Titel: PowerPoint sjabloon voor posters in Vumc huisstijl
advertisement
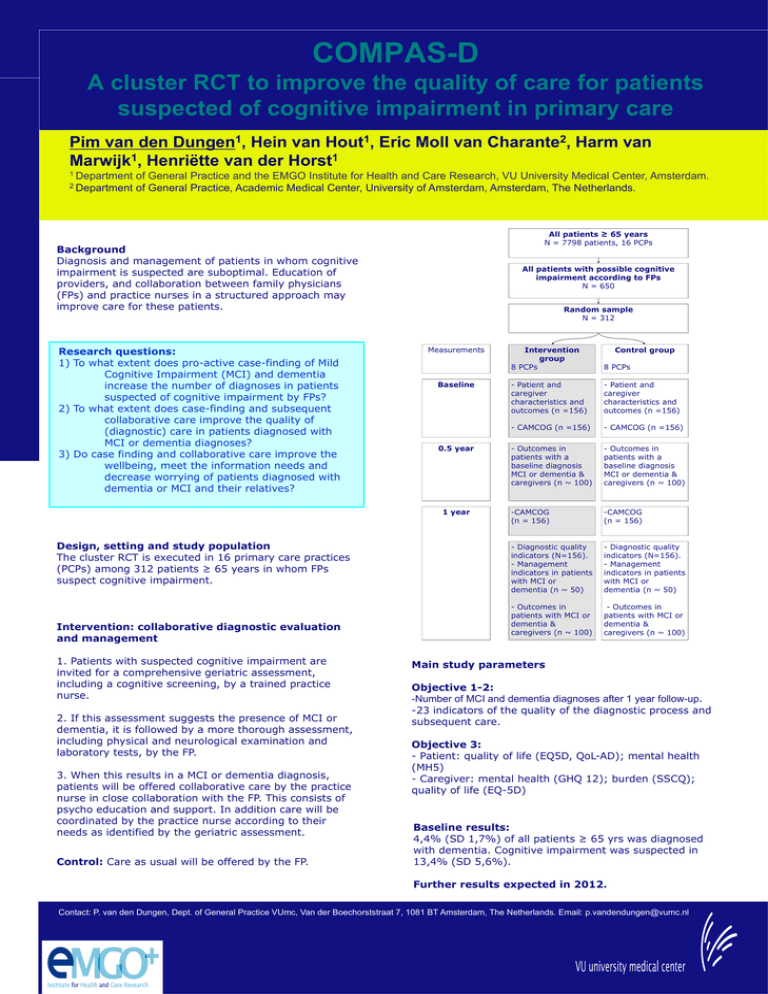
COMPAS-D A cluster RCT to improve the quality of care for patients suspected of cognitive impairment in primary care Pim van den Dungen1, Hein van Hout1, Eric Moll van Charante2, Harm van 1 1 Marwijk , Henriëtte van der Horst 1 Department of General Practice and the EMGO Institute for Health and Care Research, VU University Medical Center, Amsterdam. 2 Department of General Practice, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands. All patients ≥ 65 years N = 7798 patients, 16 PCPs Background Diagnosis and management of patients in whom cognitive impairment is suspected are suboptimal. Education of providers, and collaboration between family physicians (FPs) and practice nurses in a structured approach may improve care for these patients. Research questions: 1) To what extent does pro-active case-finding of Mild Cognitive Impairment (MCI) and dementia increase the number of diagnoses in patients suspected of cognitive impairment by FPs? 2) To what extent does case-finding and subsequent collaborative care improve the quality of (diagnostic) care in patients diagnosed with MCI or dementia diagnoses? 3) Do case finding and collaborative care improve the wellbeing, meet the information needs and decrease worrying of patients diagnosed with dementia or MCI and their relatives? All patients with possible cognitive impairment according to FPs N = 650 Random sample N = 312 Measurements Baseline 0.5 year 1 year Design, setting and study population The cluster RCT is executed in 16 primary care practices (PCPs) among 312 patients ≥ 65 years in whom FPs suspect cognitive impairment. Intervention: collaborative diagnostic evaluation and management 1. Patients with suspected cognitive impairment are invited for a comprehensive geriatric assessment, including a cognitive screening, by a trained practice nurse. 2. If this assessment suggests the presence of MCI or dementia, it is followed by a more thorough assessment, including physical and neurological examination and laboratory tests, by the FP. 3. When this results in a MCI or dementia diagnosis, patients will be offered collaborative care by the practice nurse in close collaboration with the FP. This consists of psycho education and support. In addition care will be coordinated by the practice nurse according to their needs as identified by the geriatric assessment. Control: Care as usual will be offered by the FP. Intervention group 8 PCPs Control group 8 PCPs - Patient and caregiver characteristics and outcomes (n =156) - Patient and caregiver characteristics and outcomes (n =156) - CAMCOG (n =156) - CAMCOG (n =156) - Outcomes in patients with a baseline diagnosis MCI or dementia & caregivers (n ~ 100) - Outcomes in patients with a baseline diagnosis MCI or dementia & caregivers (n ~ 100) -CAMCOG (n = 156) -CAMCOG (n = 156) - Diagnostic quality indicators (N=156). - Management indicators in patients with MCI or dementia (n ~ 50) - Diagnostic quality indicators (N=156). - Management indicators in patients with MCI or dementia (n ~ 50) - Outcomes in patients with MCI or dementia & caregivers (n ~ 100) - Outcomes in patients with MCI or dementia & caregivers (n ~ 100) Main study parameters Objective 1-2: -Number of MCI and dementia diagnoses after 1 year follow-up. -23 indicators of the quality of the diagnostic process and subsequent care. Objective 3: - Patient: quality of life (EQ5D, QoL-AD); mental health (MH5) - Caregiver: mental health (GHQ 12); burden (SSCQ); quality of life (EQ-5D) Baseline results: 4,4% (SD 1,7%) of all patients ≥ 65 yrs was diagnosed with dementia. Cognitive impairment was suspected in 13,4% (SD 5,6%). Further results expected in 2012. Contact: P. van den Dungen, Dept. of General Practice VUmc, Van der Boechorststraat 7, 1081 BT Amsterdam, The Netherlands. Email: p.vandendungen@vumc.nl