Abdominal Aortic Aneurysms
advertisement

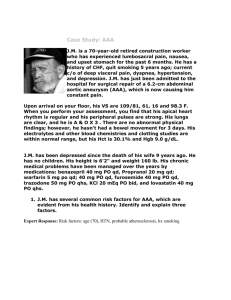
Abdominal Aortic Aneurysms Elizabeth Pensler, DO Vascular Surgery Kansas City Review April 3-5th 2014 Definition of Aneurysm • Focal and persistent dilatation of the diameter of an artery of 150% or more • Transverse diameter of 3 cm or greater • Normal aortic diameter gradually decreases from the thorax (28 mm in men) to the infrarenal location (20 mm in men) Types of Aneurysms • True vs. False (pseudoaneurysm) – True: involves all 3 layers of the arterial wall – False: Presence of blood flow outside of normal layers of arterial wall. Wall of false aneurysm is compose of the compressed, surrounding tissues. Types of Aneurysms Etiology • Degenerative • • • • Incorrectly termed atherosclerotic Not typically assoc. with occlusive disease Complex degenerative process Calcification and atherosclerotic pathology present • Inflammatory • Triad ab or back pain, pulsatile (+/- tender) abdominal mass, elevate ESR • Dx made - periaortic inflammatory rind on CT – Post-dissection- up to 20% of aneurysms are related to previous dissection. Overtime, develops into true aneurysm – Traumatic – Developmental Anomalies- persistent sciatic arteries, aberrant right subclavian artery – Infectious- Can be primary or secondary infections. – Congenital- Tuberous sclerosis, aortic coarctation, Marfan’s. Crawford Aneurysm Type Epidemiology • • • • • 15,000 Deaths per year USA 13th leading cause of death in USA 1.8-6.6% of patients in Autopsy series! Strong male predominance 3:1 - 8:1 Racial distribution Whites > Blacks Increasing Incidence of AAA • Inc. 2.6X from 2.62 deaths per 100,000 in 1981 to 6.82 per 100,000 in 2000 • Hospital admissions rose 3X • Increases in both elective admissions (from 3.05 to 7.80 per 100 000) and emergency admissions (from 7.44 to 11.23 per 100 000) • Br J Surg 2003 Dec;90(12):1510-5 Best VA; Price JF; Fowkes FG Genetic predisposition • 15-20% have 1st degree relative with AAA • 11.6x more common in persons 1st degree • Duplex 25% males and 7% females have AAA if 1st degree relative has AAA • 69% risk of AAA in offspring of women with AAA! • Females rise from 14% to 35% in affected families AAA: Associated conditions • Emphysema: Strongest independent risk factor for rupture of a known AAA – Destruction elastin matrix in lung and aortic wall may have a common cause (e.g. alpha 1 antitrypsin deficiency) Range of Potential Rupture Rates for a Given Size of Abdominal Aortic Aneurysm • • • • • • • AAA Diameter (cm) Rupture Risk (%/yr) <4 0 4-5 0.5-5 5-6 3-15 6-7 10-20 7-8 20-40 >8 30-50 Operative Mortality of AAA Repair • 3 – 5% for open repair • 1% for EVAR Assessing the AAA patient • • • • Normal - aorta 1-2.4cm & iliac 0.6-1.2cm Aneurysm - Aorta >3cm & iliac > 2cm Average expansion rate approximately 0.33 cm per year. Risk Factors for aneurysm – Older age, male gender, white race, positive family history, smoking, HTN, hypercholesterolemia, PVD, CAD. • Ultrasound – used to diagnose and monitor AAA until aneurysm approaches size at which repair considered. • Computed Tomography – used in preop assessment of AAA. Ruptured AAA • No significant overall change in mortality with open repair from 1991-2006 • Overall mortality for ruptured AAA = 90% – Mortality rate for patients who arrive at hosptial alive = 40-70% • High postop mortality rate due to MI, renal failure, and multi-organ failure – Ischemia-reperfusion injury, hemorrhagic shock, lower torso ischemia • rEVAR significantly reduces mortality of ruptured AAA patients (31 vs 50%) Screening for AAA • US Preventive Services Task Force – Men 65-75 yo who have ever smoked – Not for or against men 65-75yo who never smoked – Does not recommend screening for women • Society of Vascular Surgery, Medicare Screening – Men smoked at least 100 cigarettes during their life – men and women with a family history of AAA • Only screen patients candidates for repair. Choosing between Surgery & Observation 1. 2. 3. 4. Risk for AAA rupture without surgery Operative risk of repair Patient’s life expectancy Personal preferance of patient 1. Risk of Rupture • Size matters: – Aneurysm > 5cm 6-16% – > 7cm 33% annual rupture rate • Wall stress analysis • Saccular aneurysm have higher rate of rupture • HTN, COPD, active smoking independent predictors of rupture • (+) family hx tend to rupture • Expansion rate 2. Operative Risk of Repair • Mortality after: – elective open AAA ~ 5% – EVAR 1% • 6 independent RF’s for mortality Open repair – Creatinine > 1.8, CHF, EKG detected ischemia, Pulmonary dysfunction, older age, female gender. • Cardiac, pulmonary, renal, and GI risks with each proceudre. 3. Patient’s Life Expectancy • Very difficult to assess due to patient’s comorbidities • Typical 60yo surviving AAA repair has 13year life-expectacy • 70yo has 10year life-expectancy • 80 yo has 6 year life-expectancy. 4. Personal Preference of Patient • Fear of AAA vs. Fear of surgery • Anecdotal experiences of friends and family • Procedures provided in community by interventional specialists and surgeons. Medical Management of AAA • • • • Smoking Cessation- Single important modifiable RF Exercise Therapy- Benefit small aneurysms Beta Blockers- May decrease the rate of expansion? ACE inhibitors- Evidence is mixed, however, implicated in less aneurysm rupture. • Doxycycline – Antibiotic activiety against chlamydia species – Suppresses expression of MMP • Statins - associated with reduced aneurysm expansion rates. Decreases MMP-9 in aneurysm wall. EVAR vs. OPEN • EVAR-1 and DREAM Trials – Randomized AAA > 5.5 cm to EVAR vs. open repair – Lower 30-day mortality for EVAR (1.6% EVAR vs. 4.6% open) – Peripop mortality and severe complications 4.7% EVAR & 9.8% open repair (DREAM) – Similar all-cause mortality at 2 years – Higher rate secondary interventions in EVAR – Total cost of Tx & 4 yrs of f/u inc. for EVAR. Open Repair • • Transabdominal Approach – Previous retroperitoneal surgery – Ruptured AAA – Exposure of mid/distal portions of visceral vessels or R renal artery – R internal or external iliac artery – Co-existant abdominal pathology – Left-sided vena cava Retroperitoneal Approach – Mult. Previous intraperitoneal procedures – Abd wall stoma, ectopic/ anomaly of kidney – Inflammatory aneurysm – Proximal aortic access, endarterectomy of viceral/renal arteries needed – Obese patients – Fewer GI complications Open Repair-Complications • • • • • • Cardiac Pulmonary Renal Lower Extremity Ischemia Spinal Cord Ischemia Incisional Hernia – 14.2% ventral hernia, 9.7% SBO • Graft Infection Open Repair Complications: Colon Ischemia – Collaterals from SMA, IMA, internal iliac artery, and profunda femoris supply sigmoid colon – Mortality 40-65%, full-thickness necrosis 80-100% – Occurs in 0.6-3% of elective and – 7-27% of ruptured AAA (much more common endoscopically than clinically) Colon Ischemia – Signs and Symptoms – Bloody bowel movements – Persistent acidosis & shock – Treatment • Ischemia limited to mucosa submucosanpo, IVF, IV abx • Transmural ischemia- bowel resection, fecal diversion, creation of ostomy, washout of abdomen, IV abx. Open RepairConcomitant Pathology • Treat most life-threatening process FIRST • Avoid simult. OR prosthetic graft infection • If secondary procedure can be staged without increased risk - do aneurysm repair first • Clean procedures (ie:nephrectomy, oophrectomy) can be performed simultaneously • GI procedures should not occur at same time • Abort surgery if metastatic disease or abscesses which increase risk for graft infection discovered. Inflammatory AAA • Perianeurysmal fibrosis & inflammation • 5% of AAA • Treatment of AAA resolves the periaortic inflammation in 53% (open & EVAR) • Duodenum, left renal vein, and ureters often involved in inflammation. • PreOp ureteral stent placement recommended Infected AAA • 0.65% of AAA • Can be primary or secondary infection • Potential causes of infection: – Continguous spread of local infxn, septic embolization from distal site, bacteremia. • In the past syphilis and steptococcal species was common: – Now: staph and salmonella. • With HIV and wide-spread abx use- can be caused by any bacterial or fungal infection • Dx: fever, abdominal/back pain, high ESR, bacteremia. EVAR Types of Endoleak Types of Endoleak • Type I – Usually identified and treated @ time of stent graft implantation – Must be treated if found on post-op imaging – Associated with high likelihood of AAA rupture • Type II – 10-20% of post-op CT scan show Type II leak – 80% resolve spontaneously at 6 months – Indication to treat: persistent leak, aneurysm growth – Transcatheter tx (coil embolization) • Type III – 0-1.5% incidence – Strong predictor of rupture – Tx: re-establish continuity by additional component to bridge gap or cover hole. • Type IV – Majority resolve within one month of stent graft implantation EVAR complications • Stent-graft infection – Net infection rate of 0.43% • Pelvic ischemia – Internal iliac occlusion during EVAR – Si/sx: buttock claudication (most common 1650%), buttock necrosis, colon necrosis, spinal ischemia, lumbosacral plexus ischemia, ED (15-17%). – Ischemic colitis < 2% Discussion • “No significant difference between endovascular repair and open repair in rate of overall survival at a median of 6.4 years.” • Significantly higher rate of reinterventions in EVAR group than open group • Study limited by difference in f/u between the open and endovascular group.