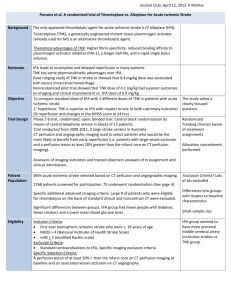
t. P.A. total Plasminogen Activator
advertisement

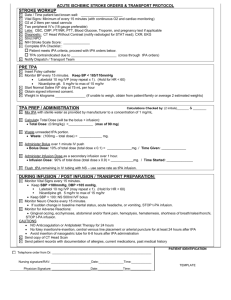
t. P.A. tissue Plasminogen Activator Presented by: Kelly Banasky, RN, BSN GCH Emergency Services Educator What is tPA? • tPA is a thrombolytic drug also known as Alteplase or Activase • Used for AMI, PE, Acute Ischemic Stroke (AIS) • The dosage for AIS is less than the dosing for AMI or PE • tPA disrupts the integrity of a thrombus, plaque or emboli within a blood vessel • It is the ONLY thrombolytic agent approved by the FDA for the treatment of AIS • Other Thrombolytics had unacceptably high hemorrhage rates or were not tested extensively to establish risk versus benefits. How it works • Upon administration: • • • • Binds the fibrin in a clot Converts the trapped plasminogen to plasmin Initiates fibrinolysis Limited systemic proteolysis (breakdown into smaller fragments) • Has a small window of time in which it can be administered and requires close monitoring post administration. • Within 3 hours of symptom onset • In some cases, based on criteria, a 3 to 4.5 hour window is possible. Eligibility for inclusion • Patients with a Negative for Hemorrhage head CT scan may receive tPA ONLY IF the following conditions are met: • Must be 18 years of age or older • Have a clinical diagnosis of stroke with a measurable deficit • Onset of symptoms: • < (less than) 3 hours • If > (greater than) 3 hours, but < (less than) 4 ½ hours if eligible based on additional exclusion criteria • Must have a reviewed CT of the head with Negative for Hemorrhage result. • Lab studies must be reviewed Absolute Exclusions for tPA • Evidence of ICH on CT Scan • Clinical presentation suggestive of a SAH • Active internal bleeding • Intracranial surgery, serious head trauma or previous stroke within 3 months • Any history of ICH, AVM or aneursym • Blood Pressure: If BP can not be controlled after 2 attempts to lower. • Systolic > 185 • Diastolic > 110 • Glucose ≤ 50 per BGM • Known bleeding diathesis including: • Platelet count < 100,000 • On Heparin (within 48 hours) & PTT • INR ≥ 1.7 • Low molecular weight heparin administered in the past 24 hours at therapeutic doses. (Excludes prophylactic doses) Additional Exclusion Criteria 3 hours to 4.5 hours • • • • • This criteria is specific for 3 to 4.5 hours after symptom onset Age > 80 Major neurological deficits with a NIHSS greater than 25 History of stroke AND diabetes Receiving anticoagulant therapy regardless of INR, PT/PTT Cautions and Warnings • Minor symptoms with rapid improvement • Major Neurological deficits (multi-lobar) of the CT > 1/3 of the cerebral hemisphere • Major surgery or trauma (excluding head trauma) within 14 days. • History of frank GI or GU hemorrhage within 21 days • Arterial puncture in a NON-compressible site within 7 days • Acute MI in previous 3 months (non concurrent) • Seizure at onset of stroke symptoms suggestive of postictal neurological impairment Dosing • tPA is based on weight • 0.9mg/kg • Pharmacy requires the weight to properly dose • Maximum dose ANY patient can receive is 90 mg. • Is a 2-part administration process • IV Bolus • 1 hour infusion • Requires multiple safety checks from pharmacy prior to pick up by nursing Administration • 1st part: • 10% of the total dose is administered as IV bolus • The bolus is administered over 1 minute IVP • 2nd part: • Remaining 90% is infused over 60 minutes • Must be administered on IVAC • Vital signs & NIHSS (nursing) every 15 minutes during administration Complications and Side Effects • The most common complication with tPA administration is bleeding. Bleeding is further broken down into two broad categories • Internal: Intracranial, retroperitoneal, or GI, GU and Respiratory tracts • Superficial: invaded or disturbed sites: • venous cut-downs • arterial and venous punctures • catheter insertion sites • needle puncture sites • sites of recent surgical intervention Necessary Precautions • Avoid IM injections • Use extreme caution with veni-punctures; only perform as required • If arterial puncture is needed during infusion or after, utilize upper extremity. Manual compression will be required. • Pressure to be applied for 30 minutes • Pressure dressing to be applied to site • Frequent checks of the puncture site • • • • • Seizure Precautions Bedrest x 24 hours HOB at 30°, place tPA sign above bed NPO until evaluated by Speech Therapy or Neurology SCD’s Post tPA Assessment/Documentation • Vital Signs AND NIHSS (by nurses) • q 15 minutes x 2 hours from start of tPA THEN • q 30 minutes x 6 hours THEN • q hour x 16 hours • Temps q 4 hours x 24 hours • Continuous Pulse Oximetery • Blood glucose (may require tight glycemic control) • Initial • every 6 hours if NPO • AC & HS once patient is eating for 48 hours • notify physician if blood glucose is > 140 Monitoring • Patients who receive tPA need to be closely monitored • The first 24 hours after tPA administration is critical with a risk of hemorrhage • Vital signs will require close monitoring • While the risk is concerning, the benefit outweighs the risk as quality of life is greatly changed. Facts to consider with tPA • tPA does NOT come pre-assembled and mixed • Is very expensive • $3,300 per dose • Requires multiple safety checks prior to administering. • Requires a weight to dose appropriately • Anti-platelet medications and Heparin will not be administered until 24 hours post tPA administration tPA is also time sensitive Special Thanks to the following people who were willing to be photographed: • • • • • • • • • May Alsamarae RPh Kim Babcock RPh Barb Bishop PharmD Melanie Deron, RN Dr. Jason Gumma Paul Hotycki, CPhT Colleen Kargenian, NT Amy Millsaps, RN Amal Sobh PharmD Resources • • • • • • • • • • Disclaimer: NO PHARMACISTS WERE HURT IN MAKING THIS PRESENTATION American Heart Association/American Stroke Association 2010 http://www.strokeassociation.org Garden City Hospital Pharmacy Services Dr. Brian Kim Dr. Anna Pawlak Del Zoppo et. Al. (2009) Expansion of the Time Window for Treatment of Acute Ischemic Stroke with Intravenous Tissue Plasminogen Activator: A Science Advisory From the American Heart Association/American Stroke Association Retrieved Electronically from stroke.ahajournals.org Thomas, Jennifer (2010) Patients Do Better at Hospitals That Follow Stroke Guidelines Chances of survival were higher study shows retrieved electronically from Circulation: Cardiovascular Quality and Outcomes Michigan Stroke Network (2010) Possible IV-rt-PA (Activase) Candidate (Inside a 3-hour window or < 180 minutes from symptom onset) Otwell, J, et. Al. (2010) Efficacy and safety of i.v. alteplase therapy up to 4.5 hours after acute ischemic stroke onset Am J Health Syst Pharm – Vol 67-July 1, 2010 pp 1070-1074 Genentech © (2005) Activase Prescribing Information retrieved electronically from www.activase.com