Syringomyelia
advertisement

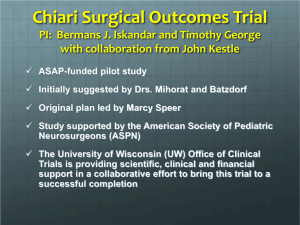
THE CHIARI MALFORMATIONS AND SYRINGOMYELIA: DEFINITIONS Bermans J. Iskandar Pediatric Neurosurgery University of Wisconsin, Madison ASAP Austin 2010 Standard Chiari Type I Chiari Type II Tonsillar descent >5mm below the plane of the foramen magnum. Caudal descent of the vermis, brainstem, and fourth ventricle. No associated brainstem herniation or supratentorial anomalies Associated with myelomeningocele and multiple brain anomalies Low frequency of hydrocephalus and syringomyelia High frequency of hydrocephalus and syringohydromyelia Rare & Poor Prognosis Chiari Type III Chiari Type IV Occipital encephalocele containing Hypoplasia or aplasia of the cerebellum Dysmorphic cerebellar and brainstem tissue New & Controversial Chiari 1.5 Chiari Zero Descent of tonsils & medulla Idiopathic syringomyelia that responds to craniocervical decompression Behaves like Chiari I JNS:Peds 2004 JNS 1998 CHIARI I MALFORMATION Diagnosis made on MRI Treatment: posterior fossa decompression. If the syrinx does not resolve: Re-explore the posterior fossa and expand the decompression Consideration of subtle craniocervical instability Consideration of benign intracranial hypertension Consideration of shunting the syrinx directly CHIARI I CASE 1: BASIC SCENARIO 8 year old boy with headaches Syrinx 1 cm tonsillar descent CHIARI I CASE 2: PSEUDOTUMOR CEREBRI 30 year-old with 1.5 cm tonsillar descent and severe symptoms Posterior fossa decompression fails LP monitoring reveals elevated ICP VP shunt Symptoms resolve CASE 3: HYDROCEPHALUS CHIARI I CASE 4: ACQUIRED CHIARI I 10 year-old who underwent serial lumbar punctures for a mild viral meningitis Develops lower cranial nerve symptoms MRI reveals new tonsillar herniation CHIARI I CASE 5: CHRONIC CRANIOCERVICAL INSTABILITY 12 year-old with Chiari I, syringomyelia, and basilar invagination Posterior fossa decompression Symptoms and syrinx don’t resolve until craniocervical fusion a year later CHIARI II MALFORMATION Likely Etiology In utero CSF leak through the myelomeningocele opening, causing caudal traction on brain structures Clinical Presentation Infants: usually asymptomatic Children: signs of lower brainstem compression: stridor, apnea, dysphagia, aspiration CHIARI II MALFORMATION Chiari II: leading cause of death in spina bifida patients in the recent past 30% of patients: brainstem symptoms by age 5 (1/3 of these die) Most dangerous period: 2-3 months of age (sometimes up to 2 years) CHIARI II MALFORMATION Current understanding VP shunt malfunction most likely cause of deterioration, rather than the Chiari Ventricle size may not change Number of Chiari II decompressions has decreased significantly since more aggressive shunt revisions SYRINGOMYELIA Fluid-filled cavity within the spinal cord Other nomenclature Hydromyelia Syringohydromyelia Spinal cord cyst SIGNS AND SYMPTOMS Dissociated sensory loss Central cord syndrome Brainstem symptoms and signs Scoliosis Chronic pain DIAGNOSTIC STUDIES Spinal MRI will show a dilated cavity with the same intensity of CSF. A complete brain and spinal MRI with and without Gadolinium is needed to determine the primary pathology. Cine MRI may also help in diagnosing abnormal CSF flow patterns. So far results have been conflicting. Rarely, myelography may help to sort some of the more difficult cases. TREATMENT - BASED ON ETIOLOGY Asymptomatic patients with small syrinx cavity and no obvious etiology are best managed with watchful waiting and serial imaging Large syrinx: Treat the cause of the syrinx, not the syrinx itself SPINA BIFIDA The syrinx may be the result Location of the syrinx within the spinal cord may help to dictate the treatment Tethered cord from the myelomenigocele repair scar Chiari II malformation Ventricular shunt malfunction. Lumbar syrinx ??tethered cord release Cervical syrinx ?? VP shunt revision Check the shunt first! CONGENITAL TETHERED CORD (SPINA BIFIDA OCCULTA) Diagnosis by MRI Treatment: Tethered cord release If syrinx is large, it is often drained at the same surgery ARACHNOIDITIS Diagnosis made on MRI Treatment: Dissection of the arachnoid scar (often difficult or impossible) Goal: Reestablish normal CSF flow Difficulties: If the arachnoiditis is so diffuse that it becomes impossible to achieve a good dissection, shunt the syrinx to the pleural or peritoneal cavities TRAUMA Post-traumatic syrinx is difficult to treat successfully Possible causes Arachnoiditis and blockage of flow causing expansion of the cord, or Atrophy long term after cord contusion Treatment: arachnoidal dissection, or syrinx shunt into the pleura or peritoneum SPINAL CORD TUMOR Diagnosis made on MRI High protein content Treatment: Tumor resection It is rare to have to shunt the syrinx in these situations. IDIOPATHIC NO IDENTIFIABLE CAUSE In a large percentage of patients, the syrinx has no identifiable cause Difficult to treat If large, syrinx shunting Rarely, posterior fossa decompression (Chiari zero) It is so far impossible to predict which patient with idiopathic syringomyelia would respond to posterior fossa decompression PROGNOSIS AND OUTCOME SYRINGOMYELIA RESOLUTION Chiari decompression Spina bifida Focal – fair prognosis Diffuse – poor, need to shunt the syrinx Trauma Excellent outcome when shunt is functional Arachnoiditis Excellent outcome Poor outcome for syringomyelia and pain Tumor: Excellent outcome for syringomyelia Overall Prognosis depends on tumor grade CONCLUSIONS Standard basic definitions Complicating factors: hydrocephalus, pseudotumor cerebri, instability, etc. Treatment controversies When to treat What to do When to do it Goals: Recognize basic concepts; recognize controversial areas; be prepared to bring these points up with your physician