PowerPoint Presentation Slideshow
advertisement

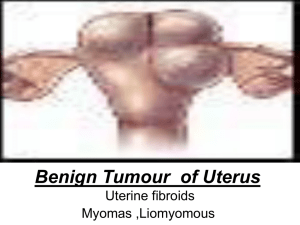
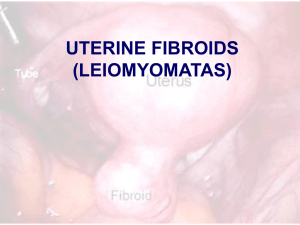
Surgical Procedures that enhance Fertility? Cleveland Clinic Tommaso Falcone,M.D. Professor & Chair Obstetrics &Gynecology Surgical Procedures that enhance Fertility? Enhance Spontaneous Pregnancy Enhance IVF outcomes Fertility preserving surgery versus fertility enhancing surgery The Most Common Causes: in Western Society Tubal disease: 15% Male factor: 25% (40%) Ovulation disorders: 25% Endometriosis: 10% Unexplained: 20% Multiple Gestation Epidemic Changing IVF paradigm Guidelines for number of embryos to transfer – Typically 1 embryo Tubal Disease: Result of Treatment Depends on severity of disease Distal tubal disease – Preserved mucosal folds – Microsurgical technique for repair CO2 laser makes no difference Salpingostomy: Result of Treatment Dubuisson et al HR1994 Canis et al F&S 1991 Donnez et al J Gynecol Surg 1989 Taylor et al F&S 2001 Milingos et al J Am Assoc Gynecol Laparosc 2000 N=81 PR% 37 N=87 PR% 40 N=25 PR % 20 N=139 PR% 25 N=61 PR% 21 Fimbrioplasty: Results of Treatment: Dubuisson et al F&S 1990 Saleh & Dlugi F&S 1997 N=31 PR% 35 N=88 PR 40% Proximal Tubal obstruction Hysteroscopic surgery 48% PR Peri-tubal adhesions No laparoscopic study One prospective study of open treatment – n-=69 Tulandi et al 1990 Am J Obstet Gynecol – Pregnancy rates at 12 and 24 months Treated Control 32 and 45% 11 and 16% When is it feasible? Importance of other pathologies Age of patient Patient preference Desire for “natural” procreation Insurance coverage Results of ART program Treatment effect Treatment effect large enough to be clinically relevant? Number needed to treat (NNT): number of subjects that must be treated to achieve one more outcome with intervention than control NNT=1/Risk difference Risk difference: Event rate treated group- Event rate control Stage 1 & 2 endometriosis Canadian study – N=172 treated & N=169 untreated – PR% 29% treated & 17% untreated – NNT= 1/.12=8.3 – NNT=9, 95 % CI, 5,33 Italian study – N=54 treated & N=47 no treatment – PR% 22% & 28% Treatment Effect Canadian study PR for pregnancies more than 20 weeks of gestation, Italian study reported any pregnancies – Combine the studies for pregnancies over 20 weeks: 27% (treated) & 18% ( non treated): NNT=12 ( 95% CI 6,112) – 20% prevalence of endometriosis – 60 diagnostic laparoscopies to get an extra pregnancy Endometriomas Drainage has a high recurrence rate Need to excise the cyst – Cochrane database 2005 Hart R et al – Excision of cyst associated with a reduced rate of recurrence; reduced symptom recurrence and increased spontaneous pregnancy rates compared with ablative surgery Endometriomas Unresponsive to medical therapy – Surgery required to remove them Jones & Sutton 2002; Alborzi et al 2004 – Surgical removal 40-50 % young women will conceive spontaneously – Laparoscopic removal of endometrioma represents the first line treatment for infertile women Stage III&IV Endometriosis: reoperation or IVF Pagidas, Falcone et al Fertility & Sterility 1996 Previously operated patients with infertility Reoperation PR were – 6% at 3 months – 18% at 7 months – 24 % at 9 months Reoperation for Stage III&IV Endometriosis ? Pagidas et al Fertility & Sterility 1996 Stage III&IV endometriosis After initial unsuccessful operative procedure to restore fertility , IVF-ET appears to be a superior alternative to reoperation In patients with chronic pain reoperation is a viable alternative Endometrial Polyps Afifi K et al Eur J Obstet Gynecol Reprod Biol- 2010 – Meta-analysis management of endometrial polyps in subfertile women: a systematic review – Significantly improved PR in women undergoing IUI Leiomyomas & Infertility: Submucosal fibroids – PR after hysteroscopic resection up to 43% Goldberg F&S 1995 Hart Br J Obstet & Gynecol 1999 Bernard Eur J Obstet Gynecol Reprod Biol 2000 Intramural fibroids distort the uterine cavity Myomectomy: Indications Shokeir et al 2010 Fertil Steril 2010 – Randomized matched trial; – Unexplained infertility – Type 0 and Type 1 myomas – Hysteroscopic surgery was performed – PR significantly improved ( 63 % vs 28 %) Ideal Candidate for Hysteroscopic procedure Single intracavitary myoma or one involving less than 50 % of the myometrium (Type 0 or 1) and up to 3cm in diameter. Uterine size less than 12-14 weeks Normal hemoglobin and normal electrolytes General Assumptions The pregnancy rate 1-2 years following laparosocpic or laparotomy myomectomy in an infertile woman ( with no other problems) is approximately – 40-60% Laparoscopic Surgery is superior to laparotomy – Challenges are Reproductive Outcome: Pregnancy rates Seracchioli et al 2000 – RCT (only study Cochrane database) – Pregnancy rate: over 3 years AM:56% LM:54% – – – – Spont Ab: AM 20% LM:12% Preterm labor:AM:7% LM:5% C/S: AM: 77% & LM:65% No ruptures EndoWrist Instrumentation TM Modeled after the human wrist. Full range of motion High-strength cable system – Transpose fingers to instrument tips Summary of Literature on Robotic Myomectomy Surgery Author Number of Robotic Year Cases Advincula 2004 AP et al Type of Study Removed Myomas Weight 35 Preliminary experience Mean = 223.2 + 244.1g Results Robotic myomectomy is new promising approach Mao SP et al 2007 1 Case report Not available Successful robotically-assisted excision of large uterine myoma measuring 9x8x7cm Bocca S et al 2007 1 Case report Not available Achievement of uncomplicated full term pregnancy after robotic myomectomy Summary of Literature on Robotic Myomectomy Surgery Author Number of Robotic Year Cases Type of Study Advincula 2007 AP, et al 29 Retrospective case matched between robotic and open myomectomy Nezhat C et al 15 Retrospective case matched between robotic and laparoscopic 2009 myomectomy Removed Myomas Weight Mean = 227.86 + 247.54g Results Robotic myomectomy approach is comparable to open approach regarding short term surgical outcome and costs Mean = 116g Robotic myomectomy (min 25-max 350)g had significant longer surgical time without offering any major advantages Cleveland ClinicObstet Gynecol 2011 Abdominal (n=393) Laparoscopic (n=93) Robotic (n=89) p value Age years 36.93 ( 5.61) 39.57 ( 9.17) 36.62 ( 5.18) < 0.001 Weight Kg 75.5 (62.8,90.7) 64.8 (59.1, 76.66) 68.04 ( 57.6, 82.5) < 0.001 Height cm 163.92 ( 13.17) 164.02 ( 6.19) 163.63 (6.62) 27(23,32) 25.1 ( 22.1, 24.1 ( 22, 28.1) 29.4) BMI kg/m2 0.97 < 0.001 Maximum Diameter of the Resected Myoma (in cm) by Surgical Approach 30 20 10 (P=0.036) 0 Abdominal Laparascopic Robotic Weight of the Resected Myomas (in grams) by Surgical Approach 2,500 2,000 Overall P < 0.001 1,500 RM vs LM < 0.001 1,000 500 0 Abdominal Laparascopic Robotic The Actual Operative Time (in minutes) by Surgical Approach 350 300 Overall P < 0.001 250 200 RM vs LM NS 150 100 50 Abdominal Laparascopic Robotic The Intra−operative Blood Loss (mL) by Surgical Approach 2,500 2,000 Overall P < 0.001 1,500 RM vs LM NS 1,000 500 0 Abdominal Laparascopic Robotic The Postoperative Hemoglobin Drop (gm/dL) by Surgical Approach 7 6 Overall P < 0.001 5 4 RM vs LM NS 3 2 1 0 Abdominal Laparascopic Robotic 8-10 cm 45° Solution: Side Docking – 4 arm Surgical Procedures that will improve IVF outcome Hydrosalpinx: meta-analysis Zeyneloglu et al Fert Steril 1998 – 13 published studies, 10 abstracts – Pregnancy rate decreased by half compared to controls (fresh & frozen cycles) – 50% lower implantation rate – Higher miscarriage rates Strandell et al HR 1999 – – – – Prospective RCT 204 patients Salpingectomy group: 36.6% No surgery: 24% Hydrosalpinx: effect of salpingectomy Subgroup analysis: Hydrosalpinges visible at ultrasound appeared to benefit the most (Strandell et al) Hydrosalpinx: alternative treatment Proximal tubal cauterization Surrey & Schoolcraft F&S 2001 – Salpingectomy: 57% – Bipolar proximal tubal occlusion: 46%; P=NS Impact of Fibroids on IVF General observations – Submucosal fibroids & intramural leiomyoma that distort the cavity have an impact IVF outcome – Subserosal leiomyomas do not affect the on IVF fertility parameters – Although less clear, there is some evidence to support the concept that intramural leiomyomas without cavity distortion may affect IVF parameters such as pregnancy rates or implantation rates. However PR & delivery rates are still high. Effect of intramural fibroids on IVF outcome Sunkara et al HR 2010 – Meta-analysis – Intramural fibroids without cavity distortion – 19 studies-6087 cycles – Significant decrease in live birth and clinical pregnancy rates – This does not mean that removal will restor PR to the levels expected in women without fibroids Impact of Fibroids on IVF Generally if there is a distortion of the uterine cavity: remove the fibroids Because of the lack of consistent or well designed studies, & high reported PR, prophylactic myomectomy pre-IVF if the cavity is normal should be individualized & not routine. No data for fibroids >5-7cm. Impact of endometriosis on IVF outcome: Meta-analysis 22 studies ( 2377 with endometriosis & 4383 without endometriosis); Barnhart et al F&S 2002 Stage I & II- 21 % per cycle ( control 27.7%) – Decrease in implantation & fertilization rates Stage III & IV –13.8 % per cycle ( control 27.7%) – Decrease in the number of oocytes retrieved Oocytes retrieved: previously operated endometriomas adapted from review Somigliana et al 2006 Endometriosis Controls-No endo Al-Azemi et al 2000 6.9+0.7 7.1+0.5 Canis et al 2001 9.4+6.2 10.9+6.5 Donnez et al 2001 10.6+4.2 8.6+6.3 Marconi et al 2002 7.5+3.9 8.7+5.1 Geber et al 2002 9.8+5.4** 12.0+5.9 Pabucco et al 2004 5.7+1.3** 7.2+1.5 Esinler et al 2006 Uni (10.8) Bi (7.1)** 11.1+6.1 Oocytes retrieved: previously operated endometriomas Endometrioma size >3cm but no upper limit given or mean diameter; others 2-5cm Pregnancy rates: – Not different in most studies – Geber et al (in women over 35) & Pabucco decreased PR Signs of decreased ovarian reserve – Marconi et al total dose of gonadotropin was higher – Esinler et al decreased antral follicle count & total dose of gonadotropin was higher Oocytes retrieved: operated vs. nonoperated normal ovary Control ovary Operated ovary Nargund et al 1996 8.9+5.1 6.3+5.2* Loh et al 1999 3.6 4.6 Donnez et al 2001 6.6+3.5 5.2+3.0 Ho et al 2002 6.1+4.1 2.9+2.6* Somigliana et al 2003 4.2+2.5 2.0+1.5* Wong et al 2004 5.2+0.8 5.6+0.9 Bilateral Endometriomas Somigliana et al HR 2008 Endometrioma group=68 patients Control group ( no ovarian surgery)=136 patients Day 3 FSH of cases> controls Number follicles/oocytes/embryos decreased/Implantation rate-lower PR/DR cases per transfer ( 14%/8%) vs. controls (28 %/25%) General Consensus Reduced responsiveness in operated patients Pregnancy rate not significantly affected-if unilateral but reduced if bilateral Large number of variables that determine outcome ( size, age, duration of infertility etc) CAUSE- surgical technique ? Actual presence of the cyst? Endometrioma surgery Outcome is dependent on technique Minimize damage to the surrounding tissue Will surgery improve IVF outcome? Surgery within 6 months of IVF vs. 6 months to 5 years No effect of the time interval between surgery & oocyte retrieval Surrey & Schoolcraft Endometriosis surgery prior to IVF: Conclusions If patient symptomatic, there does not appear to be a deleterious affect on outcome if surgery performed If patient asymptomatic: Case by Case