AKI
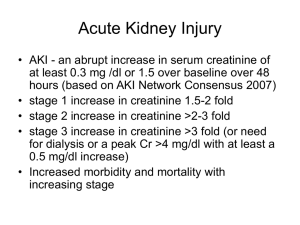
advertisement

Dr. M. A. Al-Odat Jordanian board of medicine S.R. of ICU KSMC Definition There is NO sharp definition of AKI. Traditionally defined as: Abrupt loss of kidney function that results in the retention of urea and other nitrogenous waste products, and dysregulation of extracellular volume and electrolytes. AKI-RIFLE Criteria GFR Criteria Increased creatinine x1.5 or GFR decrease > 25% Risk Injury Failure Urine Output Criteria UO < .5ml/kg/h x 6 hr Increased creatinine x2 or GFR decrease > 50% UO < .5ml/kg/h x 12 hr Increase creatinine x3 or GFR decrease > 75% UO < .3ml/kg/h x 24 hr or Anuria x 12 hrs Loss ESKD Persistent ARF** = complete loss of kidney function > 4 weeks End Stage Kidney Disease (> 3 months) High Sensitivity High Specificity Limitations The change in serum creatinine during acute renal failure does not directly correlate with the actual change in glomerular filtration rate, which alters the assignment of that patient to a particular RIFLE level. Given these limitations, a modification of the RIFLE criteria has been proposed by the Acute Kidney Injury Network. RIFLE and AKIN staging criteria for AKI ______________________________________________________________ RIFLE AKIN Serum Cr Urine Output Stage Stage Criteria Criteria ______________________________________________________________ Risk 1 Increase in Scr of 1.5-2x baseline or increase >0.3 < 0.5 ml/kg/hr for 6 hrs Injury 2 Increase in Scr of 2-3x baseline < 0.5 ml/kg/hr for 12 hrs Failure 3 Increase in Scr of more than 3x baseline or Scr >4 with an acute rise of > 0.5 Loss ESRD Persistent renal failure > 4 wk Persistent renal failure > 3 mo < 0.3 ml/kg/hr for 24 hr or anuria for 12 hr Problems with Creatinine Serum creatinine does not accurately reflect the GFR in a patient who is not in steady state. Creatinine is removed by dialysis. As a result, it is usually not possible to assess kidney function by measuring the serum creatinine once dialysis is initiated. In the early stages of severe acute renal failure, the serum creatinine may be low even though the actual (not estimated) GFR is markedly reduced since there may not have been sufficient time for the creatinine to accumulate. Abnormal BUN:Cr ratio BUN: Cr > 15 BUN:Cr < 15 High protein intake. Advanced liver disease. Catabolic states. Rhabdomyloysis. Tissue necrosis. Cimetidine. Corticosteroids. Ketones. Tetracyclines. Methyldopa. Sepsis. Barbiturates. Volume loss. Cotrimexazole Low cardiac output. Obstructive uropathy. Renal: 1) Glomerular: • Glomerulonephritis Causes of AKI 2) Tubular: • Ischaemic ATN • Nephrotoxic ATN • Myeloma cast nephropathy 3) Tubulointerstesial: • Drugs • Myeloma • Sarcoid 4) Vascular Post Renal: 1) Urethral stricture 2) Prostatic hyperplasia/malignany 3) Kidney stones 4) Renal papillary necrosis 5) Retroperitoneal fibrosis 6) Carcinoma of cervix Pre-Renal (reduced renal perfusion): 1) hypovolaemia: • hypotension •Diarrhea/vomiting •Blood loss •Third space loss •Inadequate intake 2) Reduced effective circulating volume: •Cardiac failure •Septic shock •Cirrhosis 3) Drugs: •ACE-I •NSAIDs 4) Renal artery stenosis Of AKI 67% of critical care patients have AKI 12% class R 27% class I 28% class F More than half of patients with class R will progress to either class I or F 5% of patients in general intensive cares will require RRT 10-20% of surviving patients require ongoing RRT beyond hospital discharge Hoste et al Crit Care 2006 AKI and Mortality RIFLE class F have a mortality of 57% RIFLE class I 45% RIFLE class R 21 % Compared to 8.4% of patients without AKI Ostermann M, Chang RW: CCM 2007 Epidemiology of AKI in the ICU Saudi Arabia Clinical spectrum of acute renal failure Saudi Arabia. Ghacha R, Sinha AK, Al-Khursani IA. Saudi J Kidney Dis Transpl. Acute tubular necrosis (67.5%) Obstructive uropathy (30%) Mortality rate was 26% Epidemiology of AKI in the ICU Saudi Arabia Epidemiology of acute renal failure in hospitalized patients: experience from southern Saudi Arabia. Al-Homrany M. East Mediterr Health J. 2003 Acute tubular necrosis 62% sepsis (24.7%) ischemia (12.7%) rhabdomyolysis (10.7%) drugs (7.3%) malaria and snake-bites (4.6%). Overall, 40% died Clinical Picture The clinical picture of the cause. General signs/symptoms, including decreased or no urine output, flank pain, edema, hypertension, discolored urine, anorexia, vomiting, mental status changes or seizures. Many patients are asymptomatic and are noted on routine examination to have an elevated plasma creatinine concentration or an abnormal urinalysis. laboratory findings due to the renal injury. Clinical Picture Pre-Renal History and clinical picture of the cause. Tahycardia. Hypotension/Orthostatic hypotension. Dryness of mucocutaneous membranes. Oliguria ( < 400 ml/d). Anuria ( < 50 ml/d). Clinical Picture Pre-Renal Hypovolaemia: - blood loss - Third space loss: pancreatitis, GIT obstruction, hypoalbuminaemia. Cardiovascular: - infarction, tamponade, arrythmias, valvular diseases Distributive: - sepsis, cirrhosis, hepatorenal syndrome. Local renal causes: - renal artery stenosis, malignant hypertension. Certain medications Clinical Picture Pre-Renal: Medications NSAIDs, ACE-I, Cocaine, Cyclosporines. Alteration of renal perfusion, and glomerular haemodynamics. failure of glomerular pressure autoregulation. Predisposing factors: - CHF - liver cirrhosis - nephrotic syndrome - hypovolaemia - atherosclerosis - Age. Clinical Picture Pre-Renal: Medications AKI associated with ACE-I should prompt investigation to rule out bilateral renal artery stenosis. Clinical Picture Renal History and clinical picture of the cause. Acute glomerulonephritis: vasculitis, SLE, endocarditis, cryoglobulinaemia, anti-glomerular basment membrane disease. Acute interstitial nephritis: sarcoidosis, myeloprolifrative disorders. Acute tubular necrosis: ischaemia, sepsis, nephrotoxins, drugs, contrast, rhabdomyolysis, myoglobin/ haemoglobin. Clinical Picture Renal The most common cause of AKI in hospitalized patient is intrinsic renal failure due to ATN. Polypharmacy is common among most patients with chronic diseases and hospitalized patients. Allergic interstitial nephritis should be strongly considered in all patients with AKI. Rhabdomyolysis . Contrast induced AKI. Mechanisms of ATN Medications causes of allergic interstitial nephritis Penicillines Cephasporines Sulfonamides Rifampin Ciprofloxacin NSAIDs Thiazide diuretics Loop diuretics Cimetidine Phenytoin Allopurinol Chinese herb Pathophysiology of Rhabdomyolysis Clinical Picture Renal: contrast induced AKI Contrast induced AKI is predominantly via acute vasoconstriction. Risk factors: GFR < 35 ml/min, diabetic nephropathy, severe CHF, large volume of contrast, preexisting hypotension/hypokalaemia. Pathophysiology of contrast induced acute kidney injury Prevention of contrast induced AKI Administration of crystalloid(1-1.5mL/Kg/hr for 8-12 hours before a procedure) remains the safest, most efficacious, and cost-effective method of preventing contrast induced nephropathy. Administration of acetylcysteine in two 600mg doses the day along with saline infusion for patients with stable chronic renal insufficiency(Cr~ 2.0mg/dL). Type of Contrast. Clinical Picture Post-Renal Total absence of urine (anuria) is primarily observed with bilateral ureteral obstruction/ urethral obstruction. Loin or flank pain. Prostatic hyperplasia/malignancy (male). Carcinoma of cervix (female). Evaluation of AKI Evaluation of AKI Intravascular volume status is the most important factor in the evaluation of AKI. A decrease in urinary volume is often one of the initial clinical findings in AKI. The most important laboratory test for a patient with AKI is urine analysis. Both urinary sediment and urinary indices in combination with serum values can often be extremely helpful in determining the cause of AKI. Urine analysis in AKI RBC, RBC cast, Protienuria: - Glomerulonephritis – vasculitis - thrombotic microangiopathy. WBC, WBC casts: - Pyelonephritis - Interstitial nephritis. Eosinphilurea: - Glomerulonephritis - Atheroemboli - Allergic interstitial nephritis Pigmented casts, renal tubular epithelium: - ATN - Haemoglobinurea – myoglobinurea Crystallurea: - Uric Acid - Drugs - Toxins. RBC cast Hyaline cast Granular cast Granular cast Granular cast WBC cast Oval fat body and Hyaline cast WBC cast Urinary Sediment of ATN GUIDELINE OF URINARY INDICES Typical Urine Findings in Conditions that cause AKI Condition Dipstick test Sediment analysis Uosmo FENa Pre-renal Azotaemia -ve, trace few hyaline casts >500 <1 Ischaemic ATN mild to mod. proteinuria Pigmented granular cast <350 >1 Nephrotoxins mild-mod prot. Pigmented gran. Cast <350 >1 A. Interstitial Nephritis mild-mod prot, hemoglobin, WBC WBC, WBC casts, Eosin. <350 Eosin. Casts, RBC >1 A. Glomerulo Nephritis mod-severe prot. hemoglobin RBC, RBC casts >500 <1 Post-renal Azotaemia -ve, trace, WBC hemoglobin crystals, RBC < 350 >1 Radiologic Studies : Ultrasonography is most common. Safe, easy to use, informative. Principally required to assess urinary tract obstruction, kidney stones, renal cyst or mass. CT scan. Renal Biopsy Indications : Isolated glomerular hematuria with proteinuria, nephrotic syndrome, acute nephritic syndrome, unexplained acute or rapidly progressive renal failure. Contraindications: Uncorrectable bleeding diathesis, Small kidneys (indicative of chronic irreversible disease), Severe hypertension, multiple, bilateral cysts or a renal tumor, hydronephrosis, Active renal or perirenal infection, uncooperative patient. Complications: Bleeding. Biomarkers Neutrophil gelatinase–associated lipocalin (NGAL) is up- regulated in proximal tubular cells immediately following ischemic injury. Interleukin-18 (IL-18) is a proinflammatory cytokine that is activated in proximal renal tubules following injury. Cystatin C is a better marker of GFR than serum creatinine, and could identify the development of AKI 1 to 2 days before elevation in serum creatinine. Management The goal of any focused evaluation of AKI is immediate correction of its reversible causes. Recognition and relief of urinary outlet obstruction should be given the highest priority, especially for patient with anuria. Management Support of renal perfusion with either volume infusion or therapeutics that improve renal oxygen delivery should be considered before any attempt to improve urinary flow. Urinary indices should be examined before diuretic intervention. Management Renal Replacement therapy remains the cornerstone of management of patients with severe AKI Nephron Clin Pract 2009;112:c222-c229 Indications of RRT Anuria or Oliguria (UOP < 200 ml/12 hrs.) Hyperkalaemia (K > 6.5 mmol/L). Severe Acidaemia (pH < 7.1). Azotaemia ( Urea > 30 mmol/L). Clinically significant organ oedema (particularly Lungs). Uraemic: encephalopathy, pericarditis, neuropathy, myopathy. Severe dysnatraenia (Na >160 or < 115 mmol/L) Drug over dose with dialysable product. Hyperthermia. Pharmacologic treatments under study: Dopamine: no benefit Atrial Natriuretic Peptide (ANP) or ANP-analogue (Anaritide): promising Human Insulin like growth factor 1: no benefit Erythropoietin Intensive Insulin Therapy (IIT). Case 1 26 yo F is involved in a RTA, with multiple fractures, blunt chest and abdominal trauma. She was briefly hypotensive on arrival to ED, received 6L NS and normalized BP. Non contrast CT showed small retroperitoneal hematoma. On day#2 her SCr is 0.9 mg/dl, lipase is elevated and tense abdominal distension is noted. US showed massive ascites. UOP drops to <20 cc/hr despite of 10 L total IV intake. On day#3, SCr is 2.1mg/dl, CVP is 17, UNa is 10 meq/L, with a bland sediment. What is the cause of her AKI? What bedside diagnostic test and therapeutic intervention is indicated? Bladder pressure was 29 mmHg UOP and SCr improved with emergent paracenthesis. Dx: Abdominal Compartment Syndrome causing decreased renal perfusion from increased renal vein pressure. Case 2 59 yo M, hx liver transplant in 2001 and acute on chronic rejection, now decompensated ESLD, is admitted with worsening ascites, hepatic encephalopathy and GI bleed (which is now controlled). The only medications he has been receiving are Lactulose and omeprazole. He has been hemodynamically stable with average BP~100/70 mmHg. He had a 3.5 L paracenthesis on day 2. His SCr has been slowly rising from 1.2 to 4.7 mg/dl within the 2nd to 4th day of admission and his UOP has dropped to 150 cc/day. His daily FeNa is <1% despite of 2 L fluid challenge. His Urine sediment is blend. His renal US is normal. What is the cause of his AKI? Patient required HD. He had a second liver transplant and came off HD after the surgery with stable SCr of 1.4 mg/dl. Dx: Hepatorenal Syndrome (HRS) Case 3 54 yo F with CAD, on statin, started a new exercise program with intense weight training. She was brought to ED with neck pain, and LL weakness. VS stable, normal UOP, with dry mucosa. LL muscle strength 2/5 bilaterally. BUN 40 mg/dl, creatinine=8 mg/dl. FeNa 1.5%. Renal US normal. UA: 1.010, 3+ blood, few RBCs, few granular casts. What would be the next test to order? What may be the cause of her AKI? Her CPK=57,700 She was treated with IV NaHCO3 gtt to alkalinize urine to PH>6.5 . Her UOP remained normal but she required HD for uremia. Dx: ATN due to Rhabdomyolysis Case 4 72 yo M with DM, and prostate cancer metastatic to the bone, on hormonal therapy. He is admitted with weakness, progressive weight loss, and persistent nausea. His med list also includes Diclofenac sodium daily for hip pain. BP=150/90, 350cc of urine collection immediately after foley placement, and normal exam. BUN=107 mg/dl, creatinine=9.8 mg/dl (2.0 almost 6 months PTA), which remained unchanged with hydration. Uric acid=8.2 mg/dl. UA: 1.010, 1+ protein, 1+ blood, few RBCs, no cast, no WBC. US showed 10-11 cm kidneys, no hydronephrosis. What seems to be the cause for his AKI? Patient was initiated on HD for uremia and remained HD dependent for his symptomatic uremia. Patient and his family were concerned about his renal recovery (outcome), so a renal Bx was done showing severe chronic interstitial nephritis, with fibrosis and glomerulosclerosis. Dx: ESRD due to chronic tubulo-interstitial disease secondary to NSAIDs Case 5 59 yo F with prolonged HTN, kidney transplant in 2000, on norvasc, prograf and prednisone was brought in for decreased LOC. T=39, BP=95/60, HR=104, UOP=20 cc/hr, intubated for airway protection, otherwise normal exam. BUN=80 mg/dl, creatinine=6 mg/dl (normal baseline), K=6.5 meq/L, Hct=20%, Plt=20000, FeNa 1%, urine eosinophil (-), UA: 2+ blood, no protein, RBC > 50/hpf, no WBC, no cast. What would be your next step? What could be the reason for her AKI? Her PBS showed many schistocytes and fragmented RBCs. Her Prograf was replaced with Sirolimus She underwent plasmapheresis, and required HD for anuria, and persistent hyperkalemia. She came off HD after 2.5 months with stable creatinine=1.2 mg/dl. Dx: TTP secondary to Prograf Case 6 72 yo F with depression and hypothyroidism, was found by neighbors on the floor, unconscious, in respiratory distress. Intubated for airway protection. VS stable, anuric, Lungs crackles. BUN 50 mg/dl, Creatinine=4 mg/dl, with high anion gap metabolic acidosis, and an osmolar gap of > 10. Lactic acid=1.8, FeNa 1%, urine eosinophil (-), UA: 1.020, 1+ blood, no protein, few RBCs, many oxalate crystals, few granular casts. US showed normal sized kidneys with no hydronephrosis. What is your next step? What seems to be the cause for her AKI? Her ethylene Glycol level came back after 2 days to be 40 mg/dl. Pt was given Fomepizole and initiated on HD for persistent acidemia. She remained HD dependent, eventually extubated, started therapy for depression. Dx: Ethylene Glycol toxicity Case 7 38 yo M with post ERCP pancreatitis, is admitted to ICU, intubated for hypoxic respiratory distress, is anuric, febrile, and hypotensive, requiring massive volume resuscitation, on two vasopressors. He has received 11 L of NS and other IV meds within the last 8 hours and currently his CVP~12, has coarse crackles, and 2+ edema. His Creatinine rose from 1.2 to 3.5 the morning after the above event, FeNa > 1%, UNa 45 meq/L, UA: 1.010, no protein, no blood, moderate epithelial cells, many muddy brown granular cell casts, moderate epithelial cell casts. US showed normal sized kidneys with no hydronephrosis. What is the cause of his AKI? He was started on CVVH for volume control. Has had a long hospital stay complicated with polymicrobial bacteremia and VAP. Dx: ATN secondary to renal ischemia and sepsis Case 8 45 yo M with CHF and Bipolar Disorder on Lithium for 10 years, admitted for abdominal pain after a heavy meal, which turned out to be due to acute cholecyctitis. He was kept NPO on D5 1/2NS 50 cc/hr. Next morning he felt well but thirsty and hungry, BP=120/80, I/O=1200/4500. His SCr rose from 1.2 to 1.9 mg/dl. SNa 149 meq/L. UNa 10 meq/L. UOsm 190 mOsm/Kg. What is the cause of his AKI? Patients IVF was changed to ½ NS, replacing 80% of UOP per hour. SCr and SNa improved to baseline in 2 days. Dx: Prerenal azotemia secondary to renal free water loss in DI. Case 9 18 yo F with no PMH admitted with projectile vomitting, fatigue, and low PO intake. Her BP=200/110, normal UOP with dry mucosa, trace edema, and otherwise normal exam. BUN=120 mg/dl, Creat=10 mg/dl which continued to rise on the following days, Hct=25% without schistocytes on PBS, UA: 3+ protein, 3+ blood, >50 RBC, many RBC casts. FeNa 1%. US showed normal sized kidneys. What other tests do you order? What may be the cause of her AKI? ANA (-), normal complements, cryo (-), serology for hepatitis B, and C (-), P-ANCA (+), C-ANCA (-), anti-GBM (-), ASO (-), ESR 80. Her renal Bx showed crescentic glomerulonephritis, minimal non-specific immune complex deposits, without chronic changes. She remained dialysis dependent despite of steroid, cyclophosphamide, and 10 plasmapheresis treatments. Dx: Crescentic Glomerulonephritis due to Wegner’s granulomatosis THANK YOU Take Care Of Your Kidneys