Training course on diagnostic upper gastrointestinal endoscopy
advertisement

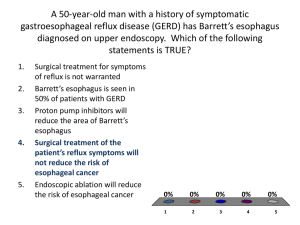
Preliminary training course on diagnostic upper gastrointestinal endoscopy Raika Jamali M.D. Gastroenterologist Sina Hospital Tehran University of Medical Sciences After this course you would be able to • Determine the indications and contraindications of upper gastrointestinal endoscopy (patient selection) • Define the proper time for the procedure • Prepare the patient for the procedure • Handle the endoscopy team • Perform the procedure • Check for the possible complications • Write an endoscopy report Patient selection • Patient with upper gastrointestinal discomfort with the alarming signs: – – – – – Age > 50 Weight loss Anemia Vomiting Family history of upper gastrointestinal malignancy • Those refractory to therapy • Surveillance for Barrett's esophagus • Long standing reflux symptoms Contraindications • Hemodynamic unstable patient that need resuscitation before endoscopy • Hopoxia • Cardiac arrhythmia • Esophageal perforation Precaution • Patients with unstable airway or respiratory failure need tracheal intubation before endoscopy • Check for hypoxia during the procedure and titrate the supplemental oxygen to avoid hypoxia • Patients with massive bleeding with risk of aspiration need tracheal intubation before endoscopy Precaution • Patients with cardiac instability need proper management before endoscopy • Check for arrhythmia during the procedure and terminate the procedure immediately if significant tachy or brady arrhythmias arise • Patients suspected for esophageal perforation (with foreign body swallowing or corrosive esophagitis) need CXR and contrast radiography for detection of possible perforation before endoscopy Timing of endoscopy • Emergent endoscopy is preferred in patients with ongoing (active) severe bleeding – Fresh blood on gastric washing – Orthostatic hypotension in spite of proper resuscitation – Melena perse or coffee ground in gastric washing is not a sign of active bleeding • Elective endoscopy is preferred when no sign of ongoing bleeding exist Preparing the patient • The risks and benefits of the procedure should be offered to the patient and written informed consent should be taken before the procedure • The patient should be examined before the procedure for the evaluation of: – Vital signs – Existence of wheezing in lungs that need bronchodilator before the procedure – Signs of esophageal perforation (pnumothorax and subcutaneous emphysema) Preparing the patient • Check for hypoxia by pulse oximetery • Use supplemental nasal oxygen for patient with O2 saturation < 90% • Check for false teeth or any foreign body in mouth and remove them before the procedure – Secretions in mouth should be suctioned and loose teeth should be removed to reduce the risk of aspiration • Insert appropriate airway device Preparing the patient • Check for the I.V. lines • Position the patient on left lateral decubitus • Sedate the patient with midazolame infusion Checking the endoscopy unit • Check the light source of scope • Perform white balance for getting the optimal light • Check for the air pump for appropriate air insufflation • Check the water tank and appropriate water spray • Check for the power of suction Endoscopy procedure • Check for the locks on endoscope and ensure that the tip of scope can move freely • Lubricate the end of scope with appropriate gel to facilitate the passage of scope through the pharynx • To reduce the risk of aspiration of the gel, the amount of gel should not be too much to suspense from the tip of scope • Do not insert gel near to the end of scope to avoid covering the lens Endoscopy procedure • Insert the scope in the mouth and move it toward the uvula watching the palate • Find the pyriform recess and insert the scope carefully to the esophagus • Do not use the blind approach to reduce the risk of perforation • Move the scope down and air insufflate to open the esophagus Endoscopy procedure • Mention to any mucosal abnormality or strictures and obtain biopsy for the evaluation of malignancy • Identify glycogenic acanthosis and inlet patch that do not have risk of malignancy • Watch for white plaques that indicate candidiasis • The possible web or ring in esophagus should be mentioned • Check for the possible esophageal varices in distal part – Describe the size – Notice to the signs of bleeding tendency (red wale sign) Endoscopy procedure • Observe the Z line in distal esophagus • Pay special attention to the possible mucosal breaks in distal esophagus before entering the stomach, since traumatizing the mucosa by the scope might cause false breaks • Observe for the length of salmon color appearance in distal esophagus • The salmon color appearance in distal esophagus is indicative of columnar epithelium • If the length of salmon color appearing part is > 3 cm, obtain 4 quadrant biopsies from it for the detection of possible Barrett's esophagus Endoscopy procedure • Move the scope upward and right to reach the pylorus • Insufflate air to inflate the stomach and watch for mucosal abnormalities carefully • To observe the cardia and the lesser curvature, retroflex the scope and withdraw the scope to reach the cardia • Check for the hiatal hernia in retroflexion maneuver Endoscopy procedure • Check for any evidence of mucosal edema (snake skin appearance, cobble stoning) in stomach • Check for the erosions and ulcers – Define the location – Define the size – Stigmata of bleeding • Check for submucosal lesions and polyps • Check for any evidence of vascular malformations suspicious as a source of bleeding Endoscopy procedure • It is better to approach from the base of antrum for passing through the pylorus and entering the duodenum • Check the bulb for the signs of duodenitis (snake skin appearance) or ulcer • The scope should move upward and right for reaching to the second part of duodenum • Check for any signs of malabsorption in D2 (scalloping) • Obtain biopsy from any suspicious lesion in D2 for evaluation of malabsorption • If the mucosa seemed normal, Obtain 4 quadrant biopsy for evaluation of malabsorption • Check for Periampullary diverticula • Check for Hemobilia Check for the possible complications • Check for chest pain, diaphoresis, and fatigue after the procedure that might indicate ischemic heart disease • In case of dyspnea, examine the lungs to check for aspiration • Check for chest pain, subcutaneous, emphysema and respiratory distress after the procedure that might indicate perforation Endoscopy report • Report should include: – Patient identification – Date of endoscopy – The reason for endoscopy – Sedation details – Endoscopic findings – Name of the endoscopist and the endoscopy team Endoscopy report • The abnormalities in larynx and vocal cords should be mentioned (vocal cord nodule, laryngitis, vocal cord paralysis) • The description of mucosal, submucosal, vascular abnormalities, and extrinsic compression in the esophagus should be reported. Endoscopy report • The description of mucosal abnormality consists of: – Size – Location – Stigmata of bleeding (active bleeding, cloth, or visible vessel) – Shape (depressed, elevated, or flat) – Causing obstruction (could the scope pass through or not) • An easy way to define the size of lesion, you should compare the size of the lesion with the tip of biopsy forceps • To localize the lesions in esophagus, the distance of the lesion is reported from the incisor teeth Endoscopy report • The description of submucosal abnormality consists of: – Size – Location – Stigmata of bleeding (active bleeding, cloth, or visible vessel) – Causing obstruction (could the scope pass through or not) • The description of extrinsic compression consists of: – Size – Location – Causing obstruction (could the scope pass through or not) Endoscopy report • Vascular abnormalities in esophagus consist of: – – – – Varices Arteriovenous malformation Angiodysplasia Hemangioma • The description of vascular abnormality consists of: – Size – Location – Stigmata of bleeding (active bleeding, clot, or visible vessel) Z line and salmon color appearance mucosa in distal esophagus Submucosal lesion ESOPHAGEAL STRICTURE Endoscopy report • Describe the mucosal breaks in distal esophagus according to “Los angles classification”: – If the mucosal break is < 5 mm (GERD A) – If the mucosal break is > 5 mm (GERD B) – If the mucosal break is > 5 mm and invading more than 75% of the esophageal circumference (GERD C) – If ulcer exists (GERD D) • Describe the length of salmon color appearance part in distal esophagus • Report that biopsy was taken if the length of salmon color appearance part in distal esophagus was > 3 cm GERD GERD A GERD C GERD B GERD D Endoscopy report • Report the size of hiatal hernia: – Small size hiatal hernia exists if there is free space between the scope and esophagogastric junction with inspiration and disappearance of the free space with expiration – Medium size hiatal hernia exists if there is fixed free space between the scope and esophagogastric junction that do not change with respiration – large size hiatal hernia exists if there is fixed free space between the scope and esophagogastric junction that do not change with respiration and the scope can freely enter the esophagus by withdrawing the scope in retroversion maneuver Hiatal hernia Large size hiatal hernia with cameron ulcer Endoscopy report • The description of mucosal, submucosal, vascular abnormalities, and extrinsic compression in the stomach should be reported with the details mentioned previously. • Report the mucosal edema or nodularity in stomach • Check for the erosions and ulcers – Define the location – Define the size – Stigmata of bleeding Nodularity (above) Snake skin appearance (below) Erosions (active bleeding in right and without bleeding in left) Stigmata of rebleeding in ulcer Gastric polyp Gastric tumor Submucosal lesion Submucosal lesion in stomach Angiodysplasia Blue rubber nevus syndrome Varice in fundus Watermelon stomach Hypertrophied gastric folds Endoscopy report • To localize the lesions in stomach you should find the incisura angularis as an important marker. • If the lesions are between the incisura angularis and pylorus they are located in antrum. • If the lesions are above the incisura angularis they are located in body. • The area about 2-3 cm around the esophagogastric junction is cardia. • The fundus is considered as the portion of the stomach that lies above the cardiac notch. Endoscopy report • The description of mucosal, submucosal, vascular abnormalities, and extrinsic compression in the duodenum should be reported with the details mentioned previously. • Report the mucosal edema • Check for the erosions and ulcers – Define the location – Define the size – Stigmata of bleeding Submucoal lesion in second part of duodenum Scalloping in second part of duodenum hemobilia