case presentation of snake bite
advertisement

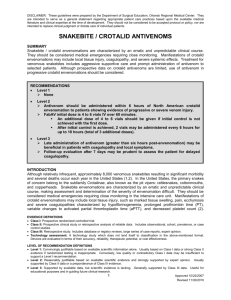
Case presentation snake bites Grampians EMET training Hub Case 1 - VICTORIA 56 year old male Arrived at 1140 - bitten by snake on right hand - whilst trying to scare it away from his children - in afternoon at nearby picnic ground - He had consumed alcohol - snake killed by friends and brought in States feels weird and nauseated No bandage applied initially What could be done differently here? Past History Angina => angioplasty 5 yrs ago, nil since Drugs Simvastatin, Aspirin Allergies Morphine Any specific features on history that you should ask about? Examination Anxious, mildly confused, breathalyser 0.32 Bite to 1st web space right hand puncture wounds dorsum Observations stable Otherwise NAD Any specific features that should be documented? Management- Initial Swab taken from bite site, then compression bandage applied IV line Blood for FBE, U+E, CK, Coagulation profile ADT given What further action is appropriate now? 30 minutes later… Venom detection kit positive for tiger and black snake Patient feels better, alert, orientated, neuro exam normal APTT 33, INR 0.9 FBE, U+E, CK normal Bandage removed 20 minutes later… A staff member has called the local wildlife park Snake seen by herpetologist, identified as copperhead What do we learn from this case? Pre hospital issues include public education, and first aid In Victoria, Australia The only antivenom required is tiger and brown snake Exceptions include snake handlers, the wildlife park/zoos, and people with other snakes as pets 25 minutes after the snake identification… Patient disorientated, slurred speech c/o weak arms and legs, and blurred vision Slight ptosis What action is needed? Do you put the bandage back on? Do give antivenom? If yes, which antivenom? Who can you ask for help? Further management One vial tiger snake antivenom given in Hartmans solution over 30 minutes IV hydrocortisone given Adrenalin and phenergan drawn up Putting the bandage back on while getting the antivenom ready is a good idea But then the antivenom must come in contact with the venom, so after infusion commenced and patient is stable, take off bandage Tiger antivenom is given for black or tiger snake HELP - seek senior help, and POISONS centre 131126 is available PRN 40 minutes later (10 mins post infusion complete) Patient feels a bit better, with clinical evidence of improvement No respiratory compromise Admitted and transferred to ICU overnight for observation Following morning Feels well, no neurological signs/symptoms, no bleeding Repeated blood tests all normal Discharged Case 2 - WESTERN AUST. 38 year old male Snake bite to middle finger of left hand Whilst trying to catch snake in house Placed a single layer compression bandage on his own arm from fingers to elbow Drove to his GP in 10 minutes No symptoms or signs of envenomation Decision to transfer to Tertiary referral Hospital by ambulance (60 minutes) In transit, the patient complained of feeling unwell with chest tightness and rapidly became unresponsive. Decision to seek medical attention at Urban Hospital en route (still 30 minutes approx from tertiary referral hospital) Initial Management 02.15 hours following the bite Unresponsive with no cardiac output ECG: pulseless electrical activity, narrow complexes CPR commenced Intubation 1mg adrenalin 1000ml normal saline Antivenom IV bolus; 1 ampoule polyvalent 2 ampoules brown snake 2 ampoules tiger snake Subsequent course Spontaneous circulation resumed within 1 minute of this antivenom, total 11 minutes CPR Platelets 33, INR >10, APTT >180, Fibrinogen < 0.3, FDP > 20 Discussed with on-call toxicologist Further antivenom: 1 ampoule polyvalent 3 ampoules brown snake Creatinine 108, ALT 113, CK 143, Troponin I < 0.4, Stabilised and transferred to tertiary centre, developed bleeding lips and gums en route 3 hours following the bite Pulse 105, BP 135/60, pupils 4mm equal and reactive Bleeding gingivae and venepuncture sites, petechiae around eyes, haematuria ECG: sinus tachycardia, RBBB, mild ST-segment depression Venom detection kit from bite site positive for brown snake Compression bandage reinforced and extended to include the whole limb Subsequent course 10 ampoules brown snake antivenom given in 100 ml 0.9% saline over 15 minutes Platelets 111, INR > 10, APTT > 180, Fibrinogen < 0.3, FDP >20 Creatinine108, ALT 201, CK 164, Troponin I < 0.4 CT head normal No further oozing noted and compression bandage removed Patient’s condition remained stable 5 hours following the bite Transferred to ICU, where remained stable Platelets 214, INR >10, APTT > 180, Fibrinogen < O.3, FDP > 20 Creatinine 133, ALT 277, CK 259, Troponin I 2.8 Further 5 ampoules brown snake antivenom infused 9.30 hours following bite Platelets 161, INR > 10, APTT > 180, Fibrinogen <0.3, FDP > 20, Creatinine 127, ALT 243, CK 366, Troponin I 10.8 15 hours following bite Platelets 148, INR 1.8, APTT 44.7, Fibrinogen 0.5, FDP > 20, Creatinine 134, ALT 223, CK 462, Troponin I 6.8 Extubated, neurologically normal. Commenced on 5 days oral prednisolone 50 mg 1 month later Follow up, well Flu like illness with rash and sore joints between days 17 and 21 after envenomation Learn from this case? A correctly applied pressure immobilisation bandage should allow stable transfer of patients long distances E.g Flying doctor service Expert advice is needed In WA, there is a different profile of snake bites The recommendations for antivenom have changed since this case, and will continue to change, hence seek advice Scenario 3 A 23 yr old man present to your emergency department complaining of dizziness, blurred vision, nausea and vomiting. He was well until about 1 hour ago. Today he has been chopping wood and re organising the wood heap, he sustained a scratch to his R thumb, but did not see what did it. What is your assessment & management? Assessment/examination cubicle ABC consider risk of snake bite swab wound for VDK pressure/immobilization full hx & ex bloods fbe, uec, clotting, glucose Investigation VDK + for brown snake FBE 12.3, 12(10), 120 UEC NAD Clot INR 4 APTT 65 Fibrinogen 0.5 what now? Management Resus prepare antivenom & give 1unit now recommended starting dose dilute as described consider premedication when do you remove the Pressure immobilisation neuro obs what next continued recheck coags do you correct the coags? Where to? There are recent updates in recommendations re treatment of coagulopathy http://www.australianprescri ber.com/magazine/35/5/152 /5 Replaces 2006 article http://www.australianprescri ber.com/magazine/29/5/125 /9/