Use of Subcutaneous IgG in Patients on Concomitant
advertisement

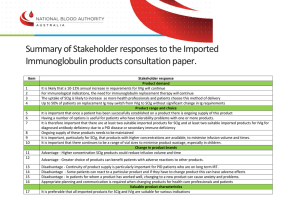
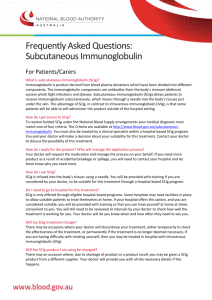
Use of Subcutaneous IgG in Patients on Concomitant Anticoagulant and Antiplatelet Therapy Mark R. Stein,1 Kelly Farnan,1 Danielle Eufrasio,1 Carla Duff, 2 Jerry Hunter,3 Diana Ochoa,4 Marie-Claude Levasseur,5 Loris Aro,6 Annette Zampelli7 1Allergy Associates of the Palm Beaches, North Palm Beach, FL, USA; 2University of South Florida, Tampa, FL, USA; 3Arizona Allergy Associates, Phoenix, AZ, USA; 4Allergy/Immunology Research Center of North Texas, Dallas, TX, USA; 5University Health Center, Sainte-Justine Hospital, Montreal, QC, Canada; 6Toronto Allergy Group, Toronto, ON, Canada; 7CSL Behring, LLC, King of Prussia, PA, USA The International Nursing Group for Immunodeficiencies October 3-6, 2012, Florence, Italy Disclosures and Acknowledgments • MRS has served as a speaker, consultant, and/or investigator for Baxter Healthcare Corp, CSL Behring, Merck, and Teva. CD, JH, MCL, and LA are nurse consultants for CSL Behring. DO is a nurse consultant for CSL Behring and has served on an advisory board for Baxter Healthcare. AZ is employed by CSL Behring. • This presentation was supported by CSL Behring, LLC. • Medical writing and editorial support was provided by Daniel McCallus, PhD, of Complete Publication Solutions, LLC, and was funded by CSL Behring, LLC. Introduction • Primary or Secondary Immunodeficiency Disease (PIDD/SIDD) – Standard treatment: • Intravenous immunoglobulin (IVIG)1 • Subcutaneous immunoglobulin (SCIG)1 • High prevalence of thrombotic risks in the general population2 – Many patients with PIDD/SIDD are also prescribed anticoagulant and antiplatelet (AC/AP) drugs for the treatment and prophylaxis of thrombotic, cardiac, and vascular diseases3 – Some disorders associated with PIDD have congenital cardiovascular manifestations that require AC/AP 1. Fried AJ and Bonilla FA. Clin Microbiol Rev. 2009;22(3):396-414. 2. Heidenreich PA, et al. Circulation. 2011;123(8):933-944. 3. Alexander KP and Peterson ED. Circulation. 2010;121(17):1960-1970. Rationale and Objective • Rationale – Infusion-site bleeding or bruising at the site of SCIG administration due to the activity of AC/AP medication was theoretical concern • Objective – To establish the safety of concomitant SCIG and AC/AP therapy Study Design • Multicenter retrospective chart review of tolerability data • Patient inclusion criteria: – PIDD or SIDD – Receiving treatment with 20% SCIG (Hizentra®, CSL Behring, LLC, King of Prussia, PA) or 16% SCIG (Vivaglobin®, CSL Behring, LLC; no longer available in the United States) – Prescribed concomitant AC/AP medications Patient Descriptions 26 of the total 33 patients were part of a larger (n=47) retrospective single-center study on safety and efficacy of SCIG in the elderly Parameter Patients, n (%) N=47 PIDD diagnosis Hypogammaglobulinemia 29 (61.7) IgG subclass deficiency or specific antibody deficiency 9 (19.1) Hypogamma globulinemia and subclass deficiency or specific antibody deficiency or another immunodeficiency 9 (19.1 Medical history Serious acute bacterial infections 31 (68.1) Chronic infections 44 (93.6) Comorbid conditions Stein et al. Postgrad Med. 2011; 123:186-93. COPD 7 (14.9) Type 1 diabetes 4 (8.5) Type 2 diabetes 3 (6.4) Patient Descriptions Cont. Concomitant medication use in the larger study population Parameter Patients, n (%) N=47 Brochodilators/inhaled corticosteroids 29 (61.7) Proton pump inhibitors 21 (44.7) Statins/antilipidemics 21 (44.7) Nasal sprays 17 (36.2) Antihistamines 16 (34.0) Diuretics/antihypertensives 16 (34.0) Antidepressants 11 (23.4) Bone resorption inhibitors 10 (21.3) Thyroid hormone 9 (19.1) Stein et al. Postgrad Med. 2011; 123:186-93. AC/AP Use: Patient Descriptions • 33 patients total – 26 from larger single-center in elderly, 7 from other centers • Age – Median: 70 years – Range: 3−89 years • AC/AP medications – Included: • Aspirin, warfarin, clopidogrel, and heparin – Used for: • Treatment and/or prophylaxis for thrombotic and vascular diseases – ie, pulmonary embolism, congenital heart disease, chronic atrial fibrillation/flutter Concomitant AC/AP Medications • The most common concomitant medication was aspirin (18/33 patients, 55%) • A large percentage of patients were on warfarin (10/33 patients, 30%) • Few patients used clopidogrel alone or aspirin combined with either clopidogrel or heparin (5/33 patients, 12%) Types of concomitant AC/AP medications in patients treated with SCIG Patient SCIG Administration Parameters • SCIG was administered using a variety of different regimens Mean duration of use, months (range) Mean total dose, mg/kg/month Number of sites per infusion 1 2-3 ≥4 Method of SCIG Administration Syringe Pump Push 22.2 (5−49) 441 3 21 9 30 3 Site of infusion Abdomen Arm Thigh Multiple body areas 24 1 3 5 SCIG administration frequency >1X/week Weekly Every 2 weeks 5 27 1 Results • Local site reactions – Mild, transient, and similar to those previously described4 • Infusion-site bleeding/bruising: observed in only 1 patient – – – – A 62-year-old white male Immune thrombocytopenic purpura and SIDD Receiving aspirin (81 mg/day) SCIG dose of 710 mg/kg per month via syringe push, 20 mL in 1 site (abdomen), 4 times per week – Reported mild bruising during the first month of SCIG treatment 4. Jolles S, et al. Clin Immunol. 2011;141(1):90-120. Case Study 1 • 21-year-old female – 16% SCIG dose of 696 mg/kg per month via syringe push – Concomitant warfarin therapy (5 mg/d) for treatment of prior pulmonary embolism • First SCIG treatment – Two 5 mL push injections (2 hours apart), followed by two 10 mL injections (1 hour apart) – No photo available Before Week 4 Infusion • Subsequent SCIG treatments After – One 20 mL push injection in one site over 15 minutes – 3 times per week • Patient outcomes – No bruising, bleeding, or skin reactions at the infusion site, despite increase in general bruisability since starting warfarin – After 8 months of well-tolerated SCIG, restarted IVIG for personal reasons Week 4 Infusion Case Study 2 • 33-year-old female – 16% SCIG dose of 750 mg/kg per month via syringe push – Concomitant warfarin therapy (alternating 9/10 mg/day) for chronic atrial flutter • First SCIG treatment • Subsequent SCIG treatments • Patient outcomes – No bruising, bleeding, or skin reactions at the infusion site After Before After First SCIG treatment – Two 5 mL push injections (2 hours apart), followed by two 10 mL injections (1 hour apart) – One 20 mL push injection in one site over 15 minutes – 3 times per week Before Week 4 Infusion Conclusions •The concurrent use of AC/AP medications in this group of patients with PIDD or SIDD aged 3-89 years did not increase the occurrence of local site complications after 16% SCIG or 20% SCIG treatment. •In patients with PIDD or SIDD and comorbid cardiovascular or thrombotic disorders treated with AC/AP medications, the use of 16% or 20% SCIG was well tolerated.