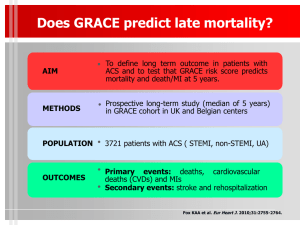
Key Quality Standards
advertisement

Quality Standards for Patients Treated by PCI Peter F Ludman NO CONFLICT OF INTEREST TO DECLARE Quality Standards for Patients treated by PCI • Caution about ‘standards’ • Overall Structure for assessing outcomes • What are Quality Standards • Options for Standards Quality Standards for Patients treated by PCI • Caution about ‘standards’ • Overall Structure for assessing outcomes • What are Quality Standards • Options for Standards Robert Liston 1794-1847 Robert Liston • 1st Professor of Surgery UCL • 1st Operation under GA in Europe • Prior to anaesthetics: – Speed • ↓ Pain • Survival • Quality = Speed – “the fastest knife in the West End. He could amputate a leg in 2 ½ minutes” Robert Liston • A High Quality Service? • Results: – Amputation 2 ½ minutes • Patient died from gangrene – Assistant’s fingers inadvertently cut through • Assistant died from gangrene – Cut coat tails of distinguished surgical spectator • Died of ‘fright’ Trolley waits • It is unacceptable that some patients have to wait on trolleys before being admitted to hospital • 2000 target – Trolley wait to < 12 hr • 2004 target – Trolley wait < 4 hours Target ‘reports’ • Inadequate resource Creativity • Patients held in ambulances – clock doesn't start England 2007-08 Time spent in A&E http://www.ic.nhs.uk/statistics-and-data-collections Local Variation in Pattern http://www.ic.nhs.uk/statistics-and-data-collections National pattern Extremes England 2007-08 Time spent in A&E http://www.ic.nhs.uk/statistics-and-data-collections England 2007-08 Time spent in A&E http://www.ic.nhs.uk/statistics-and-data-collections England 2007-08 Time spent in A&E http://www.ic.nhs.uk/statistics-and-data-collections • 66% of all patients are sent to ward in last 10 min of 4 hours deadline • ? Correct decision • ? Correct wards Measurement of Quality • Aim – Highest quality of care for patients – Outcomes are the true measure of quality • But – No single outcome captures results of care – Measures may be too narrow • single department / single intervention • May destabilize care in unmeasured area – Measures may be too broad • entire hospital rates of acquired infection – Measure of process are convenient but surrogates – Measurement leads to gaming Quality Standards for Patients treated by PCI • Caution about ‘standards’ • Overall Structure for assessing outcomes • What are Quality Standards • Options for Standards Outcome Measurement Hierachy Porter NEJM 2010;363:2477 Health Status Tier 1 Achieved or Retained Survival Degree of Health or recovery Time to recovery and return to normal activity Process of Tier 2 recovery Disutility of care or treatment process Sustainability of health & nature of recurrences Sustainability Tier 3 of health Long term consequences of therapy Outcome Measurement Hierachy Porter NEJM 2010;363:2477 Health Status Tier 1 Achieved or Retained Survival Degree of Health or recovery Time to recovery and return to normal activity Process of Tier 2 recovery Disutility of care or treatment process Sustainability of health & nature of recurrences Sustainability Tier 3 of health Long term consequences of therapy Outcome Measurement Hierachy Porter NEJM 2010;363:2477 Health Status Tier 1 Achieved or Retained Survival Degree of Health or recovery Time to recovery and return to normal activity Process of Tier 2 recovery Disutility of care or treatment process Sustainability of health & nature of recurrences Sustainability Tier 3 of health Long term consequences of therapy Outcome Measurement Hierachy Porter NEJM 2010;363:2477 Health Status Tier 1 Achieved or Retained Survival Degree of Health or recovery Time to recovery and return to normal activity Process of Tier 2 recovery Disutility of care or treatment process Sustainability of health & nature of recurrences Sustainability Tier 3 of health Long term consequences of therapy Outcome Measurement Hierachy Survival Mortality post procedure Risk adjustment Degree of Health or recovery Functional level CCS class / QoL measures Time to recovery and return to normal activity Time to referral / to investigation to Rx / to recovery post Rx / time to return to normal activities / return to work Disutility of care or treatment process MACCE / delay to emergency Rx / pain / access site comps / drug side effects / appropriateness of Rx / medical errors Sustainability of health & nature of recurrences Long term consequences of therapy Maintained freedom from symptoms / need for repeat PCI / staged procedures Stent thrombosis / drug side effects Features for Outcome measures • • • • Important to patients Occurrence sufficiently frequent Features to incorporate entire hierarchy Practical issues regarding measurement – Care with measures that encourage gaming – Objective, standardised and clearly defined – Methods for gathering data Quality Standards for Patients treated by PCI • Caution about ‘standards’ • Overall Structure for assessing outcomes • What are Quality Standards • Options for Standards White Paper July 2010 Equity and Excellence: Liberating the NHS Quality Standards Quality Standards http://www.nice.org.uk/guidance/qualitystandards/ • Specific concise statements that: – Act as markers of high quality, cost-effective patient care across a pathway or clinical area – Derived from best available evidence – Produced collaboratively with NHS and social care, with their partners and service users National Quality Board • Established 2009 • Champion quality and ensure alignment in quality throughout NHS • ‘Multi-stakeholder’ board National Quality Board NQB Prioritisation Committee NICE topic Expert Group Ministers Refer topics to NICE • Draw up draft standards – based on NICE guidance and – other NHS ‘accredited’ sources 6/52 Field testing consultation NICE Quality Standards Program Board NICE Guidance Executive Published on NICE website Use of Quality Standards • Patients and Public – Information regarding the quality of care they can expect to receive • Clinical staff – Ensure care provided is based on latest evidence and best practice • Audit • Governance • Professional development and revalidation • Provider organisations – A framework for Quality Accounts – Assess the quality of care being delivered – Highlight areas for improvement and monitor changes • Commissioners – Ensure best care being delivered via contracting process – Incentive payments (Commissioning for quality improvement CQUIN) – Demonstration of World Class commissioning competencies Quality Standards for Patients treated by PCI • Caution about ‘standards’ • Overall Structure for assessing outcomes • What are Quality Standards • Options for Standards NICE guidance so far • Technology Appraisals – Drug Eluting Stents TA 152 (July 2008) • DES if artery < 3 mm diameter or lesion > 15mm long • Price difference between BEM and DES <= £300 – Prasugrel in ACS TA 182 (Oct 2009) • Primary PCI • Stent thrombosis on clopidogrel • Diabetics with ACS – MPI TA73 (Nov 2003) partially updated • Recommended Ix if established CAD and Sx post MI of after revasc – Thrombolysis TA52 (Oct 2002) NICE guidance so far • Technology Appraisals – Drug Eluting Stents TA 152 (July 2008) • DES if artery < 3 mm diameter or lesion > 15mm long • Price difference between BEM and DES <= £300 – Prasugrel in ACS TA 182 (Oct 2009) BCIS dataset • Primary PCI Single lesions • Stent thrombosis on clopidogrel only • Diabetics with ACS – MPI TA73 (Nov 2003) partially updated • Recommended Ix if established CAD and Sx post MI of after revasc – Thrombolysis TA52 (Oct 2002) NICE guidance so far • Technology Appraisals in Progress – Ticagraor for ACS (July 2011) – Bivalirudin for STEMI (?) NICE guidance so far • Clinical Guidelines – Secondary Prevention CG48 (May 2007) • Life style / Rehab / Medication / Ix / Revasc – Chest pain recent onset CG95 (March 2010) • Acute – Mx based on diagnosis, timing of pain, Tn, ECG • Stable CAD likelihood – 10-29% Coro Ca2+ Ix other cause / 64 CT/ angio – 30-60% functional imaging – 61-90% angiography NICE guidance so far • Clinical Guidelines (cont) – UA and NSTEMI CG94 (March 2010) NICE guidance so far • Clinical Guidelines (cont) Grace Score > 3% – UA and NSTEMI CG94 (March 2010) NICE guidance so far • Clinical Guidelines (cont) Grace Score > 3% – UA and NSTEMI CG94 (March 2010) Cath < 96 hrs MDT Consider: 2b-3a / bival NICE • Currently limited • World literature • ESC and AHA Guidelines Stable v ACS Stable angina ↓ Symptoms ACS ↓ Recurrent events ↓ Mortality Outcome Measurement Hierachy Survival Mortality post procedure Risk adjustment Degree of Health or recovery Functional level CCS class / QoL measures Time to recovery and return to normal activity Time to referral / to investigation to Rx / to recovery post Rx / time to return to normal activities / return to work Disutility of care or treatment process MACCE / delay to emergency Rx / pain / access site comps / drug side effects / appropriateness of Rx / medical errors Sustainability of health & nature of recurrences Long term consequences of therapy Maintained freedom from symptoms / need for repeat PCI / staged procedures Stent thrombosis / drug side effects Outcome Measurement Hierachy Survival Mortality post procedure Risk adjustment Degree of Health or recovery Functional level CCS class / QoL measures Time to recovery and return to normal activity Time to referral / to investigation to Rx / to recovery post Rx / time to return to normal activities / return to work treatment process MACCE / delay to emergency Rx / pain / access site comps / drug side effects / appropriateness of Rx / medical errors Stable angina Disutility of care or Sustainability of health & nature of recurrences Long term consequences of therapy Maintained freedom from symptoms / need for repeat PCI / staged procedures Stent thrombosis / drug side effects Outcome Measurement Hierachy Survival Mortality post procedure Risk adjustment Degree of Health or recovery Functional level CCS class / QoL measures Time to recovery and return to normal activity Stable angina Disutility of care or treatment process Sustainability of health & nature of recurrences Long term consequences of therapy Time to referral / to investigation to Rx / to recovery Safety and Symptoms post Rx / time to return to normal activities / return to work MACCE / delay to emergency Rx / pain / access site comps / drug side effects / appropriateness of Rx / medical errors Patient Reported Maintained freedom from symptoms / need for Outcome Measures repeat PCI / staged procedures Stent thrombosis / drug side effects Outcome Measurement Hierachy Survival Mortality post procedure Risk adjustment Degree of Health or recovery Functional level CCS class / QoL measures Time to recovery and return to normal activity Time to referral / to investigation to Rx / to recovery post Rx / time to return to normal activities / return to work Disutility of care or treatment process MACCE / delay to emergency Rx / pain / access site comps / drug side effects / appropriateness of Rx / medical errors Sustainability of health & nature of recurrences Long term consequences of therapy Maintained freedom from symptoms / need for repeat PCI / staged procedures ACS Stent thrombosis / drug side effects Outcome Measurement Hierachy Survival Mortality post procedure Risk adjustment Degree of Health or recovery Functional level CCS class / QoL measures Time to recovery and return to normal activity Time to referral / to investigation to Rx / to recovery post Rx / time to return to normal activities / return to work ACS Disutility of care or treatment process Sustainability of health & nature of recurrences Long term consequences of therapy Safety and Process MACCE / delay to emergency Rx / pain / access site comps / drug side effects / appropriateness of Rx / medical errors Maintained freedom from symptoms / need for repeat PCI / staged procedures Stent thrombosis / drug side effects Key Quality Standards • Safety – Major Averse Events • Risk adjusted Key Quality Standards • Safety – Major Averse Events • Risk adjusted • Elective – Symptoms and Quality of Life • ACS (non-STEMI) – Structure / appropriateness / process • STEMI – Speed UK MINAP Data % McLenachan for NHS Improvement Heart 100 90 80 70 60 50 40 30 20 10 0 Primary PCI Lysis 2008/2 2008/3 2008/4 2009/1 2009/2 2009/3 2009/4 2010/1 PPCI Delay Early presenters High risk 120 Mortality % 100 Late presenters Low risk 80 No Rx PPCI (120 min delay) 60 40 20 0 0 1 2 3 4 Time delay to presentation / Rx PPCI Symptom to Balloon • PPCI, n=1791 De Luca Circ 2004;109:1223 1 year mortality is increased by 7.5% for each 30 minute delay PPCI Door to Balloon Delay McNamara JACC 2006:47;2180 • National Registry of Myocardial Infarction • n=29,222 High risk Anterior DM HR>100 BP<100 Low risk PPCI Door to Balloon Delay McNamara JACC 2006:47;2180 adapted by Nalamothu • NRMI, n=29,222 • Relative Risk per extra 15-Minutes DTB time Compared with DTB of 90 Minutes PPCI Door to Balloon Delay McNamara JACC 2006:47;2180 adapted by Nalamothu • NRMI, n=29,222 • Relative Each Risk per extra 15-Minutes DTB time 15-minute ↓ Door-to-Balloon time Compared with DTB 90 Minuteswith wasofassociated 6.3 fewer deaths per 1000 patients Timings in PPCI Terkelsen JAMA 2010;304:763 Onset of STEMI Patient delay Reperfusion FMC EMS delay 15 min Transport to PCI centre System Delay DTB PPCI System Delay Terkelsen JAMA 2010;304:763 • Western Denmark 2002-2008 • n=6,209 Cum Mortality 30.8% 28.1% 23.3% 15.4% PPCI Mortality v Pre Hospital Δ Sorensen EHJ Dec 2010.1093/eurheartj/ehq437 • Aarhus County Denmark • Urban and Rural implementation of Pre Hospital Diagnosis • System delay • Pre Hospital Diagnosis: • No Pre Hospital Diagnosis: Δ 1 hour 92 min 153 min PPCI Mortality v Pre Hospital Δ Sorensen EHJ Dec 2010.1093/eurheartj/ehq437 • Aarhus County Denmark, System delay 84 122 Δ 38 min 93 167 Δ 74 min PPCI Mortality v Pre Hospital Δ Sorensen EHJ Dec 2010.1093/eurheartj/ehq437 PPCI Mortality v Pre Hospital Δ Sorensen EHJ Dec 2010.1093/eurheartj/ehq437 All cause Mortality median of 4.3 yr FU 31 v 18% Pre-hospital diagnosis HR after adjustment = 0.68 PPCI Call to Balloon time By Admission Route 2009 data: Ludman 250 200 Median CTB min (+/- IQR) 161 150 100 114 106 50 0 Direct IHT ALL PPCI Call to Balloon time By Admission Route 2009 data: Ludman 250 73.9% Direct v 26.1% IHT 200 Median CTB min (+/- IQR) 161 150 100 114 106 50 0 Direct IHT ALL Conclusion • Overview of the politics of ‘Quality Standards’ • Clinical governance and quality of patient care is underpinned by standards • Not measured not assessed • Once measured inevitable change in its value • Many hidden traps to what you measure and how you use it to improve a service The End