From Zero to FLS: Implementation & Beyond
advertisement

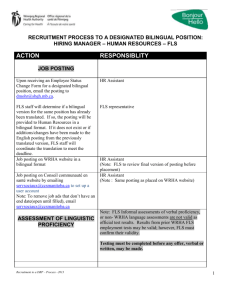
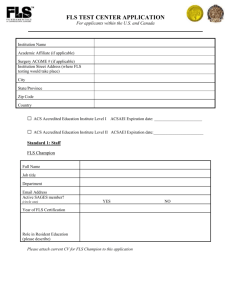
From Zero to FLS: Implementation & Beyond National Osteoporosis Society FLS Education Programme October 2010 Size Matters! Determinants of the scale of your service Previous fracture The FLS’ target population - which fracture groups? - what age group? New Fracture Non-vertebral & Vertebral Non-vertebral & Vertebral Size Matters! Determinants of the scale of your service Previous fracture ~650 new non-vertebral fractures & ~120 new vertebral fractures age 50+ per 100K, per year New Fracture Non-vertebral & Vertebral Non-vertebral & Vertebral NEW FRACTURE PRESENTING TO A&E / ORTHO / TRAUMA FALLS RISK ASSESSMENT NEW RADIOLOGY REPORT OF FRACTURE EXERCISE CLASSES Rx FOR FRACTURE 2Y PREVENTION PRESCRIPTION ISSUED BY GP McLellan et al. Osteporos Int 2003;14:1028–1034 PREVIOUS FRACTURE EDUCATION PROGRAMME From Zero to FLS: Implementation & Beyond Project Management From Zero to FLS: Implementation & Beyond The first steps • Appointment of project management team & Chair Membership of FLS implementation project team Number Post x2 Local champion / lead clinician x1 Chair GG&CHB Osteoporosis Subgroup (clinician) x3-4 Other HB lead clinician & secondary care clinicians from involved sites x1-3 CHP GP lead x2 Osteoporosis Nurse Specialists x1 General Manager – Medical Services x1 GG&C osteoporosis exercise service lead physio x1 Superintendent Radiographer x1 Assistant General Manager, Radiology x1 Consultant radiologist (DXA) – local imaging lead x1 Estates manager x1 NOS patient representative From Zero to FLS: Implementation & Beyond The first steps • Appointment of project management team & Chair • Redefine & agree with providers of funding remit of group & scope of service Remit of group & scope of planned service 1. To roll out an FLS, to provide systematic post-fracture assessment to all men & women age 50+ with new fracture presentations or with new report of vertebral fracture or with previous fracture age 50+ 2. To ensure equitable access of all relevant patients in the region 3. To implement these services within the constraints of the proposed funding 4. Case-finding for new fracture presentations & for new reports of vertebral fracture – by the FLS ONS Remit of group & scope of planned service 5. Case-finding for previous fractures – by primary care 6. Post-fracture, risk assessment based on one-stop consultation with FLS-ONS incorporating DXA, where appropriate 7. All episodes of FLS-patient care recorded in database 8. To provide this for population of x over y sites and covering fracture patients from z hospitals From Zero to FLS: Implementation & Beyond The first steps • Appointment of project management team & Chair • Redefine & agree with providers of funding remit of group & scope of service • Work breakdown From Zero to FLS: Implementation & Beyond Project Management DXA Work Breakdown Personnel Logistics From Zero to FLS: Implementation & Beyond Project Management DXA Work Breakdown Personnel Logistics From Zero to FLS: Implementation & Beyond The first steps • Appointment of project management team & chair • Redefine & agree with providers of funding remit of group & scope of service • Work breakdown • Schedule work & establish timeline for delivery of service Dec 2007 ID Task Name Start Finish 2/12 9/12 16/12 23/12 30/12 6/1 1 Scope & Remit – Group Membership Jan 2008 Feb 2008 Mar 2008 Apr 2008 May 2008 Jun 2008 Jul 2008 Duration 05/12/2007 09/01/2008 5.2w 2 WB – Personnel Appointments 05/12/2007 15/04/2008 19w 3 WB – DXA procurement to delivery 05/12/2007 14/03/2008 14.6w 4 WB - Exercise class infrastructure 05/12/2007 07/05/2008 22.2w 5 WB - protocols 05/12/2007 07/05/2008 22.2w 6 WB – Induction – training 05/12/2007 04/06/2008 26.2w 7 WB – Communications incl website 27/02/2008 30/05/2008 13.6w 8 Service launch 05/12/2007 01/08/2008 34.6w 13/1 20/1 27/1 3/2 10/2 17/2 24/2 2/3 9/3 16/3 23/3 30/3 6/4 13/4 20/4 27/4 4/5 11/5 18/5 25/5 1/6 8/6 15/6 22/6 29/6 6/7 13/7 20/7 27/7 From Zero to FLS: Implementation & Beyond Project Management DXA Work Breakdown Personnel Logistics What do you need to provide a DXA for a FLS service ? • Space for DXA (may require building works!) • DXA scanner/s – DXA (VFA) site visit to inform choice – DXA procurement • Radiographer/s • ONS clinic space - near DXA • Database - reporting system • Patient transport issues From Zero to FLS: Implementation & Beyond Project Management DXA Work Breakdown Personnel Logistics Personnel • Overview – – – – Banding & Grades of Staff Job descriptions Appointments processes - job descriptions - adverts – interviews Consultant Sessions • How are Consultant sessions best deployed? • Osteoporosis Nurse Specialist/s – Band 6/7 Osteoporosis Nurse Specialist – ONS line management – ONS where & how will they work? Personnel • Administration & Clerical Staff – Band 3 A&C • Physiotherapist/s for exercise services – Band 6 Physiotherapist • Radiographer/s – Band 6 Radiographers From Zero to FLS: Implementation & Beyond Project Management DXA Work Breakdown Personnel Logistics Logistics • Pathways of care – New fracture presentations in which hospitals & FLS in which centres – New reports of vertebral fractures in which hospitals & FLS in which centres – Past fractures from across region referred to which centres • Protocol development • Access to Mineral Metabolism clinic for those who don’t fit with management protocols • Liaison re exercise classes • Liaison with falls service Logistics • Communication within secondary care & with GPs • Standardisation of forms • Website development to facilitate communication • Patient education materials • Patient education classes • ? Nurse telephone follow up (? Telephone BPR tariff) • Training & induction • Launch meeting What do you need to provide exercise classes? • Access to health service physio gym – Identify exercise class locations • Access to leisure centre gyms – Identify exercise class locations • Patient transport issues If at first you don’t succeed… If at first you don’t succeed… you’ve failed! Pathway to success… & it will be incremental! What are we trying to accomplish? How will we know that a change is an improvement? What changes can we make to effect improvement? Plan Do Act Study Pathway to success… & it will be incremental! PDSA & the Evolution of the Glasgow FLS for new fractures Cycle 1 Objective 1 Objective 2 Case-finding all new fx F&M age 50+ by GP Fracture risk assessment by ONS at one-stop clinic with DXA Outcomes audit Only 5% wrist fx & 11% hip fx identified / referred for assessment Essential change Case-finding must be by ONS in secondary care PDSA & the Evolution of the Glasgow FLS for new fractures Objective 1 Objective 2 Cycle 1 Cycle 2 Case-finding all new fx F&M age 50+ by GP Case-finding all new fx F&M age 50+ by ONS in secondary care Fracture risk assessment by ONS at one-stop clinic with DXA Outcomes audit Only 5% wrist fx & 11% hip fx identified / referred for assessment ~all fx patients identified & assessed – but only 4% of fx were vertebral Essential change Case-finding must be by ONS in secondary care Need for new approach to identify vertebral fx PDSA & the Evolution of the Glasgow FLS for new fractures Objective 1 Objective 2 Cycle 1 Cycle 2 Cycle 3 Case-finding all new fx F&M age 50+ by GP Case-finding all new fx F&M age 50+ by ONS in secondary care Case-finding all new fx F&M age 50+ by ONS in secondary care & all new radiology reports of vertebral fx Fracture risk assessment by ONS at one-stop clinic with DXA Outcomes audit Only 5% wrist fx & 11% hip fx identified / referred for assessment ~all fx patients identified & assessed – but only 4% of fx were vertebral Essential change Case-finding must be by ONS in secondary care Need for new approach to identify vertebral fx ~all fx patients identified & assessed – now 12% of fx are new vertebral fx ‘The only place success comes before work is in a dictionary!’