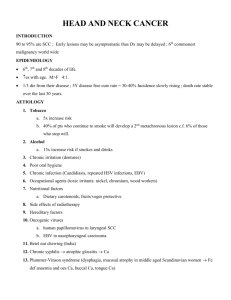
Oral Tongue
advertisement

ANATOMY Upper and Lower Gingiva Hard Palate Lip Oral Tongue Ant 2/3 Buccal Mucosa Floor Of mouth Retromolar Trigone or (Retromolar Gingiva Buccal Mucosa Anatomy Notes Retromolar trigone??:- Apex in line with maxillary tuberosity (behind last molar teeth), the lateral border extend with buccal mucosa, medially it blends with anterior tonsillar pillar, base is formed by the last lower molar and the adjacent gingivolingual sulcus. Other Trigones Trigone of bladder: a triangular region of the wall of the urinary bladder, the three angles corresponding with the orifices of the ureters and urethra; it is an area in which the muscle fibers are closely adherent to the mucosa. Carotid trigone: the triangular area bounded by the posterior belly of the digastric muscle, the sternocleidomastoid muscle, and the anterior midline of the neck. Olfactory trigone: The triangular area of gray matter between the roots of the olfactory tract. Oral Tongue Intrinsic Muscles (speech) • Longitudinal, vertical and transverse Extrinsic Muscles (move body) • Genio, hyo, stylo glossus Four taste qualities, a novel taste, that is referred by the Japanese word umami which means delicious, ‘‘fifth taste’’. Umami taste is found in a diversity of foods (e.g. fish, meat, milk, tomato and some vegetables) and is elicited by monosodium glutamate and certain ribonucleotides. Aging, pregnancy and menopause. Poor dentition and hygiene, alcoholism and/or excessive smoking are common conditions that affect taste. Patients with xerostomia, Sjogren syndrome, vitamin and zinc deficiency liver and kidney disorders, endocrine disorders, diabetes mellitus, psychological disorders, Floor of Mouth A semilunar space extending from the lower alveolar ridge to the undersurface of the tongue. The floor of the mouth overlies the mylohyoid and hyoglossus muscles. Tongue Nerve Supply Lingual (Meneeein). Chorada Tympani. Hypoglossal Nerve. Staging As other Head and Neck but not Nasopharynx. T4a and T4b Usually T4b tumor control probability is very low. Resectability is impossible. Examination Under Anesthesia can be done with the surgeon to assess the disease similar to that of the Cervix. Start by Support Nutritional support. Dental Support. Psychological Support. Speech and Swallowing Consult. Node Story The 5-year cancer-specific survival can be as high as 70% to 90% for patients without lymph node metastasis but drops by half for patients with nodepositive disease. Staging and Node in Head and Neck Cancer N2 disease put patient Stage IVA. N3 disease put patient Stage IVB. Nodes N0 should be treated prophylactically Level I to III. Treatment ORAL CAVITY BASICS - - ASK YOUR SELF THREE QUESTION? Is it small (T1 or T2 ) or large (T3 or T4)?. Is the lesion Central or Lateralized?. Is the Nodes negative or Positive?. Rules The closer to the midline the primary, the greater the risk of bilateral cervical nodal spread. The mucosa of the upper and lower alveolus and hard palate is fixed to the underlying periosteum so invasion of the adjacent bone occurs relatively early making these tumors less suitable for primary radiotherapy Early Lesion Surgical resection: where rim rather segmental resection should be performed. Situations where removal of the bone is required to achieve clear margin. Re-resection should be performed to achieve clear histological margins if the initial resection has positive margins. Lymphatics first echelon upper gingiva lower gingiva hard palate retromolar trigone submandibular and subdigastric nodes submandibular and subdigastric nodes submandibular and subdigastric nodes incidence of clinical nodal positivity at presentation subdigastric nodes Second echelon anterior cervical nodes according to anatomic subsite: - 20 – 30% for gingival and retromolar trigone tumors (with slightly higher risk of nodal disease for lower gingival vs upper gingival tumors) and 10% for hard palate tumors - incidence of clinically positive bilateral nodes rare incidence of occult nodal disease overall: 20% Planned Neck dissection What does it mean? Controversy continue. Lip Cancer In Early stage T1 and T2 surgery results equal to RT. So How to choose? LIP Surgery may be preferred in : - T1 lesion with good functional and cosmetic outcome. - Young patient with outdoor sunlight exposure. - Diffuse superficial lesion of the vermillion, or presence of severe actinic keratosis adjacent to carcinoma. N0 disease In the N0 neck, occult metastases are estimated to occur in 5% to 10% of cases. Therefore, elective neck dissection is not routinely performed in the N0 neck. Neck dissections are generally performed when cervical metastases are clinically or radiographically apparent. Primary Radiotherapy Target Volume: Tumor with a margin Tumor with a margin+first echlon lymph nodes. Tumor with a margin + whole neck . WHEN? LIP What is the likely diagnosis? How would you treat this patient (describe your technique in detail) Oral Tongue Tumor Thickness in Oral Tongue Po demonstrated that tumor thickness in oral tongue carcinomas was the only significant factor that had significant predictive value for subclinical nodal metastasis, local recurrence, and survival in multivariate analysis. External beam alone may not be very successful. Boost using brachytherapy is recommended. Oral Tongue Before external-beam RT, the cancer is photographed and diagrammed to document its extent at the time of the implant. Sometimes, the anterior and posterior borders of the lesion are tattooed with two tiny (1–2 mm) marks. If teeth with metal fillings lie against the tongue or buccal mucosa, a thin layer of gauze (a few millimeters thick) is inserted between the teeth and tongue or buccal mucosa to prevent a high-dose effect secondary to scattered low-energy electrons. Tongue depressor may be different Spot the difference? Advanced Stage Patients with resectable disease who are fit for surgery should have surgical resection with reconstruction. Patients with node positive should be treated with modified radical neck dissection. Elective dissection of the contralateral neck should bee considered if the primary tumor is locally advanced arises form the midline or there are multiple ipsilateral nodal involvement. Advanced Stage Ctn When Concurrent CRT Only Tumor can not be resected. General condition is inadequate. Patient doesn’t wish to go for surgery. Nodal level I to IV should be irradiated. Nodal Disease Patients with N1 disease should be treated by chemoradiotherapy to the primary and node. Patient with N2 or N3 disease should be treated by chemoradiotherapy followed by planned neck dissection. When Chemotherapy is not Suitable Cetuximab with radiotherapy should be considered. Where radiotherapy to be used without chemotherapy or cetuximab, A modified fractionation schedule should be considered. Management Gingival and hard palate cancer – Early (T1 – 2) tumors – Surgery is recommended over radical irradiation due to the high incidence of bone involvement – irradiation risks bone exposure after treatment of the tumor – Very superficial tumors may be treated with radical irradiation – Adjuvant irradiation is added for adverse primary (i.e., high-grade mucoepidermoid or adenoid cystic pathology) or neck pathology – Advanced (T3 – 4) tumors – Surgery and adjuvant irradiation is recommended – Unresectable disease may be treated with adjuvant irradiation followed by attempted resection or hyperfractionated irradiation alone Retromolar trigone cancer – early (T1 – 2) tumors: radical irradiation is recommended over surgery due to more favorable morbidity profile – advanced (T3 – 4) tumors – surgery and adjuvant irradiation is recommended – unresectable disease may be treated with neoadjuvant irradiation followed by attempted resection or hyperfractionated irradiation alone Results gingival cancer – M. D. Anderson (see Leibel, p. 475) treated 48 patients with radical irradiation – survival: 5YOS of 46% – patterns of failure: local control of – 70% for T1 – 2, – 59% for T3, – 29% for T4 hard palate cancer – Memorial (Evans. Am J Surg 142:451. 1981) treated 49 patients with surgery with or without adjuvant irradiation – survival surgery alone: 5YDFS of 75% for stage I, 46% for stage II, 40% for stage III, and 8% for stage IV disease surgery and adjuvant irradiation 5YDFS of 25% for stage IV disease retromolar trigone cancer – M. D. Anderson (Lo. IJROBP 13:969. 1987) treated 159 patients with retromolar trigone and anterior tonsillar pillar tumors with radical irradiation with surgery reserved for salvage – survival: 5YCSS of 83% – patterns of failure: local control – after irradiation: 70% for T1 – 2, 76% for T3, and 60% for T4 – after surgical salvage: < 90% for all T stages Standard ttt T1-T2,N0 Any site (except retromolar trigone) – Surgery alone with staging neck sampling: – Plus adjuvant radiotherapy for high risk situation Microscopic margins <5mm (irrespective of intraoperative revision or additional post-resection sampling of the surgical site) > 1 additional features at primary: – Poorly differentiatied – Peri-neural spread – Angiolympatic invasion Lymph node involvement at pathology: – Extracapsular extension in positive lymph nodes – Multiple lymph nodes – >3 cm lymph nodes Standard ttt. T1-T2 N0 Retromolar trigone Radiotherapy Alone with surgical Salvage 60 Gy in 25 fractions ? 4-6 MV beam quality Homolateral wedge pair (preferable) in lateralised lesions: – – – – – disease limited to 1 cm of palate involved disease limited to 1 cm of tongue involved Parallel opposed as necessary 3 phases (including cord shield where appropriate) Augment posterior neck with electrons after cord Pb where appropriate – Ant or Ant/Post ‘low’ neck parallel opposed (4-6 MV) or hemisplits in unilateral techniques Standard ttt. AnyT, N+ or T3-T4, N0 (except retromolar trigone) M0 – Surgery with neck dissection +/- adjuvant post-operative radiotherapy: Plus adjuvant radiotherapy for high risk situation – Microscopic margins <5mm (irrespective of intra-operative revision or additional post-resection sampling of the surgical site) – > 1 additional features at primary: Poorly differentiatied Peri-neural spread Angiolympatic invasion – Lymph node involvement at pathology: Extracapsular extension in positive lymph nodes Multiple lymph nodes >3 cm lymph nodes – Surgically ‘unstaged’ neck: No surgery to a neck Standard ttt. POST-OPERATIVE XRT 60 Gy in 30 fractions for original site of gross disease where feasible using reducing field techniques 66 Gy in 33 fractions to sites of positive margins 50 Gy to other potentially involved nodal sites Parallel opposed (4-6 MV) or ipsilateral wedge pair for lateralized lesions RADIOTHERAPY ALONE Retromolar Trigone (AnyT, Any N) Primary radiotherapy indicated all cases. Exception is gross bulk disease extending through bone and/or skin involvement where surgery should be considered followed by adjuvant radiotherapy. All Oral cavity T3-T4 or Any N + – Where surgical morbidity at primary site anticipated and considered not appropriate – where patient declines surgery – or neck disease is unresectable and primary not yet treated surgically – Unresectable neck and primary already resected: assess risk to the primary and consider inclusion in plan for neck to administer 70 Gy in 35 fractions with Cisplatin Doses & Beam arrangement Dose fractionation schedules +/chemotherapy – 70 Gy in 35f with Cis-Platin (Intergroup usually) or – 60 Gy in 25f (reserve for frail or ‘patient preference’ declining ‘standard’ treatment) Beam arrangement (technique) – Parallel opposed or angled down wedge pair as necessary with (4-6 MV) – Ant or Ant/Post ‘low’ neck if parallel pair – Augment posterior neck with electrons after cord Pb Targets for non-surgical treatments (any T, any N, M0) -PMH Primary and gross neck node(s): – Phase 1 : 1.5 cm CTV margin (superior: mastoid to inferior: clavicle) – Phase 2 : 1.5 cm CTV margin (cord shield, including custom ‘Step back’ shape for posterior mid-line disease) – Phase 3 : 0.5 cm CTV margin on primary or gross nodes Lymph nodes management Node inclusion: – Zones 2 to 5 included to adjuvant dose (50 Gy in 25 fractions or equivalent) (Leuven/Rotterdam consensus) – Retropharyngeal nodes if extensive other nodal involvement Dose fractionation: – Gross nodes always receive full dose with minimum CTV margins as used for the primary, unless planned surgery is undertaken. – Gross nodes undergoing planned surgery (see below) should receive a minimal ‘microscopic’ dose, depending on the overall dose-fractionation chosen, prior to planned surgery. – Uninvolved node regions within the risk zones should be treated to a ‘microscopic’ dose depending on the overall dose-fractionation chosen. Radiotherapy technique External Beam alone??? Organ Preservation You still can Try CRT if organ preservation is required. (provided salvage surgery may still be an option. e.g. patient reliable for good follow-up. Surgeon reliable for good surgery. Famous Laryngeal preservation trials: -Veterans Affairs (larynx neoadjuvant), EORTC (Hypopharynx neoadjuvant), (RTOG 91-11 larynx Concurrent CRT value). -Urba et al JCO 2006(NEW is the use of concurrent CRT if good response to the neoadjuvant treatment. Patient Preparation Dental. Nutritional. Psychological. Council. Immobilization. Simulation. Immobilzation Max. Extension still possible for easily shielding of the oral cavity. Tongue bite? What was the question? Portal Arrangements Opposed –lateral photon fields, with the patient immobilized in supine position are used for treatment of most cancers : oral cavity, Larynx, pharynx. Superior border: Determined by the location of the known disease and likely spread pattern. In General: Either it will be 1- At the base of skull when we want to include the retropharyngeal node, e.g. Hypopharynx. Superior Nasopharynx Hypopharynx Oropharynx Oral cavity: Larynx border: Above skull base. because the primary at skull base. Skull base? Retropharyngeal nodesz Skull base? Primary at skull base. Do you want lymph node? So skull base/If not take only a margin (1 to 2 cm). Glottic? Above the glottis. Supraglottic? Lymph nodes so skull base. Subgltic (very rare) only margin above the larynx. Glottic with extensive supra? Skull base. Eisbruch et al. established dose thresholds for the parotid gland: mean dose ≤24 Gy and ≤ 26 Gy for unstimulated and stimulated salivary flow, respectively. Also, partial volume thresholds were established: 67%, 45%, 24% of the parotid gland volume receiving ≥ 15 Gy, ≥ 30 Gy, ≥ 45 Gy, respectively. They observed that if the dose to the parotid glands exceeds (one or more of) these thresholds, Parotid salivary flow would significantly decrease Oropharynx Base of Tongue. Tonsil and Faucial arche. Soft Palate.