The Role of Pancreas Transplantation in the Long Term - wi
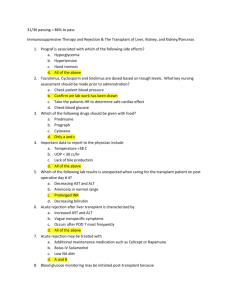
The Role of Pancreas
Transplantation in the Long Term
Management of Diabetes
Christopher Johnson MD
Professor of Surgery
Division of Transplant Surgery
Medical College of Wisconsin
Learning objectives:
1. This talk will increase your understanding about the rationale (including risk/benefit assessment) for pancreas transplantation in the management of diabetes.
2. This talk will allow you to better appreciate some of technical and immunological challenges associated with pancreas transplantation
3. This talk will help you to better anticipate therapy options for diabetic patients who have chronic kidney disease.
no disclosures
Tight control reduces end organ damage but increases the risk (2-3 fold) of severe hypoglycemic episodes ( 1 ).
1
DCCT. The Diabetes Control and
Complications Trial Research Group The
Effect of Intensive Treatment of Diabetes on the Development and Progression of
Long-Term Complications in Insulin-
Dependent Diabetes Mellitus. N Engl J
Med 1993; 329: 977–986.
DCCT trial (1441 patients randomized to intensive insulin vs. conventional insulin) designed to examine the effect of tight control on 2 ° complications (followed > 6yrs)
Retinopathy Neuropathy
Incidence progression
Prevalence of neuropathy
A successful pancreas transplant completely normalizes blood sugar control
However, it requires life long immunosuppression
Types of pancreas transplants:
Kidney/Pancreas (pts undergoing kidney transplantation)
Pancreas after kidney (already on IS)
Pancreas transplant alone (severe lifethreatening complications of DM)
Islet after kidney (no surgical procedure)
Islet transplant requires IS)
(no surgical procedure but
Combined kidney/pancreas transplant is the most common scenario for pancreas transplantation:
Indications for Simultaneous Kidney and Pancreas Transplant:
Presence of ESRD (or eGFR < 20 ml/min)
Presence of diabetes: type 1 or 2 (meeting age (< 55) and BMI criteria (<30)
Lack of major complications and/or severe cardiovascular disease which limits life expectancy
Figure 13: Unadjusted 1-year, 3-year, 5-year and 10-year pancreas graft survival by transplant type
Reversal of Lesions of Diabetic Nephropathy after Pancreas
Transplantation
Fioretto, Paola; Steffes, Michael W.; Sutherland, David E.R.; Goetz, Frederick C.; Mauer,
Michael .
NEJM 339:69-75 July 9, 1998 Number 2
Long-term survival following simultaneous kidney-pancreas transplantation versus kidney transplantation alone in patients with type 1 diabetes mellitus and renal failure
Survival estimates for patients with kidney graft function at 1 year.
Abbreviations: LD, living donor; CAD, cadaveric.
Am J Kid Disease 41:464-470. 2003
Figure 2: Waiting list death rates by
diagnosis, 1999–2008.
Diabetics who receive k/p gain more lifeyears than k-alone or non-diabetics :
k/p transplants are equally successful for type 1 and type 2 diabetes: data from SRTR
2010
What is the role of pancreas transplant in type 2 diabetes?
Diabetes affects 10% of the population
90-95% is type 2
Distinction between type 1 and 2 not always clear cut
suggested criteria:
Organ Procurement: Simultaneous Liver and
Pancreas Removal
Back table dissection:
More back table dissection…
Back table Reconstruction of Pancreatic Allograft
Arterial “Y” Graft of Donor Iliac Artery
Portal Vein Mobilization
Bladder Drainage with Systemic Venous
Anastomosis
Enteric Drainage with Portal Venous
Anastomosis
Trends in maintenance immunosuppression therapy prior to discharge for simultaneous kidney-pancreas transplantation 1994-2003
American Journal of Transplantation 2005;5(Part 2):874-886
Incidence of rejection during first year among simultaneous kidney-pancreas recipients
American Journal of Transplantation 2005;5(Part 2):874-886
ADVANCES IN PANCREAS TRANSPLANTATION .
Transplantation. 77(9) Supplement:S62-S67, May 15, 2004.
Burke G, Ciancio G, Sollinger H
Surgical Aspects of Pancreas Transplantation:
Post-Transplant Complications
•
•
Early post-operative complications (Bleeding, infection)
Venous Thrombosis
•
•
•
Reperfusion pancreatitis
Pancreas is a relatively low-flow organ
Unrecognized inherited hypercoagulable state
• in the recipient
Transplant Pancreatitis
•
•
Mild - transient amylase elevation for 48-96h
Severe – fat necrosis, infected peripancreatic fluid
• Kidney (urine leak, ureteral stricture)
Radiologic tools for transplant evaluation:
Splenic vein thrombosis:
Fluid collection on CT:
Diagnosis of Pancreatic Allograft Rejection (is difficult)
Drachenberg CB, Papadimitriou JC, Klassen DK, et.al: Evaluation of pancreas transplant needle biopsy.
Reproducibility and revision of histologic grading system. Transplantation
Histologic grading of pancreas acute allograft rejection in percutaneous needle biopsies.
Transplant Proc 1996;28(1):512-513
1997;63(11):1579-1586 .
Drachenberg C, Klassen D, Bartlett S, Hoehn-Saric E, Schweitzer E, Johnson L, Weir J and Papadimitriou J:
PAK and PTA have higher rate of immunologic graft loss after 1 year
Indications for isolated pancreas transplant (PAK or PTA):
Frequent and/or severe hypoglycemic events consistent failure of insulin-based management to prevent acute and chronic complications (poor control). clinical and/or emotional problems associated with the use of exogenous insulin therapy that are so severe as to be incapacitating
Isolated Pancreas Transplant : Recipient
Selection Criteria
IDDM, age > 18 years with an upper age limit of ?
Ability to withstand surgery and immunosuppression
Psychosocial stability/ social support/ compliance/
commitment to long-term follow-up
Diabetic secondary complications
Hyper-lability/ Hypoglycemic Unawareness
Financial resources (USA)
Absence of any exclusionary criteria:
renal function
- coronary disease
Mortality risk/benefit of PAK and PTA:
Mortality on waiting list:
Mortality after transplant:
American Journal of Transplantation 2004; 4:
2018–2026
Islet Isolation
1. Organ Procurement
2. Distension with
Collagenase
3. Digestion & Mechanical
Separation
4. Purification of Islets
5. Quantification
The “Edmonton Protocol”
Efficient Isolation Procedure
Reliable Collagenase
Steroid Free Immunosuppressive
Protocol
IL-2R Blockade
Tacrolimus
Sirolimus
Only 31% remained insulin independent at 2 years
N Engl J Med 2006;355:1318-30.
Failed islet transplants are associated with sensitization to HLA antigens:
Whole Pancreas Transplantation
Pancreatic Islet Cell Transplantation
+ +
Successful islet transplants decrease progression of nephropathy and retinopathy
Preservation of renal function
Decreased progression of retinopathy
Conclusions:
Pancreas transplants when successful, normalize glucose metabolism and increase quality (and quantity) of life.
“Good risk” diabetics (type 1 or 2) with renal failure should receive either a living donor kidney transplant or a combined kidney/pancreas transplant
Conclusions:
“Good risk” diabetics with a functioning kidney transplant (and problematic BS control) should be considered for pancreas after kidney
“Better risk” diabetics without kidney disease, but with life threatening manifestations should be considered for pancreas transplant alone
“Good” = age < 55, BMI < 30, insulin use
< 1U/kg/day, no or minimal CAD, PVD