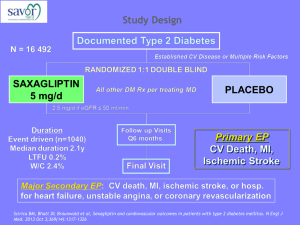
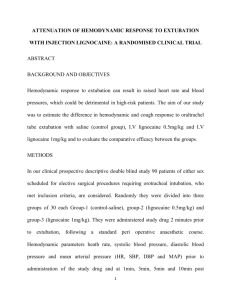
Laurence Weinberg
advertisement

Laurence Weinberg Staff Anaesthetist, Austin Hospital, Victoria Clinical Fellow, Department of Surgery, The University of Melbourne. Length of stay after open radical prostatectomy with intravenous lignocaine followed by 24-hour subcutaneous infusion: blinded, randomized, placebo controlled multicentre trial Acknowledgements o ANZCA: Project Grant o University of Melbourne Story D, Gordon I, Christophi C o Co-investigators Rachbuch C, Beilby D, Trinca J, Howard W, Yeomans M, Yanezas M, James K, McNicol L Intravenous Lignocaine • Clear advantages: abdominal surgery • Lower pain scores • Opioid sparing effects • Enhances functional recovery • Reduces immune alterations • Decreases length of hospital stay Subcutaneous Lignocaine • Neuropathic pain • Ischaemic pain Limited data for ACUTE postoperative pain Hypothesis Intraoperative IV lignocaine + 24 hrs post-operative SC lignocaine Enhances recovery Shortens length of hospital stay after open radical retropubic prostatectomy Study Design • Prospective randomised multicentre • Blinded • Inclusion criterion Adults (age > 18 years < 75 years) Elective open radical prostatectomy ASA I-III patients • Exclusion criterion x x x x Creatinine > 200 umoll/L, Abn LFT’s Chronic opioid use Allergy: morphine, LA Cardiac conduction defects/Class I anti-arrhythmic agents Study Design • • • • Human Research Ethics approval Consenting patients randomised 2 groups GA: standardized, no regional anaesthesia All patients: 1. 2. 3. 4. Induction: Propofol: 1-3 mg/kg; Fentanyl 3 ug/kg Maintenance: Volatile anaesthesia: 0.6-1 MAC, Fentanyl infusion 2.5 ug/kg/hr Surgical closure: Paracetamol IV 1 g, Ketorolac 30 mg Postoperatively: Morphine PCA, 1 mg boluses, 5 min lockout QID paracetamol, NSAID, Acute Pain Service Study Design • Lignocaine group: Pre-induction • Loading dose IV: 1.5 mg/kg • Intraop infusion IV: 1.5 mg/kg/hr Study Design • Lignocaine group: • Post-op SUBCUT infusion: 1.5 mg/kg/hr Study Design • Control group: • Normal saline: equal volume delivered in the same way Study Design • Primary outcome 1. Length of hospital stay • Secondary outcomes 1. 2. 3. 4. 5. 6. 7. 8. 9. GI function Time to mobilise Rescue analgesia and anti-emetic therapy Visual Analogue Scores for pain (VAS) 0 to 100mm Morphine consumption: 24 hours Patient satisfaction Opioid & lignocaine side effects Lignocaine plasma levels: PACU & 24 hours Adverse events Statistics analyses • Power analyses: based on a PILOT STUDY* for patients undergoing open radical prostatectomy (2007/8) who received PCA morphine alone: mean hospital stay 4.5 days (SD 26.4 hrs) • Sample size: 18 hour difference in hospital stay, power 0.8, significance level of 0.05, 38 patients per group • Analyses: intention-to-treat bases * Weinberg L, et al. Anaesthesia & Intensive Care 2010; 38: A1116 Consort diagram Total patients consented N = 85 Inclusion critreria met N = 75 Randomised Lignocaine Group N = 37 Placebo Group N = 38 Intention to treat Intention to treat Patients excluded N = 10 Laparoscopic retropubic prostatectomy N = 9 Procedure aborted (anaphylaxis) N = 1 Demographics Lignocaine Group Placebo Group Patients (n) 37 38 Age* (yrs) 61 (6.3, 44-70) 60.0 (7.6, 38-71) Weight* (kg) 85 (14.1, 52-117) 83 (11.9, 60-123) Body mass index* (kg/m2) 28 (5.05, 16.9-42.2) 26 (3.53, 21.2-35.9) ASA Class - I / II / III 24 / 13 / 0 26 / 12 / 0 Gleason Scores 7 (0.86) 7 (0.62) PSA 8.7 (5.02) 7.8 (4.85) * Data presented as SD, range Hospital Stay Hospital stay (days) Lignocaine Placebo Mean (SD) Mean (SD) Difference 3.3 (0.80) 4.6 (3.18) -1.3 P 0.017 95% CI -2.40 to -0.25 Operative variables Lignocaine Mean (SD) Placebo Mean (SD) P 95% CI Surgery duration (min) 155.7 (34.2) 141.6 (44.6) 0.13 (-4.27, 32.47) Lowest intraop temp (0C) 35.5 (0.5) 35.6 (0.5) 0.41 (-0.34, 0.14) Blood loss (ml) 1050.8 (750.9) 940.3 (651.1) 0.50 (-218, 439) Blood Tx* (% patients) 5.4% 1.00* (-16.0%, 10.9%) Colloids (total) 843.9 (926.6) 742.6 (713.8) 0.60 (-281, 483) Crystalloids (total) 3281.1 (1094.6) 2552.6 (1173.5) 0.007 (206, 1251) 7.9% • For comparison of means, standard two-sample t-tests were used • Uses Fisher's Exact Test due to comparison of proportions with small sample size Postoperative variables Lignocaine Oral sips (hrs) Free fluid (hrs) Light diet (hrs) Time to mobilise (hrs) Placebo Mean SD Mean SD Difference P 95% CI 7.2 (3.6) 8.6 (4.3) -1.4 0.17 (-3.39, 0.60) 9.7 (4.5) 13.6 (5.0) -3.9 0.002 (-6.30, -1.53) 15.5 (4.9) 20.9 (7.5) -5.4 0.002 (-8.61, -2.13) 17.4 (3.8) 22.0 (4.4) -4.6 <0.001 (-6.68, -2.52) • Two-sample t-test was used for the comparisons of means • For the comparison of percentages, Fisher’s exact test was used for the p-values and the Newcombe-Wilson approximation for the confidence intervals Adverse Effects (% patients) Lignocaine Placebo P Nausea/Vomiting 51.4% 44.7% 0.6 Pruritis 16.2% 23.7% 0.6 Dizziness 37.1% 54.1% 0.17 Visual disturbances 11.4% 16.2% 0.7 Peri-oral numbness 5.9% 5.4% 1.0 Muscle weakness 2.9% 8.1% 0.6 Paraesthesia 9.1% 8.1% 1.0 Constipation 10.8% 26.3% 0.14 Post-op Complications Lignocaine Placebo P Hypotension requiring medical intervention 5.4% 2.6% 0.6 Other cardiovascular 0.0% 0.0% 1.0 Respiratory depression 0.0% 0.0% 1.0 Pneumonia 0.0% 0.0% 1.0 Intra-abdominal sepsis 0.0% 2.6% 1.0 Wound healing 0.0% 0.0% 1.0 Renal 0.0% 0.0% 1.0 Pain Rest MEAN Lignocaine Placebo 19.3 mm 37.3 mm Difference: 18 mm 95% CI: 7.3 – 28 mm P = 0.001 Cumulative Morphine MEAN Lignocaine Placebo 38.3 mg 52.3 mg Difference: 13.9 mg 95% CI: 2.2 - 25.7 P = 0.02 Cumulative Morphine MEAN SLOPE Lignocaine Placebo 1.4 mg/hr 2.0 mg/hr Difference: -0.62 95% CI: -0.14 to -0.02 P = 0.02 Adverse events • SC cannulae: nil complications • Inadvertent administration of lignocaine Lignocaine Levels Lignocaine (ug/mL) Mean (SD) Recovery* 1.36 (0.48) 24-hours 3.20 (0.95) Range Placebo (ug/mL) Mean 0.5 – 2.19 < 0.5 1.1 – 4.96 < 0.5 SD 0.00 P 95% CI <0.001* (0.63-0.94) • * Uses Mann-Whitney of medians (adjusted for ties) due to non-Normal data • Not appropriate for formal analyses of the 24-hour data as all values in placebo were recorded as < 0.5. Conclusions IV lignocaine followed by 24-hr SC infusion • Shorter length of stay (1.3 days) • Accelerated acute rehabilitation Free fluid (3.9 hrs) Diet (5.4 hrs) Mobilisation (4.6 hrs) • Less 24-hour morphine use • Lower pain scores • Safety factors: paramount Future directions • • • • Plasma levels & pain scores Cancer recurrence Chronic pain Utility in laparoscopic radical prostatectomy Thank you 谢谢 Future directions Pearson’s correlation is r = 0.09 here, a weak positive correlation (P = 0.6)