Anesthesia by Dr. Carman - School of Medicine
advertisement

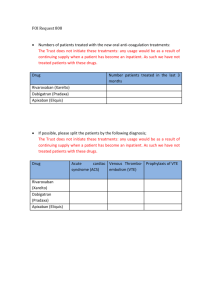
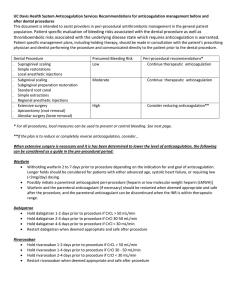
New Oral Anticoagulants in Peri-operative Medicine Teresa L. Carman, MD Director, Vascular Medicine University Hospitals Case Medical Center Associate Professor of Medicine Case Western Reserve University School of Medicine Objectives • Review the new anticoagulants and clinical indications • Discuss the pharmacology of the drugs • Review available surgical and trauma guidelines for reversing and monitoring the new anticoagulants Historical Perspective Lepirudin Argatroban Bivalirudin Desirudin 1916 Heparin 1950s 1990s Warfarin LMWHs Enoxaparin Dalteparin Tinzaparin DTIs Dabigatran Rivaroxaban Apixaban 2002 Indirect Factor Xa Inhibitors Fondaparinux 2010 2012 Endoxaban Betrixaban Ideal Anticoagulant • • • • • • • • Oral administration Rapid and predictable anticoagulant effect Broad therapeutic window Efficacious with a low bleeding risk No food-drug and drug-drug interactions No need for laboratory monitoring Easily reversible Affordable (acceptable cost-benefit ratio) Mechanisms of Anticoagulation Intrinsic system (surface contact) Extrinsic system (tissue damage) XIIa XII Tissue factor XIa XI IX VIIa IXa VIII Heparins Vitamin K antagonists Factor Xa inhibitors VII VIIIa Xa X V Va II IIa IIa (Thrombin) Direct thrombin inhibitors Fibrinogen Fibrin New Terminology • DOAs – Direct oral anticoagulants • NOAs – New oral anticoagulants • TSOAs – Target specific oral anticoagulants TSAs Emerging Therapies • Pentasacchaide anti-Xa – Idrabioptraparinux** • Oral DTIs – – – – – Ximelagatran** Dabigatran AZD0837 SB-424323 TGN-167 • Oral direct Anti-Xa – – – – – Rivaroxaban Apixaban Edoxaban Betrixaban Otamixaban • FVIIa inhibitors – rNAP-c2 – TFPI TSOAs Dabigatran VTE prevention RE-MODEL RE-NOVATE RE-MOBILIZE RE-SOLVE VTE treatment RE-COVER RE-MEDY RE-SONATE Rivaroxaban RECORD 1 RECORD 2 RECORD 3 RECORD 4 MAGELLAN EINSTEIN-DVT EINSTEIN-PE EINSTEIN-EXT Stroke prevention in AF RE-LY ROCKET-AF ARISTOTLE AVERROES ATLAS 2 APPRAISE 2 Prevention of secondary events in ACS — Apixaban ADVANCE I ADVANCE 2 ADVANCE 3 ADOPT AMPLIFY AMPLIFY-EXT TSOA • Phase III trials of new/emerging anticoagulants demonstrate promise – Ease of dosing – Bioeffective – Safe compared to conventional therapies – Monitoring and dose adjustments are typically not required • Apply caution in renal insufficiency Dabigatran • Oral direct thrombin inhibitor (DTI) • Rapidly converted from dabigatran etexilate to dabigatran • Binds clot-bound and free thrombin with high affinity and specificity • Predictable anticoagulant effect • Low plasma protein binding • No liver toxicity based on available clinical data Dabigatran • • • • • Onset is immediate with peak activity at 2-3 hrs Plasma t ½ 12-17 hours Excreted renally (80%); eliminated in bile No significant food-drug Few drug-drug interactions (amiodarone, quinidine, verapamil – dose once daily) • Bottled product has a 4-month shelf life once opened • Needs acidic environment for best absorption Dabigatran • Approved for NONVALVULAR AFIB – Fixed dose CrCl>30 ml/min - 150 mg BID • Once daily dosing with verapamil, quinidine, and amiodarone • Dose adjustment or avoidance with other strong P-gp agents – Caution with CrCl < 30 ml/min – CrCl 15-30 ml/min - 75 mg BID • FDA recommended based on pharmacology (no trial data) • No monitoring is required • NOT for use in patients with valves • Approved in Europe and Canada for orthopedic prophylaxis Rivaroxaban • Direct factor-Xa inhibitor • Inhibits free factor-Xa as well as prothrombinase-bound and clot bound factor-Xa • Circulates primarily bound to albumin • 80-100% oral bioavailability • Peak activity at 2-4 hours • T ½ - 7 to 11 hours • Hepatic metabolism with renal and fecal excretion • Avoid with CrCl <15 ml/min; caution when CrCl 1530ml/min • No food and few drug interactions Riveroxaban • VTE prophylaxis in THA/TKA – 10 mg daily (w/ or w/o food) • Nonvalvular Afib – 20 mg daily w/ evening meal – 15 mg daily with CrCl 15-50 mg/ml w/ evening meal • VTE dosing – 15 mg BID x 21 days then 20 mg daily with food • VTE extended prophylaxis – 20 mg daily with food • Approved in European Union for VTE prophylaxis after TKA/THA, nonvalvular afib, and VTE • Approved in Canada for VTE prophylaxis after TKA/THA Apixaban • Direct factor-Xa inhibitor • Inhibits free factor Xa as well as clot bound Xa and activated prothrombinase bound Xa • Peak activity at 3 hours • T ½ - 8 to 11 hours • Non-renal metabolism with renal (25-30%) and fecal (65%) excretion • Reduce dosing with ketoconazole, itraconazole, ritonair, clarithromycin Apixaban Dosing • Nonvalvular Afib – 5 mg BID – With 2 or more risk factors – dose 2.5 mg BID • age >80 • Cr > 1.5 • wt < 60 kg TSOAs J Thromb Thrombolysis 2013;36:133-140. New Anticoagulants • Benefits – Efficacy similar in to present therapy in many clinical settings – Large trials support relative safety compared to VKA – Wide therapeutic window • Problems – – – – Inability to accurately monitor the agents NO antidotes Short t ½ may leave patients unprotected with missed doses No clear indication of patients that may benefit most from the new therapies – $$$ Special Clinical Situations • Peri-procedural management – Determining the need for bridging • Acute reversal for surgery or bleeding Pre-procedural Interruption J Thromb Thrombolysis 2013;36:212-222. Pre-procedural Interruption Cleve Clin J Med 2013;80:443-451. Bridging algorithm for vitamin K antagonists and new oral anticoagulants. Gallego P et al. Circulation 2012;126:1573-1576 Copyright © American Heart Association Pre-op Management • If surgery cannot be delayed, there is an increased risk of bleeding in patients receiving anticoagulants. • Risk of bleeding should be weighed against the urgency of intervention. • Discontinue drugs minimum 1 to 2 days (CrCl ≥ 50 mL/min) • Patients with the highest risk of bleeding hold for 2-4 days – major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required • CrCl< 50 mL/min hold 2 to 5 days before elective invasive or surgical procedures van Ryn et al. Thromb Haemost 2010;103:1116-1127. Need for Bridging Estimated that >250,000 patients interrupt AC annually for procedures >10% risk 5-10% risk < 5% risk Bridging Therapy • Bridging -- transitioning warfarin to a short-acting anticoagulant for a temporary interruption of anticoagulation, especially for surgery or a potential invasive procedure (colonic polyp removal). • Pro – avoid thromboembolism – avoid prolonged hospitalization • Con – – – – – May increase bleeding complications Creates miscommunications, logistical nightmares Prolongs the hospital stay in some cases Lack of evidence (no RCTs) Published reports are cohort studies, without tight protocols Periprocedural Heparin Bridging in Patients Receiving Vitamin K Antagonists Systematic Review and Meta-Analysis of Bleeding and Thromboembolic Rates Circulation 2012; 126:1630 Vitamin K antagonist–treated patients receiving periprocedural heparin bridging appear to be at increased risk of overall (OR 5.4) and major bleeding (OR 3.6) and at similar risk of thromboembolic events compared to nonbridged patients (0.9% vs. 0.6%). Bridging Decisions • • • • • Does AC need interrupted? Is bridging required (risk assessment)? “Bridge in”– Preop strategy “Bridge out”– Postop strategy Anticoagulation Intensity – (risk/bleeding assessment) “full” or “therapeutic” (e.g., Enoxaparin 1 mg/kg BID or UFH gtt) “prophylactic” (e.g., Enoxaparin 40 mg/day or SQ UFH) Bridging Protocol Arch Cardiovasc Dis 2011;104:669-676. Basic Recommendations 1. “Bridging” is becoming more selective because of the high bleeding risks, logistical problems, and communication mishaps. 2. The higher the risk the tighter the management. 3. Don’t forget about the option of “bridging-in” with LMWH (OP) or IV UFH in-hospital when necessary. 4. “Bridging-out” may be unnecessary in many patients. Regional Anesthesia Anesthesiology 2013;118:1466-1474. Why Monitor? Monitoring • Requires understanding of the available coagulation tests • Should not be done “routinely” but limited to clinical situations a specific goal in mind – Urgent pre-op assessment – Active bleeding assessment • Presently – do not quantitatively assess the degree of anticoagulation but can make a qualitative assessment Cautions - Monitoring • Do not have reliable laboratory monitoring – 150 mg BID dose • Peak - 184 ng/ml • Trough - 90 ng/ml – PT is insensitive to dabigatran • INR rarely exceeds 1.2 – aPTT is more sensitive with less variability – Very high dabigatran levels are underestimated by aPTT values van Ryn et al. Thromb Haemost 2010;103:1116-1127. Cautions - Monitoring PT/INR and aPTT are variable based on the coagulometer and the reagent Thromb Haemost 2010;105 (epub) Cautions - Monitoring • For DTIs - ECT is the best lab monitor – not widely available/not FDA approved • Chromogenic antifactor II – FDA approved but not for monitoring DTIs • Thrombin time is too sensitive van Ryn et al. Thromb Haemost 2010;103:1116-1127. Cautions - Monitoring Limited data a best are available for rivaroxaban and apixaban for monitoring or reversal • Rivaroxaban and Apixaban influences prothrombin time (PT) > aPTT Rivaroxaban and apixaban should be able to be monitored by chromogenic Anti-Xa assays • Standards have not been set/reported Monitoring Guidelines J Thromb Thrombolysis 2013;36:187-194. Dabigatran Arch Cardiovasc Dis 2013;106:382-393. Riveroxaban Arch Cardiovasc Dis 2013;106:382-393. Managing Bleeding • • • • • • Hold the drug Local hemostatic measures Supportive PRBC/PLT transfusions FFP unlikely to be useful Initiate a hematology consult early Institutional protocols are recommended* Managing Bleeding • Specific reversal agents (“antidotes”) not yet available • Protamine sulfate and vitamin K should not be expected to affect the anticoagulant activity • With overdose – when given within 1-2 hours of ingestion activated charcoal can adsorb dabigatran (in vitro data) • Maintain adequate diuresis given renal elimination • Dabigatran can be dialyzed with removal of about 60% of drug over 2-3 hrs. • Rivaroxaban is not expected to be dialyzable (high plasma protein binding). • Consider transfusion of fresh frozen plasma, platelets or red blood cells for supportive management Reversal Agents Effect of PCC infusion (vs placebo) on the Protime after administration of Rivaroxaban 20 mg BID x 2.5 days Note: PCC infusion also reversed the effect of rivaroxaban on new thrombin generation as measured by the endogenous thrombin potential Erenberg ES et al. Circ 2011:124:1573-9 Effect of PCC infusion (vs placebo) on the Ecarin Clotting Time after administration of Dabigatran 150 mg BID x 2.5 days Note: PCC infusion did NOT reverse the anticoagulant effect of dabigatran on aPTT or Thrombin Time Managing Bleeding • Some evidence supports use of activated prothrombin complex concentrates (FEIBA) for rivaroxaban, recombinant factor VIIa (Novoseven) for dabigatran or concentrates of coagulation factors II, IX, or X (PCC) but data are limited. • 4-factor PCC recently approved in the US. – Best data available for the DTIs • Always concerns about the “potentially” prothrombotic state created with bypassing agents. • Xa recombinant reversing agent is under investigation. Phase II data was encouraging – Phase III in development Conclusions • Available anticoagulants successfully inhibit thrombin formation and the interactions of thrombin within the coagulation cascade • There is no antidote yet available. • Mechanisms to bypass the anticoagulant effect are available. • In the appropriate patient the half-life is typically short. Withholding therapy may be sufficient Conclusions • Reversibility still need to be addressed • Monitoring is problematic – Common/familiar coagulation assays are helpful but not the most accurate • Be wary in high risk clinical settings • Advise the use of Med-alert devices for patients using the drugs Ongoing Clinical Challenges • No validated tests to measure anticoagulation effect • No established therapeutic range • No true antidote for most agents • Assessment of compliance more difficult than with vitamin K antagonists • Potential for unknown long-term adverse events • Balancing cost against efficacy • Lack of head-to-head studies comparing new agents Questions