Stroke
by
Ann Van Eerden
April, 2011
Navigation of this Tutorial
Click to advance to the next slide
Click to go to the previous slide
Click to return to Table of Contents
Click to return to the last slide you viewed
Click on underlined words and blue
boxes throughout the tutorial for more
information.
Learning Outcomes
Learner will define CVA
Learner will distinguish the causes of CVA
Learner will state risk factors for CVA
Learner will recognize clinical manifestations of
a stroke
Learner will identify the nursing diagnosis “at
risk for falls.”
Learner will discern conditions related to risk for
falls
Learner will develop nursing outcomes and
interventions
Table of Contents
Welcome to Your Clinical
What is a Stroke?
Causes of Stroke
Risk Factors
Clinical Manifestations
“At Risk for Falls”
Conditions Related to “At Risk for
Falls”
References
Welcome to the first day at your new clinical
site!
You learn that the patient you have been
assigned for the day has a medical diagnosis
of stroke, more specifically, a left sided
cerebrovascular accident. Would you like to
continue?
Yes!
No, I think I am
going to drop
this class.
Before you make that decision,
please stay for awhile; you’ll feel
much better after this tutorial!
Your instructor greets you and introduces
you to the night nurse who immediately
begins giving you report. This is your first
time on a medical unit. Your mind is
racing; you are trying to recall everything
that you remember about stroke, and
nothing comes to mind. Would you like a
review?
Yes, please!
No thanks, I’ve
decided to change
my major.
Ha! Ha! But, before you make that
official, you might feel better if you
take a few minutes to review stroke
with this tutorial.
A stroke is a BRAIN ATTACK! It means that there is
an interrupted flow of blood to the brain.
What do you think might cause this interruption?
A Thrombus
You are correct! Is
there anything
else?
An Embolism
You are correct! Is
there anything
else?
A Hemorrhage
You are correct! Is
there anything
else?
A thrombus is the most common cause of
stroke. It accounts for 60% of all strokes.
It occurs more often in men.
The onset is usually during or after sleep.
The signs and symptoms develop slowly.
(Lewis, 2004, p. 1528)
An embolic stroke occurs when an
embolus occludes a cerebral artery.
It occurs more often in men.
The onset is rapid.
It is a single event.
(Lewis, 2004, p. 1529)
(Used with permission of Emily Gillis)
Hemorrhagic strokes are either an intracerebral
hemorrhage or a subarachnoid hemorrhage.
An intracerebral hemorrhage has a sudden onset and
a very poor prognosis.
A subarachnoid hemorrhage is caused by an
aneurysm and often follows
strenuous activity.
(Lewis, 2004, p. 1529)
(Used with permission of Emily Gillis)
Okay! The night nurse has left and its time
for you to take over. Mr. C. V. Accident is
still sleeping and a nursing assistant offers
to get his breakfast tray, so you have time to
get organized. Let’s use the nursing
process.
Do you remember the process?
Click on each box below for a review.
ASSESS
DIAGNOSE
PLAN
IMPLEMENT
EVALUATE
Mr. C.V. Accident’s Chart
Mr. C.V. Accident is a 72 year old
African- American with a history of
hypertension. He is overweight, does not
exercise, and smokes one pack of
cigarettes per day. His wife died last year
and since her death his diet consists
primarily of fast food.
There are a number of risk factors
that contribute to stroke. Some are
modifiable, others are not.
Click here to review the modifiable
risk factors.
Click here to review the nonmodifiable risk factors.
Modifiable Risk Factors
Atrial fibrillation
Carotid stenosis
Cigarette smoking
Diabetes
Heavy alcohol consumption
Hypercoagulability
Hyperlipidemia
Hypertension
Obesity
Oral contraceptive use
Physical inactivity
Sickle cell disease
(Lewis, 2004, p. 1526)
Non-Modifiable Risk
Factors
Age
Gender
Race
Family history
Prior stroke, TIA, or heart
attack
(Lewis, 2004, p. 1525)
Hypertension is the most important
modifiable risk factor. Hypertension is a
sustained elevation in blood pressure.
It is defined as a systolic blood pressure equal
to or greater than 140 mm Hg OR a diastolic
blood pressure equal to or greater than 90 mm
Hg for extended periods of time.
Would you like to review what happens with
hypertension? (Lewis, 2004, p.779)
Yes
No thanks.
Hypertension Flow Chart
What does high
blood pressure do
to the blood
vessels?
Increased Blood
Pressure
Injury to vessels
What happens to
injured vessels?
Do you remember
what happens to the
inflamed vessels?
And what does
atherosclerosis
lead to?
Inflammation
Plaque develops and leads to
atherosclerosis
Risk of thrombus and emboli
and INCREASED RISK FOR
STROKE
Atherosclerosis is often
described as hardening and
thickening of the arteries.
How does this lead to stroke?
Lipids in the arteries develop into
PLAQUE
Plaque leads to narrowing and
thickening of the arteries
PLAQUE
may break off and
occlude the artery and
ultimately cause
STROKE!
PLAQUE
narrows arteries and
can lead to
hypertension and
ultimately STROKE!
Other factors affect these processes.
They are:
Aging
Genetics
Inflammation
Stress
Contribution of
Aging
Aging
What does aging do to
the aorta and arteries?
What does this do to
blood pressure?
Aorta and arteries
decrease in elasticity
Increase in systolic
blood pressure
Increased risk for
stroke
Contribution of Genetics
What do the sickle
cells adhere to?
What happens to
the vessel lining?
Sickle cell disease
Sickles adhere to
endothelium
Vessel lining becomes
inflamed
What else do these
sickle cells promote?
What is the risk
associated with
increased coagulation?
Increased
coagulation
Increased risk of
thrombus
Increased risk for
stroke
Contribution of Inflammation
Do you remember what
happens to an injured
cell?
Injury to Endothelial
Cell
Inflammatory cells
migrate to injury
What do these cells do?
Contribute to development
of atherosclerotic plaques
What is this plaque
build up called in the
vessels?
What modifiable risk
factor does this
contribute to?
Atherosclerosis
Hypertension
Increased risk for
stroke
Contribution of the Stress Response
What does stress do
to the sympathetic
nervous system?
What happens to
your blood pressure?
Do you remember
what this does to the
cells?
And this leads to
hardening of the
arteries, also known
as?
Do you remember
which risk factor
develops because of
this?
Stress
Sympathetic Nervous System
releases epinephrine and
norepinephrine
Increased blood pressure
and increased mechanical
stress
Endothelial Cell
Injury
Atherosclerosis
Hypertension
Increased risk for
stroke
What Are Modifiable Risk Factors that
Contributed to Mr. C.V. Accident’s Stroke?
Age
No, this is not
modifiable.
Hypertension
Yes, this is
correct.
Race
No, race is not
modifiable.
Weight
Yes, this is
modifiable.
Activity Level
Yes, this is
modifiable.
Family History
No, this is not
modifiable.
Diet
Yes, this is
modifiable.
Sex
No, this is not
modifiable.
Height
This is not a
risk factor.
Profession
This is not a
risk factor.
Smoking
Yes, this is
modifiable.
Hair Color
This is not a
risk factor.
Mr. C. V. Accident’s history indicates that
while he was at church with his daughter, the
right side of his face started drooping.
Suddenly, he was unable to lift his right arm,
and his speech became slurred.
His daughter acted quickly and
immediately called 9-1-1.
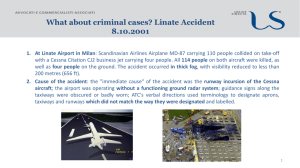
Mr. C.V. Accident had an ischemic stroke.
Because he got to the hospital in LESS THAN
THREE HOURS from the onset of his
symptoms and a CT scan excluded the
diagnosis of hemorrhagic stroke,
Mr. C. V. Accident received recombinant
tissue-type plasminogen activator (tPA), a
thrombolytic agent.
How does tPA work?
Here is how tPA works:
Tissue plasminogen activator (tPA) targets the
thrombus and catalyzes the conversion of
plasminogen to plasmin resulting in thrombolysis.
Mr. C.V. Accident is diagnosed with a left sided cerebral accident. This means
that the left side of his brain has been damaged and that the right side of his body
will be impaired. Damage to the right side of his brain would result in impairment
to the left side of his body.
(Used with permission of Emily Gillis)
In your assessment, what are some of the clinical
manifestations you might see with Mr. C.V.
Accident? (Remember he has a left sided CVA.)
Right sided
hemiplegia
Yes, you are
correct!
Left sided
weakness
No, not with a
left sided CVA.
Impaired
concept of time
No, this is true
for right sided
strokes.
Impulsivity
No, this is true
for right sided
strokes.
Homonymous
hemianopsia
Yes, this is the loss of
the visual field at the
vertical midline of both
eyes and is true of all
strokes!
Right sided
neglect
Yes, this is true
for left sided
brain damage.
Impaired
speech and
language
Yes, this is true!
Difficulty in
learning new
information
Yes, this is true
for any stroke!
Your assessment is complete,
now, its time for a nursing
diagnoses for Mr. C.V.
Accident.
Do you think Mr. C.V. Accident
is at risk for falls?
YES
MAYBE
NO
Falls are one of the most common
medical complications after stroke.
7% incidence first week after stroke
25%-37% incidence between one and six months
post-stroke
40%-50% incidence six to twelve months after
stroke
55%-73% incidence one year after stroke
(Verheyden, 2010)
(Microsoft Clip Art)
So, Mr. C.V. Accident is
AT RISK FOR FALLS related to
Balance Impairment
Hemi-neglect
Self-care deficit
Cognitive impairment
Hemiparesis
Hemianopsia
At risk for falls related to balance
impairment
Outcome: Mr. C.V. Accident will remain free
from falls
Which nursing intervention would you use?
Encourage Mr. C.V. Accident to use walking aids when
ambulating.
Yes! You are correct!
Monitor Mr. C.V. Accident’s fluid intake.
This may be valuable for other reasons, but it will not
decrease the risk of falls related to balance impairment.
(Microsoft Clip Art)
At risk for falls related to hemi-neglect
Outcome: Mr. C.V. Accident will remain free
from falls
Which nursing intervention would you use?
Offer Mr. C.V. Accident frequent reminders to be aware of his
left side.
You are correct!
Assess Mr. C.V. Accident’s pain level.
While this may be a great intervention if Mr. C.V. Accident
exhibits signs of pain, this will not help him address his hemineglect.
At risk for falls related to self care
deficit
Outcome: Mr. C.V. Accident will remain free
from falls
Which nursing intervention would you use?
Monitor Mr. C.V. Accident’s vital signs every four hours.
While vital signs are important, this will not keep Mr. C.V.
Accident from falling while dressing himself.
Assist Mr. C.V. Accident with dressing.
Hooray! You are correct!
(Microsoft Clip Art)
At risk for falls related to cognitive
impairment
Outcome: Mr. C.V. Accident will remain free
from falls
Which nursing intervention would you use?
Orient Mr. C.V. Accident to his environment. Include the location and
way to use his call button.
Correct!
Assess neurological status with the Glasgow coma scale.
This is appropriate if Mr. C.V. Accident exhibits an altered level of
consciousness, but it will not keep him free from falls.
(Microsoft Clip Art)
At risk for falls related to hemiparesis
Outcome: Mr. C.V. Accident will remain free
from falls
Which nursing intervention would you use?
Perform neurological assessment every four hours.
Sorry! This will not prevent Mr. C.V. Accident from falling.
Encourage Mr. C.V. Accident to use assistive devices for walking.
Hooray! You are correct! If he uses his assistive devices, the risk for
falls will be decreased.
(Microsoft Clip Art)
At risk for falls related to hemianopsia
Outcome: Mr. C.V. Accident will remain free
from falls
Which nursing intervention would you use?
Place items in Mr. C.V. Accident’s field of vision.
Correct! You are doing a great job!
Encourage Mr. C.V. Accident to increase his fluid intake.
While fluids are important, this will not prevent falls.
Click here to
help Mr. C.V.
Accident find
the knife.
(Microsoft Clip Art)
Wow! Mr. C.V. Accident’s care plan
is done! Its time to implement the
nursing interventions, and evaluate
them as the day goes on. This first
clinical is almost over and it is going
very well!
References
Centers for Disease Control and Prevention (n.d.). Stroke Facts.
Retrieved from http://www.cdc.gov/stroke/facts.htmm.
Lewis, S.M., Heitkemper, M. M., & Dirksen, S. Medical surgical
nursing: assessment and management of clinical problems, ed 6, St.
Louis, 2004, Mosby.
Microsoft Clip Art
Porth, C.M., 2005. Pathophysiology, 7th edition. Lippincott.
Verheyden, G., Weerdesteyn, V., Pickering, R., Hyndman, D., Lennon,
S., Geurts, A., & Ashburn, A. (2010). Interventions for preventing falls
in people after stroke.