15-Lead ECG
advertisement
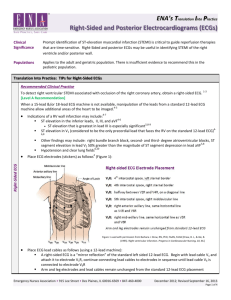
15-Lead ECG Nicole Gamblin, Alissa Graft, Holly Krause, Faith Metzinger, Sam Parmenter, Jenna Quill, Molly Reasner, Brittany Rowe, Allison Silver, Jessie Tucek Objectives8 • • To determine the effect of utilizing additional leads with the conventional 12 lead ECG in patients presenting with suspected Posterior Myocardial Infarction (PMI) To determine the utility of 15-lead ECG in the early diagnosis of acute posterior myocardial infarction Background7 • • • Acute posterior myocardial infarctions (PMI) and right ventricular myocardial infarctions are likely to be underdiagnosed; the standard 12-lead ECG does not assess these areas directly Consequently, this underdiagnosis often leads to delay of early intervention and undertreatment Leads V7, V8, and V9 view the posterior wall of the left ventricle, while leads V3R, V4R, and V5R reflect the status of the right ventricle and the posterior left ventricle • • • Background 6, 7, 8 The use of the additional leads might not only confirm the presence of AMI, but also provide a more accurate reflection of the true extent of myocardial damage. May help clinicians identify the occluded vessel before PCI, which can help in stratifying risk and planning the procedure, and in identify reocclusion after coronary interventions The 15-lead ECG can routinely be used in patients with ischemic-like chest pain. PICO For a patient with signs and symptoms of an Acute Myocardial Infarction (AMI), will the use of additional posterior chest leads as compared to a standard 12 lead improve the efficacy of diagnosing posterior wall AMIs? • • • • Problem: missing diagnoses, or delaying the diagnosis of posterior wall AMIs Intervention: use of posterior chest leads Comparison: 12 lead EKG Outcome: improving diagnosis of posterior wall acute myocardial infarction Significance of the Problem1, 3, 4 • • • Posterior myocardial infarction is commonly missed because it is not usually visible in the standard leads ST depression is absent in anterior leads of some patients who had ST elevation in posterior leads; slowing diagnosis and implementation of thrombolytic therapy In the US alone, data shows that greater than 200,000 patients annually may have a coronary occlusion that is missed by the standard 12-lead ECG (Zalenski et al., 1997) (Khaw, 1999). Literature Review3, 8 • • ST segment elevation is not seen on the standard 12 lead ECG in up to 50% of patients with posterior or circumflex-related infarction One study found 24% of participants had posterior injury that was not detected in the 12 lead. Adding 3 posterior leads found 17% more posterior injury patterns than the 12-lead. Literature Review Cont.8 • • In 345 patients with AMI, an additional 29 had ST elevation on nonstandard leads with when the 12 lead ECG was negative for ST elevation Another study found that the sensitivity for the detection of left circumflex artery occlusion improved by twofold with the posterior leads. Additionally, 11% of patients with ST elevation in the posterior lead had no elevation or depression in any other lead. Quality of the Research • Strengths o Mix of qualitative and quantitative studies o Comparison of results from many studies o Not limited to specific geographics, type of patient, unit, protocols, and treatments. • Weaknesses o Lack of randomized control trials o Small sample sizes o Research conducted within one hospital Research conducted outside of the U.S. Some research found that 15 lead, as compared to 12 lead, did not alter diagnosis, therapy, o o AACN Levels of Evidence Level Description A Meta-analysis of multiple controlled studies or metasynthesis of qualitative studies with results that consistently support a specific action, intervention, or treatment B Well-designed controlled studies, both randomized and nonrandomized, with results that consistently support a specific action, intervention, or treatment C Qualitative studies, descriptive or correlational studies, integrative reviews, systematic reviews, or randomized controlled trials with inconsistent results D Peer-reviewed professional organizational standards, with clinical studies to support recommendations E Theory-based evidence from expert opinion or multiple case reports M Manufacturer’s recommendation only Levels of Evidence • 1. • 1. Level A Somers, M., Brady, W., Bateman, D., Mattu, A., & Perron, A. (2003). A Level D Krishnaswamy, A., Lincoff, M., & Menon, V. (2009) • Level B 1. Aqel, R. A., Hage, F. G., Ellipeddi, P., Blackmon, L., McElderry, H. T., Neal Kay, G., & Plumb, V. (2009). 2. McElderry, H. T., Neal Kay, G., & Plumb, V. (2009). 3. Katoh, T., Veno, A., Tanaka, K., Suto, J., & Wei, D. (2011). 4. Khaw, K. Moreyra, A. Tannenbaum, A. Holser, M. Brewer, J. Agarwal, B. (1999). Improved detection of posterior myocardial wall ischemia with the 15-lead electrocardiogram. American Heart Journal, 138(5). 5. Rosengarten, P., Kelly, A., & Dixon, D. (2001) 6. Wung, Shu-Fen. (2007) 7. Wahab, S., Islam, A., Haque, M., Hossain, S., Kamal, M., Ali, S., & Mahabub, S. (2012). Clinical Guideline (Protocol) Individuals presenting with chest pain and other signs and symptoms of a suspected MI should have a 15-lead ECG in place of the usual 12-lead ECG protocol. Implementation • • • • • Hospital wide statement to increase awareness of change in protocol and its significance Education on placement and positioning of additional leads Education on reading and interpreting the additional views from 15-Lead ECG Considering updating and replacing current equipment if indicated Purchase of additional leads Barriers to Implementation • • • Additional time for placement of additional leads Time to educate personnel on 15 lead ECG placement Cost for new equipment for 15 lead ECG Questions? References 1. Aqel, R. A., Hage, F. G., Ellipeddi, P., Blackmon, L., McElderry, H. T., Neal Kay, G., & Plumb, V. (2009). Usefulness of three posterior chest leads for the detection of posterior wall acute myocardial infarction. The American Journal of Cardiology, 160-163. doi:10.1016/j.amjcard.2008.09.008 2. Katoh, T., Veno, A., Tanaka, K., Suto, J., & Wei, D. (2011). Clinical Significance of Synthesized Posterior/Right Sided Chest Lead Electrocardiograms in Patients with Acute Chest Pain. Journal of Nippon Medical School 78(1), 22-29. 3. Khaw, K. Moreyra, A. Tannenbaum, A. Holser, M. Brewer, J. Agarwal, B. (1999). Improved detection of posterior myocardial wall ischemia with the 15-lead electrocardiogram. American Heart Journal, 138(5). 4. Krishnaswamy, A., Lincoff, M., & Menon, V. (2009). Magnitude and consequences of missing the acute infarctrelated circumflex artery. American Heart Journal, 158(5), 706-712. doi: 10.1016/j.ahj.2009.08.024 5. Rosengarten, P., Kelly, A., & Dixon, D. (2001). Does routine use of the 15-lead ecg improve the diagnosis of acute myocardial infarction in patients with chest pain?. PubMed, 13(2), 190-193. 6. Somers, M., Brady, W., Bateman, D., Mattu, A., & Perron, A. (2003). Additional electrocardiographic leads in the ED chest pain patient: right ventricular and posterior leads. American Journal of Emergency Medicine, 21(7), 563-573. 7. Wahab, S., Islam, A., Haque, M., Hossain, S., Kamal, M., Ali, S., & Mahabub, S. (2012). Comparative study between 12 and 15 lead electrocardiograms for evaluation of acute posterior myocardial infarction. Cardiovascular Journal, 4(2), 154-163. Retrieved October 16, 2012 8. Wung, Shu-Fen. (2007). Discriminating Between Right Coronary Artery and Circumflex Artery Occlusion by Using a Noninvasive 18-Lead Electrocardiogram. American Journal of Critical Care, 16(1), 63-71.