Sink or Swim: New Waves in Fluid Resuscitation
advertisement

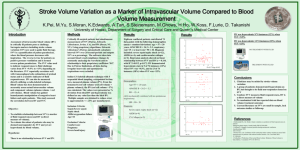
Sink or Swim: New Waves in Fluid Resuscitation Mike McEvoy, PhD, RN, CCRN, NRP Chair – Resuscitation Committee – Albany Medical Center, NY Sr. Staff RN – CTICU – Albany Medical Center EMS Coordinator – Saratoga County, NY Learning Objectives 1. Recall the incidence of patients who fail to respond to fluid boluses in the ICU 2. Discuss current controversies in fluid volume management 3. Recognize the value of measuring patient response to fluid administration www.mikemcevoy.com S/P Open AAA > BP 80/40 (MAP 58), CVP 4, HR 86, UO 5 > BP 82/38 (MAP 60), CVP 4, HR 82, UO 10 > BP 84/36 (MAP 59), CVP 4, HR 88, UO 8 3 Shock States: 1. Hypovolemic 2. Distributive 3. Cardiogenic Is there danger in the water? Permissive Hypotension in Trauma Resus IV fluids in hypovolemic shock: > No survival, some mortality Theories on IVF in trauma: 1. BP dislodges clots 2. BP = bleeding 3. IVF hemodilutes clotting factors EMS/ED: allow SBP 90, MAP 50-60 Duchesne JC et al. Damage Control Resuscitation: From Emergency Department to the Operating Room. The Amer Surgeon. 2011; 77: 201-206. Permissive Hypotension Limits SBP 90 (MAP 50 – 60 mmHg): 1. Bleeding controlled, no shock = no IVF 2. Bleeding controlled, shock 500 ml IVF (may repeat X 1) 3. Bleeding uncontrolled = no IVF Ideal permissive hypotension < 90 min. Severe damage when > 120 min. Li T, et al. Ideal Permissive Hypotension to Resuscitate Uncontrolled Hemorrhagic Shock and the Tolerance Time in Rats. Anesthesiology. 2011; 114 (1): 111-119. More than 50% of patients in which fluid loading was “clinically indicated” are non-responders and are being loaded with fluids unnecessarily! The Volume Problem > Volume expansion 1st line of therapy. > Only ½ of patients show an increase in CO as a response to fluid therapy (Defined as responders). > Need a reliable means to determine patient ability to respond to fluids. Crit Care Med – Jan 2013 Crit Care Med 2013; 41:34–40 Crit Care Med – Jan 2013 • • • • • • 27,022 simultaneous NIBP & A-line BPs 4,957 patients University teaching hospital ICU NIBP overestimated SBP in hypotension Mean from NIBP and A-line consistent MAP < 60 associated with AKI & death Crit Care Med 2013; 41:34–40 AKI: aline versus cuff Acute Kidney Injury: MAP Can We Use BP Alone? Bland, Shoemaker J Surg Obst 1978: 74 % of survivors achieved normal values 76% of NONSURVIVORS achieved normal vital signs 2001: Rivers Calls for EGDT System-based Approaches to sepsis Early-Goal Directed Therapy INCLUSION = Sepsis AND [BP < 90 after fluid OR Lactate > 4] Control Intervention EGDT CVP 8-12 Fluids CVP 8-12 MAP > 65 Vasopressors MAP > 65 Transfusions Dobutamine ScvO2 > 70% 49% mortality 33% mortality LOS 4 less days $13-16,000 savings Rivers, E., Nguyen, B., Havstad, S., Ressler, J., Muzzin, A., Knoblich, B., Peterson, E., et al. (2001). Early goal-directed therapy in the treatment of severe sepsis and septic shock. New England Journal of Medicine, 345(19), 1368–1377. System-based Approaches to sepsis Going forward after the study… Control EGDT 49% mortality 33% mortality ...treated at clinician discretion according to a protocol Do what you for hemodynamic support, with normally do. We’ll critical-care consultation, and admitted for inpatientyou. care as be watching soon as possible... ...treated in the emergency Use a rigid protocol department (by ED attending, 2 residents, according with3 nurses) multiple to a protocol for early goaldedicated team directed therapy...for at least six hours... members Rivers, E., Nguyen, B., Havstad, S., Ressler, J., Muzzin, A., Knoblich, B., Peterson, E., et al. (2001). Early goal-directed therapy in the treatment of severe sepsis and septic shock. New England Journal of Medicine, 345(19), 1368–1377. Hospital-wide impact of a standardized order set for the management of bacteremic severe sepsis After Before Thiel, S. W., Asghar, M. F., Micek, S. T., Reichley, R. M., Doherty, J. A., & Kollef, M. H. (2009). Hospital-wide impact of a standardized order set for the management of bacteremic severe sepsis*. Critical Care Medicine, 37(3), 819–824. doi:10.1097/CCM.0b013e318196206b Summary of Trials Rivers 2001 RCT Sebat 2005 Before-After Nguyen 2007 Complete or Not Goals CVP >8 MAP > 65 ScVO2 >70% HCT >30 MAP > 70 SaO2 > 92 UOP > 30ml/h SvO2 > 60 CI > 2.5 Specific Interventions Fluids, Blood, Pressors ABX, Fluids Pressors Screening, System ED-based Sepsis Education, Shock Team Interventions Team, Protocols Absolute Change in Mortality -16% -12% Thiel 2009 Before-After Levy 2011 Before-After ABX in 4 h CVP > 8, MAP > 65, ScVO2 > 70%, HCT > 30 Check Lactate Steroids Appropriate ABX in 4 h, CVP > 8, MAP > 65, ScVO2 > 70% Early ABX, Blood Cultures, Appropriate ABX, CVP > 8, MAP > 65, SvO2 > 70% ABX, Fluids, Blood, Pressors ABX, Fluids, Pressors, Steroids, Xigris, Other Supportive Care ABX, Fluids, Pressors, Steroids, Xigris, Other Supportive Care Education, Inservices, Protocols Education, Inservices, Order Set, Protocols Screening, Education, Order Sets -19% -16% -7% Sepsis Guidelines 2012 Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Critical Care Medicine 2013;41(2):580–637. Sepsis Guidelines 2012 Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Critical Care Medicine 2013;41(2):580–637. During the first 6 hrs of resuscitation, the goals of initial resuscitation of sepsis-induced hypoperfusion should include all of the following as a part of a treatment protocol (grade 1C): Drilling into Surviving Sepsis 2012 Strong evidence exists only for: 1. Quickly restoring perfusion 2. Early blood cultures Bundles A bottle of wine makes for a good evening? 5 beers make for a good evening? A fine scotch makes for a good evening? Wine + 5 Beers + fine scotch = a GREAT evening? 2012 Meta-Analysis of Fluid Bolus in Kids: Conclusions: “…fluid boluses were harmful compared to no bolus. Simple algorithms are needed to…determine who could potentially be harmed by the provision of bolus fluids, and who will benefit.” Ford N, Hargreaves S, Shanks L (2012) Mortality after Fluid Bolus in Children with Shock Due to Sepsis or Severe Infection: A Systematic Review and Meta-Analysis. PLoS ONE 7(8): e43953. doi:10.1371/journal.pone.0043953 Forest plot for the outcome of mortality: no bolus versus bolus Continuous cardiac output monitoring is the gold standard to monitor the response to a fluid challenge. Arterial Pulse Cardiac Output (APCO) Pulse Pressure Relationship to Stroke Volume > Fluctuations of blood pressure around a mean value result from the volume of blood forced into the arterial circuit during systole > Magnitude of change in pressure – i.e., pulse pressure, is a function of the magnitude of the change in stroke volume > One factor of importance is compliance of the arterial walls Limitation: Heart Rate Variability 47 SVV Arterial Pressure Based Technologies > Technologies that use the arterial pressure to determine cardiac output can be affected by the quality of the arterial pressure tracing. > Note the impact of an overdamped tracing on the LiDCO cardiac output value. Jansen & van den Berg 2005 “There is growing evidence that the pulse contour method is not the solution to providing reliable CO monitoring at the bedside.” Does Respiration Affect Pressure Waveforms? SPV, PPV, SVV Defined All measure the difference between the maximum and minimum values over a full respiratory cycle: SPV: Systolic Pressure Variation (mmHg): PPV: Pulse Pressure Variation (%): SPMax – SPMin Normal < 10 mmHg PPMax – PPmin/ PP mean Normal <13% SVV: Stroke Volume Variation (SVV%) measured over a 20 second cycle: SVMax – SVMin/SV mean Normal < 10 – 15 % SPV, PPV, SVV Dynamic Parameters Pleth Waveform SVV or PVI and Fluid Status > High variability = volume depletion (“high is dry”) Ability to observe and intervene in real time > 50% of patients are fluid non-responders The ventricle more sensitive to respiratory changes is more responsive to preload 1. Who needs fluid 2. Who will respond Clinical Evidence: Predicting Fluid Nonresponders Invasive -Maxime Cannesson, M.D., Louis Pradel Hospital , Lyon, France Lactate (Lactic Acid) Hypoperfusion severity index NL < 2, concerned when > 4 > 15 often fatal More helpful as trend (q 6 hours) Chest 2002;121;1245-1252 PLR?? SemiFowler’s > > > > 45 ° Passive Leg Raising 150 – 300 ml volume Effects < 30 sec., not > than 4 minutes Self-volume challenge Reversible InSpectraTM StO2 Systems Ardolic, Ann Emerg Med. 2010;56:S131. Cohn, J Trauma. 2007;62:44. Moore, Int Proc TSIS 2007;111. What is StO2? StO2 = hemoglobin oxygen saturation of the microcirculation SaO2 and SpO2 measure O2 saturation in the arteries. ScvO2 measures O2 saturation in the superior vena cava. SaO2 SpO2 ScvO2 SvO2 measures SvO2 O2 saturation in InSpectra StO2 StO2 measures O2 saturation in the microcirculation where O2 diffuses to tissue cells. StO2 is a measure of tissue oxygenation and is a sensitive indicator of tissue perfusion status. Cohn, J Trauma. 2007;62:44. the pulmonary artery. Intensive Care Med. 2013 Jan;39(1):93-100 What hemodynamic monitoring do you routinely use for the management of high-risk surgery patients? What are your indicators for volume expansion in patients undergoing high-risk surgery? While only 47% of intensivists believed that CVP should guide resuscitation, 86% used it because of the Surviving Sepsis Campaign Guidelines. How should we monitor preload and fluid responsiveness in shock? Why, why, why? Crit Care Med Apr 2013; 41:972–981 Why, why, why? • Lactic acidosis results from the effects of Care Med 2013; 41:972–981 the organisms, notCrit hypovolemia • Liberal fluid administration has little effect and does not improve lactic acidosis or renal function • Pulonary edema is common and exacerbated by fluid loading • Liberal fluid replacement should be avoided Fluid Resuscitation Give fluids only when needed, and no more than needed (Could 2 liters be the limit?) No value in non-responders, likely harmful Crystalloids are favored as the initial fluid Hydroxyethyl starches are likely harmful Albumin may have a role, particularly if a lot of fluid is given A lower Hb target (~7) is generally accepted Summary > We need to rethink why we’re giving fluids Important to identify who will benefit > Restoration of circulation is the goal Assess cardiac function and perfusion markers When fluids are not immediately effective – use pressors > Standardized approaches improve outcomes Continual attention to effects of individual interventions Questions?