AB Comp Workshop Powerpoint - TEACH | Training in Early
advertisement

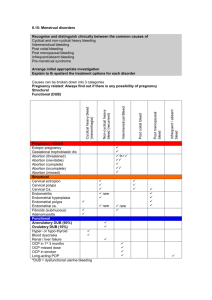
Abortion Complications Management Workshop Earlier Procedures are Safer-- CDC’s Abortion Mortality Surveillance System Currently, gestational age = strongest risk factor for abortion-related mortality Lowest risk of death: abortions < 8 weeks Mortality risk is increases 38% for each additional week of pregnancy Bartlet 2004 Abortion Related Mortality 1st Trimester: Infection (33%) Hemorrhage (14%) 2nd Trimester: Hemorrhage (40%) Paul 2009 Emergency Prevention Emergency carts, boxes, cards on site Appropriate history; patient selection Pre-op labs: Hgb Careful dating (clinical +/- dating) Adequate cervical prep (miso, lam) Vasopressin in PCB > 12 wks (Edelman 2006) Uterotonics available Transfer agreements w/ nearby hospitals Procedural Pearls Careful exam for uterine axis Cautious dilation Avoid overconfidence Develop 6th sense Low threshold to use os finders, US, hCGs Careful evaluation of POC Proceed quickly to next action Develop stress readiness TEACH Simulation Innovations Papaya: a memorable MVA & PCB model Historically used as an abortifacient In dialects means “vagina” Pitaya = dragon fruit: helpful model for practicing comp management steps Also thought to be helpful in pregnancy Paul, 2005; Goodman NAF 2013 Case 1 24 y/o G4P3, 2 prior c/s, 8w5d desiring AB MVA quickly fills up with blood You empty it, recharge and it again fills with blood. You ask your assistant to prepare another MVA but it promptly fills with blood when attached to the cannula. What do you suspect? What do you do? Demo and Group Brainstorm Causes of Hemorrhage 4 Ts Tissue: Retained Clot, Tissue, Hematometra Tone: Uterine Atony Trauma: Perforation, Cervical Lacerations Thrombin: Rare Bleeding Disorders, DIC ALSO 2013 Risk Factors for Hemorrhage Cause Risk Factors Tissue Incomplete procedure Less surgical experience Hematometra Abnormal placentation Tone Increasing EGA Prior C/S Previous obstetrical hemorrhage Increasing maternal age * General anesthesia Trauma Uterine flexion Increasing EGA Nulliparity Inadequate cervical dilation Thrombin Personal / FH bleeding or disorder Anticoagulation (esp. increasing EGA) SFP Guideline 2012 Algorithm – 7 T’s 6 T’s : 2 steps each 4 T’s (Tissue, Tone, Trauma, Thrombin) Treatment plan Transfer (Teamwork with a leadership role) Tissue 4 Ts: Think tissue first Re-aspiration Tone (Atony) Medications Misoprostol 800-1000 mcg SL/ BU/ PR Methergine 0.2 mg IM, IC, IV (HTN) (Min evidence for 1 particular agent) Massage SFP Guideline 2012 Trauma Assess bleeding source Walk cervix Cannula test Ultrasound Think perforation if free fluid Free fluid in cul-de-sac Thrombin Bleeding history? Appropriate tests clot test, repeat hgb, coags Note: Women taking anticoags did not have clinically significant increased VB < 12 weeks Kaneshiro 2011, SFP Guideline 2012 Additionally Treatment Start IVF Balloon tamponade (30-80 cc) Transfer Assess VS q 5 minutes Initiate transfer (Teamwork with a leadership role) Communicate with patient & delegate roles Stay calm under pressure Individual Simulation Groups of 3 1 provider, 1 assistant, 1 tester 15 minutes for each provider; 1-2 run throughs 1 point for each step Please complete and hand-in assessment These patients don’t respond to usual measures Give provider opportunity to think it through Review Hemorrhage Algorithm – 7 T’s Recognize heavy bleeding; initiate algorithm 6 T’s : 2 steps each 4 T’s (Tissue, Tone, Trauma, Thrombin) Treatment Transfer (Teamwork) Case 2 22 y/o G2P0 woman after uncomplicated 10 week abortion Called from recovery to evaluate for uterine pain with hypotension DDx and evaluation? Emergencies Specific to Surgical Abortion: Tissue: Acute Hematometra Pathophysiology Relative cervical stenosis plus uterine hypotonia Leads to retention of clotted blood in uterus Diagnosis Usually within first hour post-procedure US shows clotted blood in uterus Emergencies Specific to Surgical Abortion: Tissue: Acute Hematometra Diagnosis Vital Signs May be hypotensive; orthostatic(HoTN with standing) Signs Uterine enlargement / tenderness on exam Symptoms Usually little or no vaginal bleeding Patient may be asymptomatic when supine Severe cramping, lower abdominal pain, rectal presssure Dizziness/faintness Emergencies Specific to Surgical Abortion: Tissue: Acute Hematometra Management Re-aspiration usually provides complete resolution If not resolving or to prevent re-accumulation, consider uterotonics Case 3 33 y/o G4P3, h/o CS x 2, 12 wk EGA Dilation mildly difficult While inserting cannula into retroflexed uterus, you feel cannula get hung up at one point, and then slide in easily without a “stopping point.” Patient feels something sharp. Prevention? DDx? What should you do now? Trauma: Uterine Perforation 1st Tri: Fundal Advanced GA Few complications More likely lateral Bleed more Incidence 0.1 – 3 / 1000 SFP Guideline 2012 Emergencies Specific to Surgical Abortion: Trauma: Uterine Perforation Three types “Benign” - midline with blunt instrument, no suction “Intermediate” – perforation with suction on, no abdominal contents are seen or serious bleeding “Serious” - perforation with suction on, and abdominal contents (bowel, omentum, etc.) seen or heavy bleeding occurs How to Prevent? Increasing experience Careful exam; re-examine if necessary Shorter wide speculum Traction on tenaculum Posterior placement for a retro-flexed uterus Os finder US guidance early Consider rigid curved cannula to get angle Cervical ripening with misoprostol Emergencies Specific to Surgical Abortion: Trauma: Uterine Perforation If prior to start of abortion: STOP immediately INFORM of what is happening US: re-identify uterine cavity, evaluate bleeding OBSERVE in recovery room 1-1/2- 2 hours Antibiotics If stable, d/c home with phone f/u x 1-2 days Reschedule abortion 1-2 weeks later Alternatively, at clinician discretion, complete procedure under US guidance Emergencies Specific to Surgical Abortion: Trauma: Uterine Perforation Type 2 - “Intermediate Risk” Suction on; no excess bleeding or abd contents Stop suction Remove cannula without suction US to re-identify uterine cavity, evaluate bleeding May occur at end of procedure → uterus empty OBSERVE 1-1/2- 2 hours or send for observation Antibiotics At clinician discretion, complete procedure under US guidance or with laparoscopic visualization Emergencies Specific to Surgical Abortion: Trauma: Uterine Perforation Type 3 - “Serious Risk” Perforation with suction on Intra-abdominal contents seen in cx or POC +/- Severe pain or excessive bleeding Stop procedure immediately US to identify uterine cavity, evaluate bleeding Antibiotics; re-check hgb & abd exam Must be transferred, usually operated on (at the discretion of the admitting physician) Stable patient may be evaluated using laparoscopy But usually lapartomy to run bowel As needed: UA Embolization, Hysterectomy Emergencies Specific to Surgical Abortion: Trauma: Cervical Laceration Pathophysiology May occur inadvertently during sounding or dilation Or withdrawing sharp fetal parts Diagnosis Laceration obvious at time of procedure or after Persistent, bright red bleeding after procedure Examination Walk cervix with o-rings If visible: note location, length If not visible: cannula test: start at fundus, slowly withdraw to ID site Emergencies Specific to Surgical Abortion: Trauma: Cervical Laceration Management External/Low Cervical lac < 2 cm in length usually heal without leaving a defect and require no repair Pressure +/- vasopressin, silver nitrate, monsels Exception → brisk bleeding that continues → repair High Consider vasopressin, clamping Often require surgical repair in OR Hospital Transfer Call for ambulance Inform front office Duplicate pertinent charting Notify ER / OB Notify medical director Summary Hemorrhage is a common cause of abortion-related mortality. 50% of women have no risk factors Critical to prepare Tissue is more common cause after abortion than postpartum, where tone (atony is 70%). 40% of post-abortal hemorrhage may be controlled by medications alone. Frick 2010; SFP Guideline 2012 Key Points Keep good habits: Develop 6th sense Avoid overconfidence & negative self-talk Have low threshold to use tools: os finders, US Have a life line (by phone) POC eval & hCGs as needed Develop stress readiness: quarterly scenarios If you do enough, you’ll have comps Questions Thank you Please fill out evaluations!