Acute Screening of Swallow in Stroke / TIA
advertisement

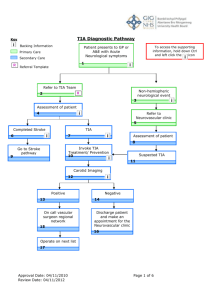
Evidence into Nursing Practice - Symposium 2011 The LMH ASSIST pilot trial (Acute Screening of Swallow in Stroke / TIA) - a multi disciplinary 'evidence into practice' partnership. Cathi Montague, RN, MClinNsg NMF, SA Prison Health Service With acknowledgement to: Linda Nimmo, Patti Holtze and Yvonne Hindman Speech Pathologists - LMH Speech Pathology Dept. Background > Lyell McEwin Hospital, 2006 • 265 funded beds • ~51000 ED presentations per year • ~500+ patients per year with 10 CVA / TIA • ED bed block (48+ hours) • focus on strategies to actively manage E.D. overcrowding. The Problem > E.D. bed block - delays in patient journey. > delays to formal speech assessment > No formal swallow screening process in E.D. > No weekend speech pathology service > No formal best practice clinical pathways for stroke care. The Problem con’t Patients with Stroke / TIA either: • Fasted, up to 72 hours over weekend. or RISKS: • deconditioning • inadvertant feeding • aspiration • inconsistent IV hydration practices Fed RISKS: • inconsistent, cursory or no swallow screen • aspiration / choking / inappropriate diet • unsafe discharge WHY? • ~65% acute stroke patients • Not always assessed • Swallow clearance quality? • Prolonged recovery • Risk of complications e.g. decubitis ulcer, falls • Length of stay ~10% of acute stroke patients. Can be silent Antibiotic use Length of stay deconditioning Risk ~3x in this population The EBP Process in 5 easy steps! 1. Ask a focused question 2. Assess the appropriate evidence 3. Appraise the evidence for validity, impact and precision 4. Apply evidence - account for patient values, preferences, clinical and policy issues. 5. Audit your practice Schneider et al. 2007 Nursing and Midwifery Research – Methods and appraisal for evidence based practice 3rd Edition Mosby /Elsevier, New South Wales – based on work by Sackett et al (2000) and Jackson et al (2006) ETHICS ??? The focussed question - PICO > Patient Population: • All patients in the E.D. with Stroke / TIA > Intervention / Area of Interest: • Early standardised screening of swallow > Comparison Intervention: • No screen, untrained screen or formal screen by speech pathologist > Outcome desired: • improved swallow screening in this at-risk group. ‘What can be done in the E.D. to minimise swallow-related adverse health outcomes for patients with stroke / TIA?’ Assess and Appraise the Evidence > Conference presentations in the Speech Pathology field on this topic. > focus in the speech pathology and medical literature. > 2000 onwards - development in NSW of consolidated care (bundles) under the TASC banner, including standardised EBP based swallow screen tool for stroke / TIA: • ASSIST tool. > Levels of evidence sufficient to implement pilot trial. Apply the evidence : The Multi-D team > Speech Pathology • Director, Speech Pathology team with ED focus. > ED CSC • inform Nursing Director > ED Liaison Nurses x2 > ED Medical Director • + inform LMH Physicians > LMH Librarian • + SALUS The Process > 2 phases of the pilot trial • First ~3months • Second – next 9 months. > Communication! > ASSIST tool > EDL Nurse education in swallow screen • Theory and Practical • Proof of competency > Education of ED staff and Inpatient Medical teams. The Audit > Integral to process > Provides rigour > Database review > Speech Pathology random audit of completed screening forms. Phase One (First 105 days) > Only 21% (N=26) of eligible population (n=123) screened by EDLN > Age range 40 to 90yrs (Medium=71yrs) > Average wait time to EDLN screen from admission= 8.09hours. > 25% (n= 15) failed ASSIST at Step 1 (highest risk) and subsequently received Speech Pathology assessment within 24hrs of initial screen. > Of those, 1 subsequently cleared for normal diet by Speech pathologist. The Audit – Phase One Collateral patient populations > Those with a secondary diagnosis of Stroke / TIA were excluded (n=176 in phase 1) > However the audit process identified these patients who would also benefit from early speech pathology input. Benefits Improved profile and multidisciplinary teamwork. Those patients were safer! Turn problems into solutions - Ongoing problem identification and problem solving Identified Problems > Visibility of service > Allowed for minor revision of ASSIST tool > Limitations of hours of cover > Documentation, communication and education! > Patients fed inadvertently > Fasting status didn’t always move with patient > Visiting Medical staff continuing ‘adhoc’ or no screen The Audit cont Phase Two (next 9 months) > Further 41 patients screened by EDLN • 27% (n=11) Pass • 73% (n=30) Fail > A number of other patients outside of ASSIST guidelines were initially reviewed and referred for Speech Pathology. STROKE / TIA? ‘THINK SWALLOW’ Final Outcomes > Speech Pathology and ED Leadership decided not to continue screening by EDLN. Issues: Cost vs benefits Ongoing assessment of nursing competency Hours of trained nursing staff cover limited Concerns over role / profession overlap Right fit? Ongoing Benefits > activity capture > Collateral implementation of ED Allied Health Assessment Team > EDLN’s as an ongoing ‘expert’ resource > FASTING armbands > Demonstrated sensitivity of the ASSIST tool Take Home Messages > Evidence into Practice uptake has to remain a focus of healthcare to benefit the patient. > Solitary discipline approaches will limit approaches to care – whole of patient care demands a whole of team approach. > Individual health disciplines each bring a unique focus to the table and can prompt new questions. Take Home Messages con’t > National standards / guidelines to support best practice. > Improving the focus can be equally as valuable as the outcomes > Lateral problems solved along the way also valuable! > Don’t duplicate or replicate - Use your librarians!! > Other great resources – your library, search tools, EBP websites ‘You treat a disease, you win, you lose. You treat a person, I guarantee you, you'll win, no matter what the outcome.’ Robin Williams ‘Patch Adams’ QUESTIONS?