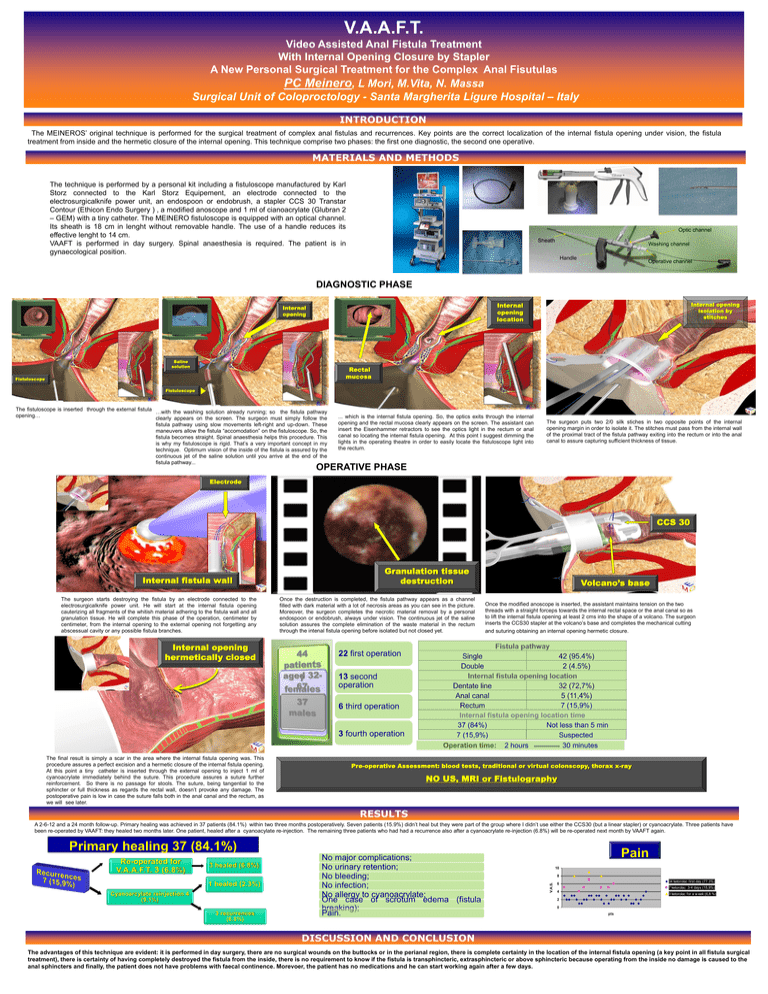
V.A.A.F.T.
Video Assisted Anal Fistula Treatment
With Internal Opening Closure by Stapler
A New Personal Surgical Treatment for the Complex Anal Fisutulas
PC Meinero, L Mori, M.Vita, N. Massa
Surgical Unit of Coloproctology - Santa Margherita Ligure Hospital – Italy
INTRODUCTION
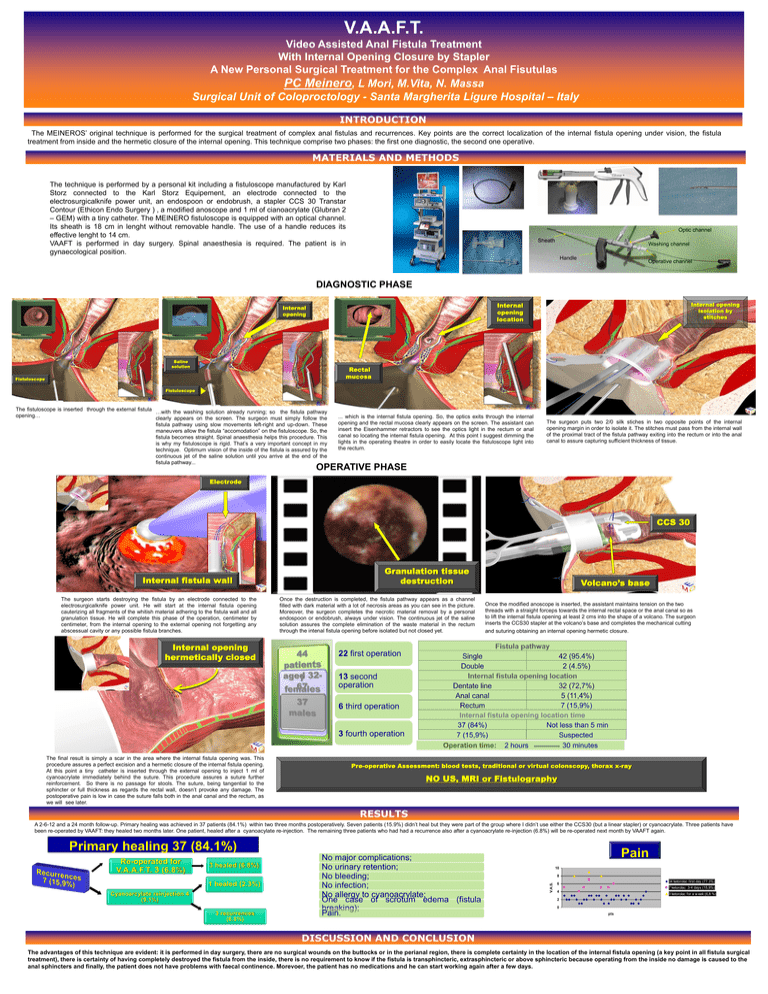
The MEINEROS’ original technique is performed for the surgical treatment of complex anal fistulas and recurrences. Key points are the correct localization of the internal fistula opening under vision, the fistula
treatment from inside and the hermetic closure of the internal opening. This technique comprise two phases: the first one diagnostic, the second one operative.
MATERIALS AND METHODS
The technique is performed by a personal kit including a fistuloscope manufactured by Karl
Storz connected to the Karl Storz Equipement, an electrode connected to the
electrosurgicalknife power unit, an endospoon or endobrush, a stapler CCS 30 Transtar
Contour (Ethicon Endo Surgery ) , a modified anoscope and 1 ml of cianoacrylate (Glubran 2
– GEM) with a tiny catheter. The MEINERO fistuloscope is equipped with an optical channel.
Its sheath is 18 cm in lenght without removable handle. The use of a handle reduces its
effective lenght to 14 cm.
VAAFT is performed in day surgery. Spinal anaesthesia is required. The patient is in
gynaecological position.
Optic channel
Sheath
Washing channel
Handle
Operative channel
DIAGNOSTIC PHASE
Internal opening
isolation by
stitches
Internal
opening
location
Internal
opening
Saline
solution
Rectal
mucosa
Fistuloscope
Fistuloscope
The fistuloscope is inserted through the external fistula …with the washing solution already running; so the fistula pathway
opening…
clearly appears on the screen. The surgeon must simply follow the
fistula pathway using slow movements left-right and up-down. These
maneuvers allow the fistula “accomodation” on the fistuloscope. So, the
fistula becomes straight. Spinal anaesthesia helps this procedure. This
is why my fistuloscope is rigid. That’s a very important concept in my
technique. Optimum vision of the inside of the fistula is assured by the
continuous jet of the saline solution until you arrive at the end of the
fistula pathway...
... which is the internal fistula opening. So, the optics exits through the internal
opening and the rectal mucosa clearly appears on the screen. The assistant can
insert the Eisenhammer retractors to see the optics light in the rectum or anal
canal so locating the internal fistula opening. At this point I suggest dimming the
lights in the operating theatre in order to easily locate the fistuloscope light into
the rectum.
The surgeon puts two 2/0 silk stiches in two opposite points of the internal
opening margin in order to isolate it. The stitches must pass from the internal wall
of the proximal tract of the fistula pathway exiting into the rectum or into the anal
canal to assure capturing sufficient thickness of tissue.
OPERATIVE PHASE
Electrode
CCS 30
Granulation tissue
destruction
Internal fistula wall
The surgeon starts destroying the fistula by an electrode connected to the
electrosurgicalknife power unit. He will start at the internal fistula opening
cauterizing all fragments of the whitish material adhering to the fistula wall and all
granulation tissue. He will complete this phase of the operation, centimeter by
centimeter, from the internal opening to the external opening not forgetting any
abscessual cavity or any possible fistula branches.
Internal opening
hermetically closed
Once the destruction is completed, the fistula pathway appears as a channel
filled with dark material with a lot of necrosis areas as you can see in the picture.
Moreover, the surgeon completes the necrotic material removal by a personal
endospoon or endobrush, always under vision. The continuous jet of the saline
solution assures the complete elimination of the waste material in the rectum
through the intenal fistula opening before isolated but not closed yet.
Volcano’s base
Once the modified anoscope is inserted, the assistant maintains tension on the two
threads with a straight forceps towards the internal rectal space or the anal canal so as
to lift the internal fistula opening at least 2 cms into the shape of a volcano. The surgeon
inserts the CCS30 stapler at the volcano’s base and completes the mechanical cutting
and suturing obtaining an internal opening hermetic closure.
22 first operation
13 second
operation
6 third operation
3 fourth operation
The final result is simply a scar in the area where the internal fistula opening was. This
procedure assures a perfect excision and a hermetic closure of the internal fistula opening.
At this point a tiny catheter is inserted through the external opening to inject 1 ml of
cyanoacrylate immediately behind the suture. This procedure assures a suture further
reinforcement. So there is no passage for stools. The suture, being tangential to the
sphincter or full thickness as regards the rectal wall, doesn’t provoke any damage. The
postoperative pain is low in case the suture falls both in the anal canal and the rectum, as
we will see later.
7 (15,9%)
Internal fistula opening location time
37 (84%)
Not less than 5 min
7 (15,9%)
Suspected
Operation time: 2 hours
30 minutes
Pre-operative Assessment: blood tests, traditional or virtual colonscopy, thorax x-ray
NO US, MRI or Fistulography
RESULTS
A 2-6-12 and a 24 month follow-up. Primary healing was achieved in 37 patients (84.1%) within two three months postoperatively. Seven patients (15.9%) didn’t heal but they were part of the group where I didn’t use either the CCS30 (but a linear stapler) or cyanoacrylate. Three patients have
been re-operated by VAAFT: they healed two months later. One patient, healed after a cyanoacylate re-injection. The remaining three patients who had had a recurrence also after a cyanoacrylate re-injection (6.8%) will be re-operated next month by VAAFT again.
Primary healing 37 (84.1%)
3 healed (6.8%)
1 healed (2.3%)
Cyanoarcylate reinjection 4
(9.1%)
3 recurrences
(6.8%)
Pain
10
8
V.A.S.
Re-operated for
V.A.A.F.T. 3 (6.8%)
No major complications;
No urinary retention;
No bleeding;
No infection;
No allergy to cyanoacrylate;
One case of scrotum edema (fistula
breaking);
Pain.
34 ketorolac first day (77.3%)
6
7 ketorolac 3-4 days (15,9%)
4
3 ketorolac for a w eek (6,8.%)
2
0
pts
DISCUSSION AND CONCLUSION
The advantages of this technique are evident: it is performed in day surgery, there are no surgical wounds on the buttocks or in the perianal region, there is complete certainty in the location of the internal fistula opening (a key point in all fistula surgical
treatment), there is certainty of having completely destroyed the fistula from the inside, there is no requirement to know if the fistula is transphincteric, extrasphincteric or above sphincteric because operating from the inside no damage is caused to the
anal sphincters and finally, the patient does not have problems with faecal continence. Morevoer, the patient has no medications and he can start working again after a few days.