St. Joseph Mercy Health System – ICU Collaborative
advertisement

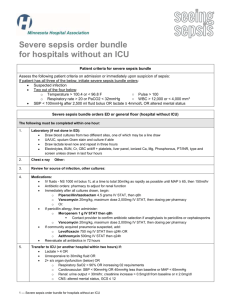
St. Joseph Mercy Health System Keystone ICU Collaborative: Making your ICUs safer The secret ingredients are culture and team Pat Posa RN, BSN, MSA System Performance Improvement Leader St. Joseph Mercy Health System Ann Arbor, MI patposa@comcast.net Objectives Review the purpose of the ICU Comprehensive UnitBased Safety Program/CLABSI Initiative. Understand how your ICU and your hospital will benefit from participation. Build the skills of physicians, nurses, and other care team to improve teamwork and build a safety culture. Engage in discussion with national experts on best practices in reducing infections, preventing central line infections Statewide initiative-75 Hospitals, 127 ICUs In Collaboration with Johns Hopkins’Quality and Research Institute Reduce errors and improve patient outcomes in ICUs Combination of evidence based medicine and quality improvement 5 interventions implemented over a 2 year Grant funded period Still going strong after 6 years!!!! Science of Safety(CUSP) BSI VAP Daily Goals Sepsis Oral Care Delirium and Progressive mobility Partnership between Johns Hopkins University and MHA Initiated with AHRQ Matching Grant Sustained with participant fees in 2005 and 2006 St. Joseph Mercy Story CUSP in the ICU and beyond Preventing CLABSI in ICU and beyond Building on CUSP and CLABSI for other work Daily goals VAP prevention Sepsis identification and management Intra-abdominal hypertension identification and management Delirium and Progressive mobility Start with: Keystone ICU Team Denise Harrison RN, MSN, Director of Critical Care Christine Curran, MD, physician project leader Mary-Anne Purtill MD, medical director SICU Pat Posa RN, MSA, system performance improvement leader Marco Hoesel MD, surgical resident Amy Heeg RN, BSN CCULivingston Brian Kurylo RN, CCU Cathy Stewart RN, BSN, CCRN Resourse Pool Diane Jones PA, cardiac surgery David Holmes, cardiac surgery Sondra RN CCU-Livingston Andreea Sandu RN, MICU Angie Malcolm RN, MICU Michael Maher, RN, SICU Emily McGee, RN, Case Nurse, SICU Shikha Kapila, Pharm. D Cheryl Morrin MPH, infection control Chris Kiser, Pharmacy, Livingston Beverly Bay-Jones, RRT, Resp Therapy Tahnee Thibodeau., RD, MICU dietitican Wendy Nieman RN, Project Impact Assess culture of safety---must get 60%+ return rate Educate staff on science of safety Identify defects Assign executive to adopt unit Learn from one defect per quarter Implement team/communication tools Reassess culture every 18 months- 2 years Keep focus on this throughout the journey!!! Understand system determines performance Use strategies to improve system performance Standardize Create Independent checks for key process Learn from Mistakes Apply strategies to both technical work and team work. Recognize that teams make wise decisions with diverse and independent input How we do this: • Educate all personnel in all the ICU—RN, RT, residents, PA/NP • Educate the attending---difficult but important • Part of orientation Safety Issues Survey 1. 2. 3. Tell us about the last patient who would have been harmed without your intervention. How will the next patient be harmed? What steps can you do to prevent this harm? by either preventing the mistake, making the mistake visible or mitigating the harm should it occur This is a very important tool. Use this to identify some of the ‘whys’ mistakes are happening and what is impacting culture Taking an identified patient safety issue from the frontline staff and create an action plan to resolve this is an early win for this program and staff buy-in Learn from a Defect Tool Designed to rigorously analyze the various components and conditions that contributed to an adverse event and is likely to be successful in the elimination of future occurrences. Tool can serve to organize factors that may have contributed to the defect and provides a logical approach to breaking down faulty system issues. Learn from a Defect Tool(LDT) Divided into three sections: Section 1 asks the users to identify what happened or the defect they want to investigate Section 2 is a framework provided for the investigators to identify any contributing factors. These factors include: patient, task, caregiver, and team related, training and education, local environment, information technology and institutional environment. Section 3 asks participants to develop an action plan with assigned responsibility for task completion and follow up dates for each item. Finding Defects to Learn From Staff feedback Event reporting Quality and safety measures Gaps in application of the evidence Have staff complete short 3 question survey Mistakes and near misses are defects Have each ICU present learning from a defect each quarter NG placed in the lungs Missed respiratory treatments Delay in radiology tests for ICU pts This is very hard to continue to do, we did it first for the first year. We didn’t keep it up----but are trying to get back to focusing on doing this. The biggest challenge is following up on each action plan giving the feedback to the staff. Daily rounds/goals Pre-procedure briefing Morning briefing Huddles Learn from a defect Executive Safety Rounds Morbidity and Mortality Conference Interdisciplinary rounds with daily goals Purpose: Improve communication among care team and family members regarding the patient’s plan of care Goals should be specific and measurable Documented where all care team members have access Checklist used during rounds prompts caregivers to focus on what needs to be accomplished that day to safely move the patient closer to transfer out of the ICU Measure effectiveness of rounds—team dynamics, communication Interdisciplinary rounds with daily goals--Challenges and Opportunities Hardest initiative to implement, especially if you have an open unit and/or no intensivists We had each unit create their own daily goal checklists---each unit culture and process is different. Changed this form multiple times---and in two units we gave up. Focused first on create a daily goal and recording those either on the white board in the room or on a sheet of paper One year ago: closed our MICU and started intensivist program in the SICU Relooking at this again, and focusing on team dynamics and created a defined role for the nurse: survey and observation Pre-procedure briefing • • • • • Make introductions Discuss patient information and procedure Agree upon a time for line insertion Review best practice for line insertion (if necessary) Nurse defines their role to physician: provide equipment, monitor patient, provide patient comfort, observe for compliance with best practices and STOP procedure if sterile process compromised • Establish communication expectation for sterile procedure breaks • Examples include: your sleeve has touched the IV pole, the guidewire touched the headboard • Identify any special supply or procedural needs • Discuss any special patient issues (IE: patient confused, patient awake) • Answer any additional questions TIME OUT: RIGHT PATIENT---RIGHT PROCEDURE Used this when rolled out CLABSI bundle to non-ICU Morning Briefing Purpose: Increase communication between physicians and nursing staff while efficiently prioritizing patient care delivery and ICU admissions and discharges What is it? A morning briefing is a dialogue between 2 or more persons using concise and relevant information to promote effective communication prior to rounds Have used this for a long time between charge nurses from shift to shift. Since we have closed the units, now this also occurs with charge nurse and intensivist. Morning Briefing Tool: answer following questions What happened overnight that I need to know about? Where should I begin rounds? (patient that requires immediate attention based on acuity) Which patients do you believe will be transferring out of the unit today? Who has discharge orders written? How many admissions are planned today? What time is the first admission? Huddles Enable teams to have frequent but short briefings so that they can stay informed, review work, make plans, and move ahead rapidly. Allow fuller participation of front-line staff and bedside caregivers, who often find it impossible to get away for the conventional hour-long improvement team meetings. They keep momentum going, as teams are able to meet more frequently. Beginning to use this strategy to begin to recovery immediately from defects--IE: falls, sepsis CUSP-Challenges and Strategies Issues Strategies Engaging frontline staff (including off-shifts) owning this work Part of team(especially night shift staff), bulletin boards, newsletters, Timely follow through with identified defects or safety issues and strategies to resolve Manager shares updates/status at staff meetings, Continued engagement of the executive MHA Keystone letters to executive, locally at each hospital—through one on one conversations Implementing strategies and tools to Learn from a defect, MDR with help improve culture and teamwork focus on communication, survey team members on perception of communication, morning briefings, debriefings Continual learning from defects Have each unit learn from a defect quarterly and share at meetings Lessons Learned Spend sufficient time on CUSP before moving on to implementing practice changes CUSP is the foundation and needs to be a continued focus-----forever!!!! Must work on culture and team improvement strategies throughout the journey CUSP must be unit based. Culture is different on each unit, therefore opportunities for improvement and strategies might be different Define at beginning a communication plan that includes all levels of the organization This work must be the responsibility of everyone, but important to have someone who’s job is to focus and drive this daily Strategies to Improve Culture Multidisciplinary Rounds with Daily Goals Closed MICU to only Intensivists Surgical Intensivists Program-SICU Learn from a defect Define/implement Critical Care Standards of Nursing and Medical Practice Standardize RN-RN Shift Handoff Simulation Program—focus on teamwork and communication ACLS certification Critical Care Nurse Certification Can we change practice through process improvement alone? or Will successful change require an altering of the value structure within the unit? Translating Evidence into Standard Practice Translating Evidence into Practice Multidisciplinaryteam (Keystone ICU team) Including bedside RN and Physician champions Reviewed evidence to define ‘best practice’ CLABSI prevention bundle Gathered baseline data Implemented the CLABSI Bundle Central line Checklist Line carts Empower nursing staff to identify and correct errors (support of chief of surgery and medicine) Communication of new practice through medical and nursing committee structures Measure rates and Compliance with process Central Line Associated Blood Stream Infection Rate: Infections per 1000 Line Days ICUs Ann Arbor MHA Keystone Baseline 2004 2005 7.6 6.12 2.2 7.7 2.51 1.51 2006 1.2 2007 1.25 2008 0.95 2009 0.66 1.25 1.17 0.98 0.89 Translating Evidence into Practice Expanding beyond the ICU • • • Can’t have multiple standards for line insertion All floors, ED, OR and anywhere they put in a line Got a group together of non ICU providers to define a process for line insertion • • • • • Pre-procedure briefing Central line bag vs line cart Talk with medical and surgical residents and asked them what their barriers were to placing the lines following the best practice strategies Challenges with getting denominator: line days in the non-ICU area. Our focus now is the non-ICU CLABSI and understanding why they are happening Getting to Zero and Sustaining the Gains Monitor process and outcomes and provide information to team and staff Try to understand ‘why’ if an infection occurs Continue to evaluate the evidence Apply additional evidence-based strategies as necessary based on the causes of the defect: CHG baths CHG dressing Antiseptic/antimicrobial catheters After CLABSI—what was next? Chose VAP prevention, since it was the other major HAI in the ICU Ensure you have respiratory therapy on your team Used same model for implementation Engage: what are our rates? and how many people are dying---tell stories Educate: review the evidence and agree on the bundle components, Execute: bedside tools, automatic orders for pts on the vent Evaluate: prospective vent bundle rounding Ventilator Pneumonia Prevention Bundle HOB at 30 degrees WAKE UP AND BREATH Daily Spontaneous Breathing Trials Appropriate Sedation PUD Prophylaxis DVT Prophylaxis Glucose Control Oral Care q 2 hours plus CHG rinse every 12 hrs Don’t routinely instill NS with suctioning Handling of suctioning and oral care equipment Use of pulmonary specialty beds Subglottal suctioning Progressive Mobility Ventilator Associated Pneumonia: Infections per 1000 Ventilator Days Baseline 2004 2005 2006 2007 2008 2009 ICUs Ann Arbor MHA Keystone 7.75 3.89 1.9 1.53 3.96 2.05 1.44 7.6 4.68 3.87 2.89 2.46 1.93 1.6 Challenges/Strategies with Vent Bundle Issues Strategies Sedation Holiday •Nurses fear that pt will be wild •No one’s responsibility Daily vent bundle rounding, set specific time to do the holiday, link with SBT, understand why the nurses aren’t doing it, SBT •RT staffing •Poor communication between RNRT Working with RT to define time to perform these that will result in patient being successful, discuss on rounds everyday Glucose Control *lacking evidence for best target * Time consuming Selected middle of road target, measure rate of hypoglycemia, revise targets based on new evidence Severe Sepsis: A Significant Healthcare Challenge Major cause of morbidity and mortality worldwide Leading cause of death in noncoronary ICU (US)1 10th leading cause of death overall (US)2* More than 750,000 cases of severe sepsis in the US annually3 In the US, more than 500 patients die of severe sepsis daily3† * Based on data for septicemia † Reflects hospital-wide cases of severe sepsis as defined by infection in the presence of organ dysfunction 1. Sands KE, Bates DW, Lanken PN, et al. Epidemiology of sepsis syndrome in 8 academic medical centers. JAMA 1997;278:234-40. 2. National Vital Statistics Reports. 2005. 3. Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome and associated costs of care. Crit Care Med 2001;29:1303-10. The Severe Sepsis Bundles: Surviving Sepsis Campaign/IHI Resuscitation Bundle Management Bundle (To be accomplished as soon as possible over first 6 hours): (To be accomplished as soon as possible over first 24 hours): Serum lactate measured. Blood cultures obtained prior to antibiotics administered. (1C) Perform imaging studies promptly to fine source (1C) From the time of presentation, broad- spectrum antibiotics within 3 hours for ED admissions and 1 hour for non-ED ICU admissions. (1D/1B) For hypotension and/or lactate > 4 mmol/L: Deliver an initial minimum of 20 mL/kg of crystalloid (or colloid equivalent) (1C) Apply vasopressors for hypotension not responding to initial fluid resuscitation to maintain MAP > 65 mmHg. For persistent hypotension despite initial fluid resuscitation (septic shock) and/or lactate > 4 mmol/L: 1C Achieve CVP > 8 mmHg & MAP > 65 mmHg & UO >0.5mL/kg/hr Achieve ScvO2 of > 70% or SvO2 > 65%. if ScvO2 not > 70% blood or dobutamine (2C) Low-dose steroids administered for septic shock in accordance with a standardized ICU policy. (Given to patients who respond poorly to fluids or vasopressors) (2C) Drotrecogin alfa (activated) administered in accordance with a standardized ICU policy. (Given to patients with sepsis induced organ dysfunction at high risk of death (2B) Glucose control maintained to < 150 mg/dL (8.3 mmol/L). (2C) Tidal volume 6 ml/kg (1B) Inspiratory plateau pressures < 30 cmH2O for mechanically ventilated patients. (1C) Adapted from the revised guidelines: CCM 2008;36:296327. 4-Tier Process for Severe Sepsis Program Implementation© Sepsis Solutions Int. Measuring Success Implementation of the Sepsis Bundle Early Screening with Tools and Triggers Organizational Consensus that Severe Sepsis Must be Managed Early and Aggressively Severe Sepsis Screening Tool Septic Shock Clinical Pathway Challenges/Strategies with Sepsis Program Issues Strategies Staff buy-in Part of team, Education frequently, daily rounds by sepsis program coordinator, data, data, data, executive physician support, executive management support Identification of severe sepsis patient Screening process, lactate rounds, RRT Achieving interventions in timely manner Bedside tools, pocket cards, education, daily rounding by sepsis program coordinator Continual learning---work in progress. This program takes a long time to have it become the standard of practice Sepsis Mortality Sepsis Program Outcomes Severe Sepsis/Septic Shock 65% of patients achieve resuscitation goals within 6 hours of septic shock diagnosis Hospital mortality: decrease from 45% to 26% Hospital average LOS: decrease from 26 days to 14 days Lessons Learned- Sepsis Must have program coordinator (like stroke and trauma) to oversee and lead this work. This person has to have leadership skill set and thick skin. ICU medical leadership plays key role in physician buy-in Frequent team meeting (twice a month)—lots of work by coordinator between meetings to ensure continued forward movement and buy-in Employ all change management strategies Data is hard to capture, but VITAL to move program forward Keep executive management engaged---give them frequent data, have them help with removing barriers ACCOUNTABILITY for all team members What’s Next Program lead (nurse and physician) continue to review literature and identify gaps in practice Delirium Progressive mobility A Healthcare Imperative “In medicine, as in any profession, we must grapple with systems, resources, circumstances, people-and our own shortcomings, as well. We face obstacles of seemingly endless variety. Yet somehow we must advance, we must refine, we must improve.” Atul Gawande, Better: A Surgeon’s Notes on Performance QUESTIONS ????? Objectives Review the purpose of the ICU Comprehensive UnitBased Safety Program/CLABSI Initiative. Understand how your ICU and your hospital will benefit from participation. Build the skills of physicians, nurses, and other care team to improve teamwork and build a safety culture. Engage in discussion with national experts on best practices in reducing infections, preventing central line infections