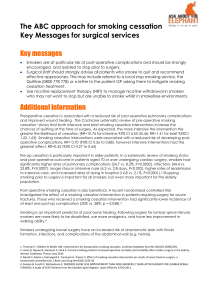
Stopping Smoking Before Surgery: Advantages and Issues Dr. John Oyston Assistant Professor University of Toronto Department of Anesthesia 3rd Ottawa Model Conference February 4th 2011 How Important is Smoking? • It is the #1 cause of preventable death • It consumes 15% of health care budget • It is more important than Breast Cancer More women die of lung cancer due to smoking than from breast cancer. Why do anesthesiologists across Canada care about smoking? • We provide anesthesia for patients who would not have needed surgery if they had never smoked Anesthesiologists – Obvious examples see the problems • Peripheral and cardiac vascular disease caused by smoking every day • Lung and ENT cancers – Less obvious • Bladder tumours (3 x risk: Smoking causes 50%) • Cataracts (20% due to smoking, 50,000 per year) • Fractures (84% increase hip fractures in smokers) Chronic smokers have chronic health problems: CAD COPD Arteriosclerosis Smokers do less well in the operating suite ST Depression v CO level Anesthesia and Analgesia 1999; 89 856 HJ Woehlck et al Smokers do less well postoperatively Short Term - Worse wound healing (Mastectomy flap necrosis 18.9% v 9.0 in NS) (DW Chang Plastic & Long Term - Worse outcome (more pain, poorer function) one year after ACL repair (Karim, Reconstr Surg. 2000 p2374) JBJS, 2006) - More infections (12% in smokers, v 2% NS) (Sorensen, Ann Surg, 2003) “We found that smoking was the single most important risk factor for the development of postoperative complications” (Moller JBJS 2002) … and smokers are more likely to come back for repeat surgery • Failure of original operation Spinal fusion: Non-union twice as common in smokers (Glassman Spine 2000) • Postoperative complications Abdominal wall necrosis (Smokers 7.9% Ex-smokers 4.3% NS 1.0 %). (Padubidri Plastic & Recon Surgery: 2001: p342) • Progression of underlying disease Fem-pop graft -> Revision/Endarterectomy >Sympathectomy ->Toe amputation ->BKA -> AKA Smokers are a pain in the butt for anesthesiologists. Can we do anything about that? 120 patients for elective joint replacement Randomised to control or smoking cessation intervention: Control Routine preoperative preparation 4 stopped smoking anyway Intervention Routine preoperative preparation plus weekly meetings with nurse, NRT therapy 36 stopped smoking, 14 reduced, 6 continued Results Control Wound problems: 31% CV Insufficiency 10% Avg. days in hospital Total days in ICU 13 32 Intervention 5% 0% 11 2 Stopping smoking reduces risk: When to stop? • Ideally 6 – 8 weeks or longer • Definite advantage of 4 weeks • For carbon monoxide elimination, 4 -8 hours – “No smoking after midnight”? – Risk of stopping shortly before surgery? • Postoperative quitting aids wound healing How and when to educate patients about preoperative smoking cessation: • In community, healthy • With a surgical condition, in GPs office • In surgeon’s office My recommendation: • At least one preoperative smoking cessation counselling session should be mandatory before elective surgery . • Surgery should be scheduled no sooner than six weeks after attending that session. How and when to educate patients about preoperative smoking cessation: • • • • In community, healthy With a surgical condition, in GPs office In surgeon’s office During preadmission process – Phone/MD/Pharmacy • In hospital • Post-surgical follow-up • Back in community Three quick issues: Should anesthesiologists prescribe anti-smoking drugs (e.g. Bupropion, Varenicline)? In my clinical setting, where: – I see patients only once – I rely on their self-reported medical and psychiatric history – It is difficult for patients or their families to get back in touch with me – There is no out-of-hours coverage I do not feel it is appropriate to prescribe medications which have significant risks. Some colleagues in academic teaching centres disagree. Does nicotine impair bone healing? • Yes, in experimental models – Vasoconstriction – Parasympathetic system – Effect on stem cells • Is this a reason to avoid NRT in Ortho patients? – Probably not – Some studies showing benefit of quitting used NRT Is it worth quitting before minor surgery? • There is no evidence that quitting before minor surgery improves outcome • BUT … if patients quit when they have an arthroscopy or D & C, when they need a joint replacement or hysterectomy, they will have been smoke free for weeks or months! Can we use surgery as a tool to promote smoking cessation? • • It’s a reason to quit at a specific date Suddenly convert from being healthy to being a patient • It’s a way to regain an element of control in a stressful situation • Less withdrawal symptoms • Surgery forces interaction with a variety of health care workers Does surgery make smokers quit? (Crouse & Hagaman, Am J Epidemiology, 991 p 699) Percentage quit smoking 1 year later Non-cardiac surgery Angiography Angioplasty CABPG 13% 14% 25% 55% How important is surgery as a reason to quit? • 8% of all quitting is related to surgery • 100,000 patients/yr in US quit due to surgery (Yu Shi, Anesthesiology, 2010) But 42% of pts said they were not informed about the effects of preop smoking and 43% of anesthesiologists don’t routinely advise smokers to quit. • There are specific health and economic benefits to perioperative smoking cessation • 1.3 m operations are performed in Canada every year (~ 250,000 on smokers) • We are not leveraging this opportunity to get smokers to quit • We need a national strategy! • An independent not-for-profit organization • Evidence-based, focussed on patient safety and organizational excellence • 600 surveyors ensure proper policies in place in 1000 health service organizations across Canada and world wide • Now becoming interested in smoking policies! Anesthesiology 2006, 104;356-67 www.stopsmokingforsafersurgery.ca john7@oyston.com ADDITIONAL SLIDES





![[Section 2.0] PICO Question Table – LC III Guidelines](http://s3.studylib.net/store/data/006838942_1-d31e4d679d8742f590f21898872c27c9-300x300.png)
